Abstract
Respiratory tract infections (RTIs) are among the most common illnesses affecting children worldwide, leading to significant morbidity and healthcare utilization. This review article aims to explore the epidemiology, etiology, and clinical manifestations of RTIs in children, focusing on both upper and lower respiratory tract infections. The role of vitamins and home remedies in the prevention and management of these infections is critically examined, highlighting their efficacy, safety, and potential mechanisms of action. Various vitamins, such as vitamin C, vitamin D, and vitamin A, have been studied for their immune-boosting properties and their ability to reduce the incidence and severity of RTIs. Additionally, traditional home remedies, including honey, herbal teas, steam inhalation, and dietary modifications, are evaluated for their therapeutic benefits and limitations. This review synthesizes current research findings, providing evidence-based recommendations for clinicians and caregivers on integrating vitamins and home remedies into the comprehensive management of paediatric RTIs. Future research directions are suggested to further elucidate the role of these complementary approaches in improving respiratory health outcomes in children.
Keywords
Respiratory tract infections, vitamins, home remedies, Paediatric health.
Introduction
Respiratory Tract Infections (RTIs) are among the most common ailments affecting children worldwide, contributing significantly to pediatric morbidity and healthcare burden. RTIs encompass a broad spectrum of conditions, ranging from mild infections such as the common cold to more severe diseases like pneumonia and bronchitis. The high incidence of RTIs in children is attributed to several factors, including immature immune systems, frequent exposure to pathogens, and environmental influences. In recent years, there has been growing interest in exploring the potential role of Vitamin D in the prevention and management of RTIs in children. Vitamin D, known primarily for its role in bone health, also plays a crucial part in modulating the immune system. Several studies have suggested that adequate levels of Vitamin D may reduce the susceptibility to infections, including RTIs. However, the evidence remains mixed, necessitating further exploration into the exact relationship between Vitamin D and respiratory infections in children. Alongside Vitamin D, various home remedies have been traditionally employed to alleviate symptoms and promote recovery in children suffering from RTIs. These remedies, often passed down through generations, include practices such as steam inhalation, honey, herbal teas, and dietary modifications. While some of these remedies are supported by scientific evidence, others lack rigorous validation, leading to ongoing debate about their efficacy and safety. This review aims to critically examine the current literature on the role of Vitamin D and home remedies in the prevention and treatment of RTIs in children. By synthesizing the available evidence, we seek to provide a comprehensive understanding of how these interventions may contribute to reducing the burden of RTIs in pediatric populations.
Respiratory Tract Infection (RTIs):
Respiratory tract infections (RTIs) are a major global health issue, affecting all age groups and causing significant morbidity and mortality. They range from mild to severe conditions and require an understanding of their causes, diagnosis, and management. RTIs are classified into upper (URTIs) and lower respiratory tract infections (LRTIs), with URTIs like the common cold being mostly viral and LRTIs, such as pneumonia, involving bacteria, viruses, or fungi. Viral pathogens like rhinoviruses and influenza are common, while bacterial infections can involve pathogens like Streptococcus pneumoniae. Fungal infections mainly affect immunocompromised individuals. Symptoms vary, with URTIs presenting mild symptoms like a sore throat, while LRTIs cause more severe symptoms like chest pain and shortness of breath. Diagnosis involves clinical assessment and tests like PCR, while treatment depends on the pathogen, using antivirals, antibiotics, or antifungals as needed. Preventive measures include vaccination, hygiene practices, and public health strategies. RTIs impose a significant burden on global health, particularly affecting vulnerable populations. Future research focuses on better vaccines, diagnostics, and antimicrobial stewardship. Addressing RTIs in children is crucial due to their higher susceptibility, especially in low- and middle-income countries. Misuse of antibiotics in RTIs also contributes to antimicrobial resistance, complicating treatment.
Respiratory Tract Infections in Children's:
Respiratory tract infections (RTIs) are a significant global health challenge, impacting individuals of all ages and leading to considerable morbidity and mortality. These infections range from mild, self-limiting conditions to severe, life-threatening diseases, necessitating a comprehensive understanding of their pathophysiology, epidemiology, diagnosis, and management. Respiratory tract infections are among the most common illnesses in children, accounting for significant healthcare visits and hospitalizations. These infections can range from mild upper respiratory infections, like the common cold, to severe lower respiratory tract infections, such as pneumonia and bronchiolitis.
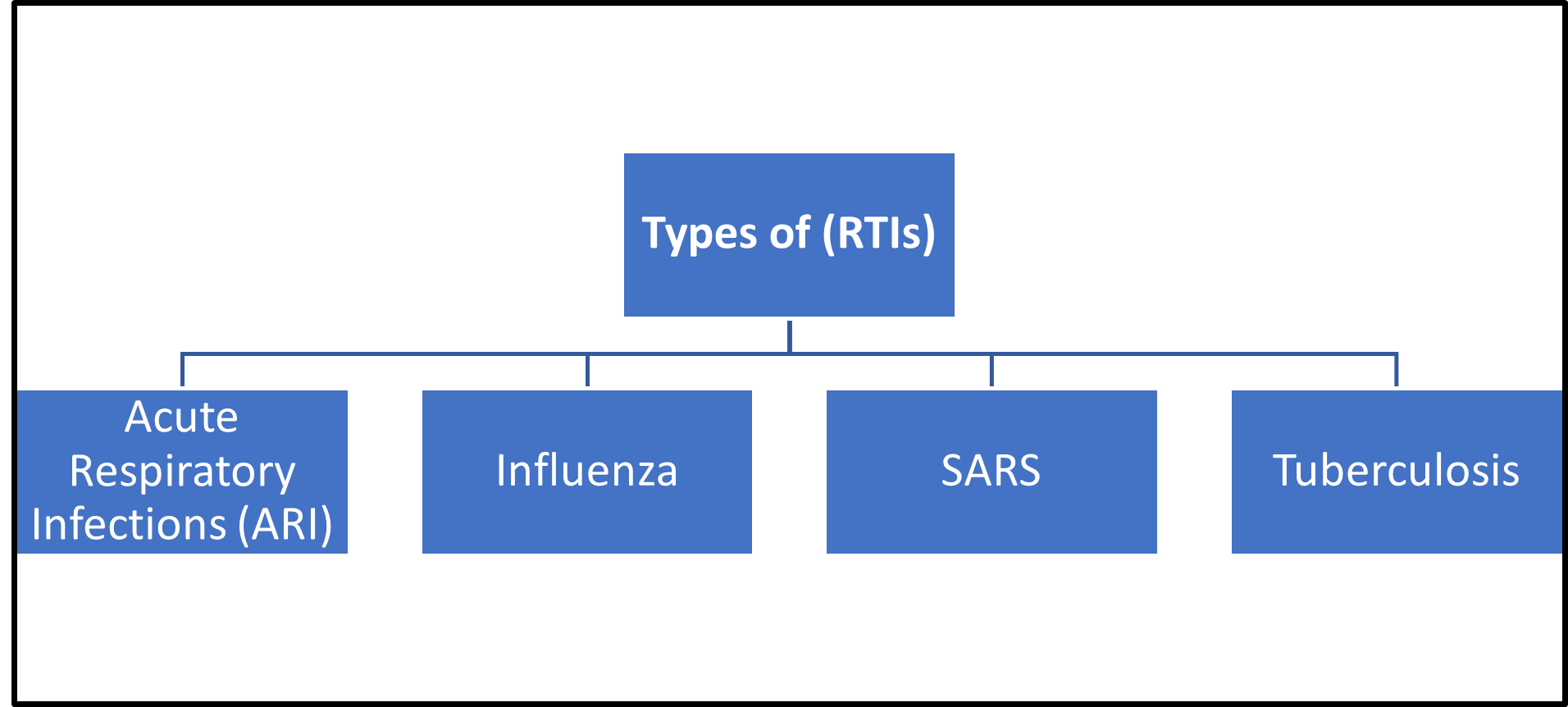
Types of Respiratory Tract Infections (RTIs)
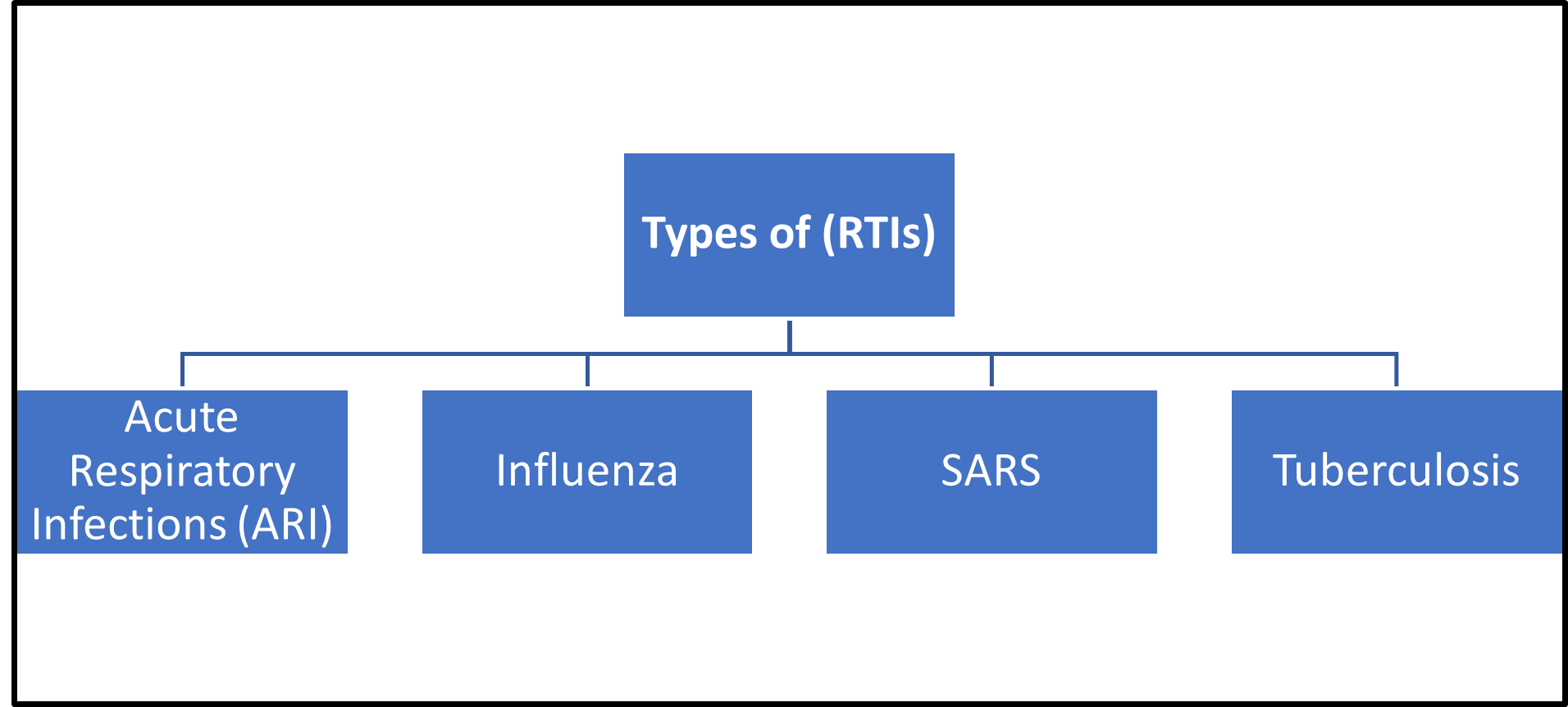
Figure 1: Types of Respiratory Tract Infections
Acute Respiratory Infections (ARI)
Acute respiratory infection indicates infection of any part of the respiratory tract of less than 30 days duration and otitis media of less than 14days duration The infection mainly includes acute episodes of cough, cold, running nose, hoarseness of voice, ear discharge, fast breathing, breathing difficulty and chest indrawing with or without fever.
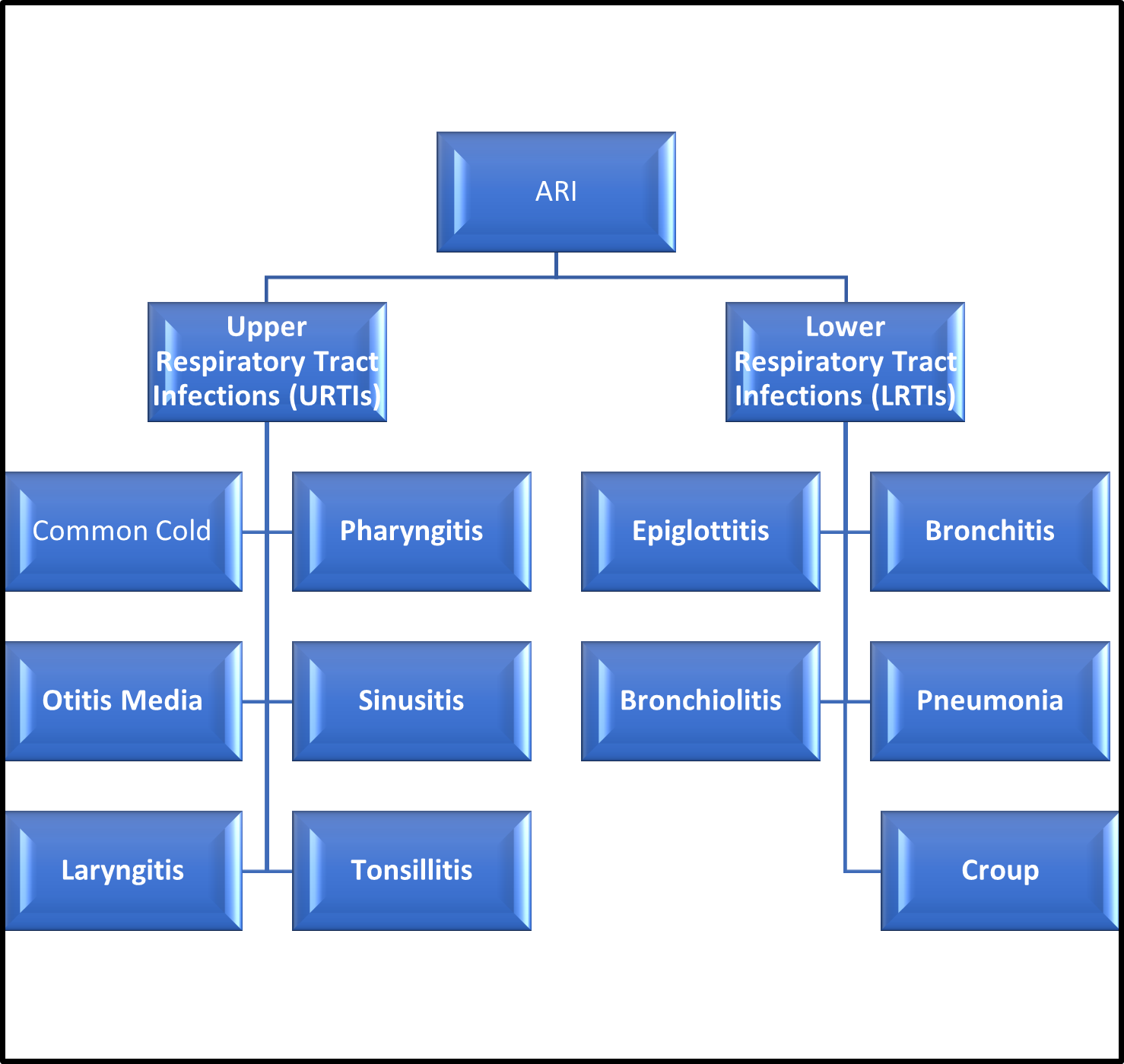
Classification of ARI:
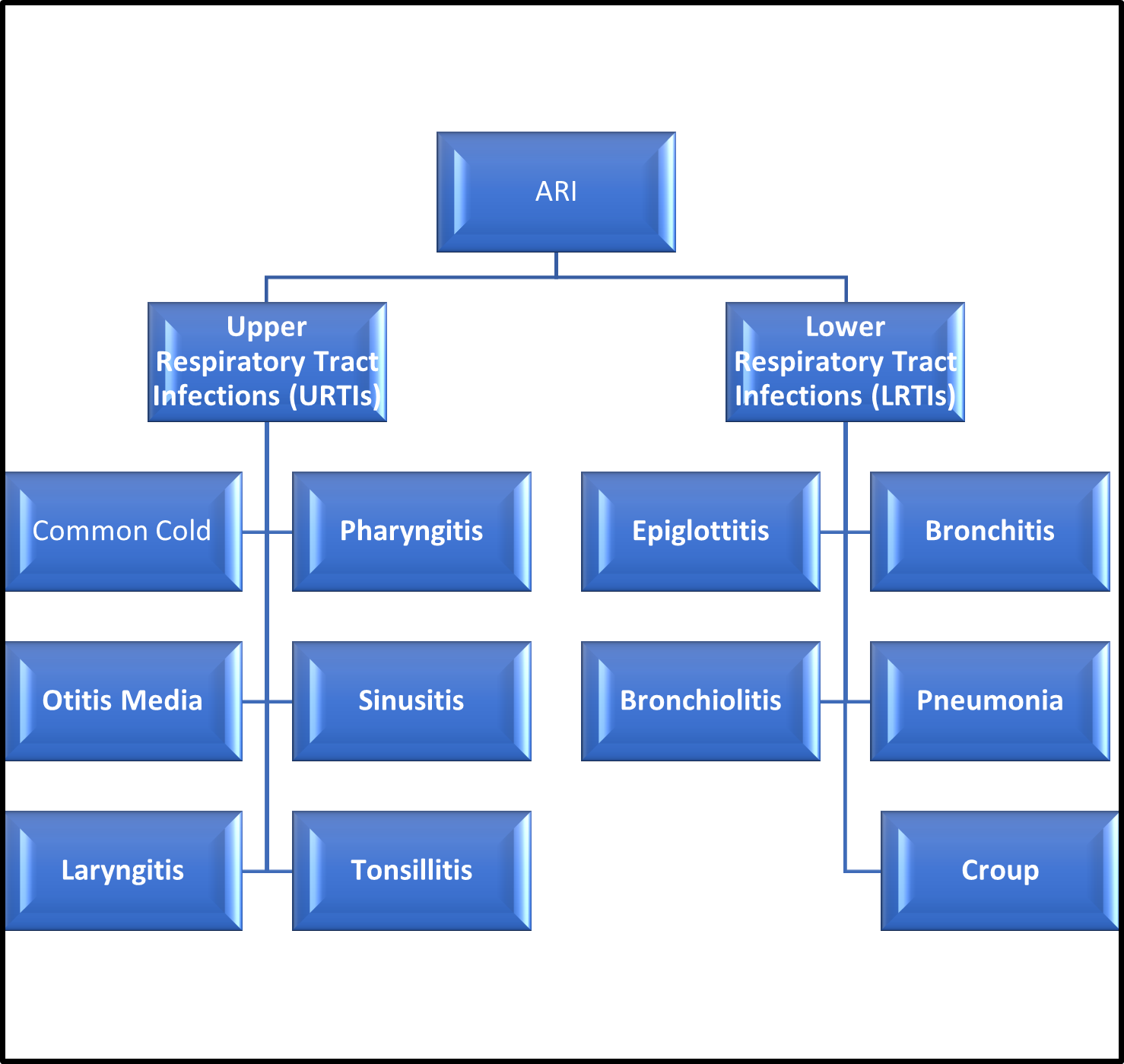
Figure 2: Types of Acute Respiratory Infections
Acute Respiratory Infections (ARI):
Upper Respiratory Tract Infections (URTIs)
1.Common Cold (Viral Rhinitis):
Common cold is a mild upper respiratory tract viral illness. It is generally treated as a self-limited illness that will go away without any treatment. Common is one of the most frequent acute illnesses that is observed in most of the people. In a year a person is affected with cold on an average of 2 or 3 times. It is caused by many types of viruses.
Symptoms:
-
- Sore throat
- Cough
- Congestion
- Sneezing
Diagnosis:
The common cold is usually diagnosed based on symptoms and a physical examination. No specific tests are typically required unless other conditions are suspected.
Treatment:
- Rest and hydration: Adequate rest and plenty of fluids.
- Over-the-counter medications: Pain relievers (e.g., ibuprofen, acetaminophen), decongestants, antihistamines, and cough syrups.
Prevention:
Hand hygiene:
Frequent hand washing with soap and water.
Avoid close contact:
Stay away from people who are sick.
Complications:
Secondary infections:
Sinusitis, ear infections, or bacterial infections.
Exacerbation of chronic conditions:
Asthma or chronic obstructive pulmonary disease (COPD) flare-ups.
2.Pharyngitis:
Pharyngitis is defined as the inflammation of the pharynx. It is simply called as “sore throat”. It mainly causes scratching sensation in the throat and difficulty in swallowing. According to the AOP (American Osteopathic Association) Pharyngitis is the most common reason for visiting doctors. It occurs mostly in colder months of the year.
Symptoms:
- Sore throat
- Pain or difficulty swallowing
- Red and swollen tonsils
- White patches or pus on the tonsils
Diagnosis:
Physical examination:
Checking the throat for redness, swelling, and white patches.
Throat swab:
A rapid antigen detection test (RADT) or throat culture to detect Streptococcus bacteria if a bacterial infection is suspected.
Treatment:
Viral pharyngitis:
- Rest and hydration.
- Pain relievers (e.g., acetaminophen, ibuprofen).
Bacterial pharyngitis:
- Antibiotics (e.g., penicillin, amoxicillin) prescribed by a healthcare provider.
- Follow the full course of antibiotics even if symptoms improve.
Prevention:
Hand hygiene:
Frequent hand washing with soap and water.
Avoid close contact:
Stay away from people who are sick.
Good respiratory hygiene:
Covering mouth and nose when coughing or sneezing.
Complications:
Rheumatic fever:
A serious condition that can affect the heart, joints, nervous system, and skin.
Post-streptococcal glomerulonephritis:
A kidney disease that can occur after a strep throat infection.
Spread of infection:
The infection can spread to other areas, such as the sinuses or middle ear.
3. Otitis Media:
Otitis media, also known as a middle ear infection, is an inflammatory disease that causes swelling, redness, and fluid buildup behind the eardrum. It can be caused by a cold, sore throat, or respiratory infection, and can also be caused by allergies, excess mucus and saliva during teething, infected adenoids, or tobacco smoke.
Symptoms:
- Ear pain
- Fever
- Hearing loss
- Irritability (especially in children)
Diagnosis:
Physical examination:
A doctor uses an otoscope to look inside the ear for signs of infection, such as redness, swelling, and fluid behind the eardrum.
Tympanometry:
A test that measures the movement of the eardrum in response to changes in air pressure, indicating fluid in the middle ear.
Treatment:
Pain management:
Over-the-counter pain relievers (e.g., acetaminophen, ibuprofen).
Warm compresses:
Applying a warm, moist washcloth to the affected ear.
Antibiotics:
Prescribed for bacterial infections or if symptoms are severe or do not improve within a few days. Common antibiotics include amoxicillin.
Prevention:
Vaccinations:
Ensure children receive vaccines such as the pneumococcal and influenza vaccines.
Breastfeeding: Breastfeeding for at least six months can help reduce the risk of ear infections in infants.
Complications:
Hearing loss:
Temporary hearing loss is common, but persistent infections can lead to more significant and long-term hearing impairment.
Speech or developmental delays:
Hearing problems can interfere with speech and language development in children.
4. Sinusitis:
Sinusitis is present when the tissue lining the sinuses become swollen or inflamed. It occurs as the result of an inflammatory reaction or an infection from a virus, bacteria, or fungus.
Symptoms:
Facial pain or pressure:
Especially around the eyes, forehead, and cheeks.
Nasal congestion:
Difficulty breathing through the nose.
Diagnosis:
Physical examination:
A doctor examines the nose, throat, and sinuses for signs of infection.
Nasal endoscopy:
A thin, flexible tube with a light and camera (endoscope) is inserted into the nose to view the sinuses.
Treatment:
Viral sinusitis:
Rest and hydration:
Adequate rest and plenty of fluids.
Nasal decongestants:
Over-the-counter nasal sprays or drops (limit use to a few days).
Bacterial sinusitis:
Antibiotics:
Prescribed if symptoms are severe, persistent, or worsen after an initial improvement. Common antibiotics include amoxicillin.
Corticosteroids:
Nasal or oral steroids to reduce inflammation (e.g., prednisone).
Chronic sinusitis:
Nasal corticosteroids:
Prescription nasal sprays to reduce inflammation (e.g., fluticasone, mometasone).
Oral or injected corticosteroids:
For severe inflammation.
Prevention:
Avoid upper respiratory infections:
Practice good hygiene, such as frequent hand washing and avoiding close contact with sick individuals.
Manage allergies:
Use allergy medications and avoid known allergens.
Complications:
Chronic sinusitis:
Prolonged inflammation and infection of the sinuses.
Asthma exacerbation:
Sinusitis can worsen asthma symptoms.
Meningitis:
Infection can spread to the membranes surrounding the brain and spinal cord.
Orbital cellulitis:
Infection of the tissues around the eyes, which can lead to swelling and vision problems.
5. Laryngitis:
Laryngitis is an inflammation of your voice box (larynx) from overuse, irritation or infection. Inside the larynx are your vocal cords — two folds of mucous membrane covering muscle and cartilage.
Symptoms:
- Hoarseness or loss of voice
- Sore throat
- Dry throat
- Tickling or raw sensation in the throat
Diagnosis:
Physical examination:
A doctor examines the throat and listens to the voice.
Laryngoscopy:
A procedure using a thin, flexible tube with a camera (laryngoscope) to view the vocal cords and larynx.
Treatment:
Viral laryngitis:
Rest the voice: Avoid talking or whispering to allow the vocal cords to heal.
Hydration:
Drink plenty of fluids to keep the throat moist.
Humidifier:
Use a humidifier to add moisture to the air.
Bacterial laryngitis:
Antibiotics:
Prescribed if a bacterial infection is confirmed or strongly suspected.
Chronic laryngitis:
Voice therapy:
Work with a speech-language pathologist to improve vocal techniques and reduce strain on the vocal cords.
Avoid irritants:
Eliminate exposure to smoke, alcohol, and other irritants.
Manage underlying conditions:
Treat conditions like gastroesophageal reflux disease (GERD) and allergies.
Prevention:
Avoid overuse of the voice:
Don't shout, talk loudly, or speak for extended periods without breaks.
Stay hydrated:
Drink plenty of water to keep the throat moist.
Avoid irritants:
Refrain from smoking and limit exposure to secondhand smoke, dust, and pollutants.
Complications:
Chronic laryngitis:
Prolonged inflammation of the larynx, leading to ongoing hoarseness or voice changes.
Vocal cord nodules or polyps:
Benign growths that can develop from prolonged vocal strain or irritation.
6. Tonsillitis:
Tonsillitis is inflammation of the tonsils, two oval-shaped pads of tissue at the back of the throat — one tonsil on each side. Signs and symptoms of tonsillitis include swollen tonsils, sore throat, difficulty swallowing and tender lymph nodes on the sides of the neck.
Symptoms:
- Sore throat
- Red, swollen tonsils
- White or yellow patches on the tonsils
- Difficulty swallowing
- Fever
Diagnosis:
Physical examination:
A doctor examines the throat and tonsils for signs of infection.
Throat swab:
A rapid antigen detection test (RADT) or throat culture to detect Streptococcus bacteria if a bacterial infection is suspected.
Treatment:
Viral tonsillitis:
Rest and hydration:
Plenty of fluids and adequate rest.
Pain relievers:
Over-the-counter medications like acetaminophen or ibuprofen to reduce pain and fever.
Warm salt water gargle: To soothe the throat.
Bacterial tonsillitis:
Antibiotics:
Prescribed if a bacterial infection, such as strep throat, is confirmed. Common antibiotics include penicillin or amoxicillin.
Complete the full course of antibiotics:
Even if symptoms improve.
Chronic or recurrent tonsillitis:
Tonsillectomy:
Surgical removal of the tonsils may be recommended for individuals who experience frequent or severe episodes of tonsillitis.
Prevention:
Hand hygiene:
Wash hands frequently with soap and water.
Avoid close contact:
Stay away from individuals who are sick.
Good respiratory hygiene:
Cover mouth and nose when coughing or sneezing.
Complications:
Peritonsillar abscess:
A collection of pus around the tonsil that can cause severe pain and difficulty swallowing.
Chronic tonsillitis:
Persistent inflammation and infection of the tonsils.
Spread of infection: Infection can spread to surrounding tissues, leading to conditions such as pharyngitis or sinusitis.
Lower Respiratory Tract Infections (LRTIs)
1. Epiglottitis:
Epiglottitis is an inflammatory condition of the epiglottis and/or nearby structures including the arytenoids, aryepiglottic folds, and vallecula. Epiglottitis is a life-threatening infection that causes profound swelling of the upper airways which can lead to asphyxia and respiratory arrest.
Symptoms:
- Severe sore throat
- Difficulty swallowing
- Drooling
- Fever
Diagnosis:
Physical examination: Examination of the throat and neck to assess for signs of swelling and airway obstruction.
X-ray:
To visualize the epiglottis and confirm swelling (though this is done cautiously due to the risk of causing further obstruction).
Fibreoptic laryngoscopy:
A thin, flexible tube with a camera (laryngoscope) is inserted to visualize the epiglottis and surrounding structures.
Treatment:
Emergency management:
Immediate medical attention is crucial as epiglottitis can rapidly progress to airway obstruction.
Hospitalization:
Most cases require hospitalization in an intensive care unit (ICU) for close monitoring and airway management.
Oxygen therapy:
To ensure adequate oxygen levels.
Prevention:
Haemophilus influenzae type B (Hib) vaccination: Routine childhood vaccination against Hib has dramatically reduced the incidence of epiglottitis caused by this bacterium.
Prompt treatment of respiratory infections:
Early diagnosis and treatment of respiratory infections can help prevent complications that may lead to epiglottitis.
Complications:
Airway obstruction:
The most serious complication, requiring urgent intervention to maintain breathing.
Pneumonia:
Infection spreading to the lungs.
Sepsis: Systemic infection that can be life-threatening.
2. Bronchitis:
Bronchitis is a condition that develops when the airways in the lungs, called bronchial tubes, become inflamed and cause coughing, often with mucus production.
Symptoms:
- Cough: Persistent cough that may produce mucus (clear, white, yellowish-gray, or green).
- Fatigue
- Shortness of breath
- Chest discomfort or tightness
- Slight fever and chills
Diagnosis:
Physical examination:
A doctor listens to the lungs with a stethoscope for signs of wheezing or abnormal lung sounds.
Chest X-ray:
To rule out pneumonia and check the condition of the lungs.
Sputum tests:
Analysis of mucus produced from the lungs to check for bacteria or viruses.
Treatment:
Acute bronchitis:
Rest and hydration:
Adequate rest and drinking plenty of fluids.
Pain relievers:
Over-the-counter medications like acetaminophen or ibuprofen to reduce pain and fever.
Cough suppressants:
Used sparingly, as coughing helps clear mucus from the airways.
Chronic bronchitis:
Bronchodilators:
Inhaled medications to open the airways.
Steroids:
Inhaled or oral corticosteroids to reduce inflammation.
Pulmonary rehabilitation:
A program that includes exercise training, education, and breathing techniques.
Prevention:
Avoid smoking:
Do not smoke, and avoid exposure to secondhand smoke.
Vaccinations:
Get vaccinated for influenza and pneumococcal pneumonia.
Hand hygiene:
Wash hands frequently with soap and water.
Avoid lung irritants:
Stay away from pollutants, dust, fumes, and other lung irritants.
Complications:
Pneumonia:
Acute bronchitis can lead to pneumonia, especially in older adults, young children, and individuals with compromised immune systems.
Chronic obstructive pulmonary disease (COPD):
Chronic bronchitis can contribute to the development of COPD, a serious lung disease that includes chronic bronchitis and emphysema.
3. Bronchiolitis:
Bronchiolitis (brong-kee-oh-LYE-tiss) is an infection of the respiratory tract. It happens when tiny airways called bronchioles (BRONG-kee-olz) get infected with a virus. They swell and fill with mucus, which can make breathing hard. Bronchiolitis is more common during the fall and winter months.
Symptoms:
- Runny nose
- Stuffy nose
- Mild cough
- Fever
- Wheezing
Diagnosis:
Physical examination:
A doctor listens to the lungs with a stethoscope for signs of wheezing or abnormal lung sounds.
Pulse oximetry:
A non-invasive test to measure the oxygen level in the blood.
Chest X-ray:
To check for signs of lung inflammation or other conditions.
Treatment:
Supportive care:
The primary approach since bronchiolitis is usually caused by a viral infection.
Hydration:
Ensure adequate fluid intake.
Oxygen therapy
: Provided if blood oxygen levels are low.
Nasal suctioning:
To remove mucus from the nose, especially in infants.
Medications:
Bronchodilators or steroids:
Occasionally used in severe cases, but their effectiveness is limited and they are not routinely recommended.
Antibiotics:
Only if there is a bacterial co-infection, as bronchiolitis is typically viral.
Prevention:
Hand hygiene:
Wash hands frequently with soap and water.
Avoid close contact:
Keep infants and young children away from individuals who are sick.
Clean and disinfect surfaces: Regularly clean toys, doorknobs, and other frequently touched objects.
Breastfeeding: Breastfeed infants to help boost their immune system.
Complications:
Dehydration:
Due to difficulty feeding and poor fluid intake.
Respiratory failure:
Severe cases may require mechanical ventilation.
Secondary bacterial infection:
Such as pneumonia or otitis media.
Long-term respiratory issues:
Increased risk of recurrent wheezing and asthma later in life.
4. Pneumonia:
Pneumonia is an infection that inflames the air sacs in one or both lungs, causing them to fill with fluid or pus. This can make breathing painful and limit oxygen intake.
Symptoms:
Cough:
Often produces phlegm (may be green, yellow, or bloody).
Fever:
High fever, sweating, and chills.
Shortness of breath:
Rapid breathing and difficulty breathing deeply.
Chest pain:
Sharp or stabbing pain that worsens with deep breaths or coughing.
Diagnosis:
Physical examination:
A doctor listens to the lungs with a stethoscope for abnormal breath sounds (crackles or wheezes).
Chest X-ray:
To confirm the presence of infection and determine the extent and location of lung involvement.
Blood tests:
To check for elevated white blood cell count (indicating infection) and other markers of inflammation.
Treatment:
Antibiotics:
Prescribed based on the suspected or identified cause of pneumonia (bacterial, viral, fungal). Common antibiotics include amoxicillin, azithromycin, or levofloxacin.
Antiviral medications:
If pneumonia is caused by influenza virus (especially during flu season).
Fluids:
IV fluids may be given to prevent dehydration, especially if there is difficulty in drinking enough fluids.
Prevention:
Vaccination:
Getting vaccinated against influenza (flu) and pneumococcal pneumonia can prevent pneumonia caused by these bacteria and viruses.
Hand hygiene:
Washing hands frequently with soap and water, especially before eating and after coughing or sneezing.
Avoid smoking:
Smoking damages the lungs and increases the risk of respiratory infections.
Complications:
Respiratory failure:
In severe cases, pneumonia can lead to respiratory failure, requiring mechanical ventilation.
Sepsis:
Infection spreading through the bloodstream, potentially leading to organ failure.
Lung abscess:
Collection of pus within the lung tissue.
5. Croup:
Croup is a common respiratory illness of the trachea, larynx, and bronchi that can lead to inspiratory stridor and barking cough. The parainfluenza virus typically causes croup, but a bacterial infection can also cause it.
Symptoms:
Barking cough:
A distinctive cough that sounds like a seal or barking.
Hoarseness:
Changes in voice due to swelling of the vocal cords.
Stridor:
A high-pitched sound when breathing in.
Difficulty breathing:
Rapid breathing or labored breathing.
Fever:
Often mild, but can be present.
Diagnosis:
Physical examination:
A doctor can often diagnose croup based on the characteristic barking cough and other symptoms.
Evaluation of breathing:
Listening for stridor and observing the child's breathing patterns.
Chest X-ray:
Sometimes done to rule out other causes if the diagnosis is uncertain.
Treatment:
Home care for mild cases:
Humidified air:
Use a cool mist humidifier or take the child into a steamy bathroom to help ease breathing.
Fluids:
Ensure the child drinks plenty of fluids to prevent dehydration.
Comfort measures:
Provide comfort and reassurance to calm the child during coughing episodes.
Medical treatment for moderate to severe cases:
Corticosteroids:
Oral or inhaled steroids to reduce airway inflammation.
Oxygen therapy:
Administered if the child has low oxygen levels.
Hospitalization:
In severe cases or if the child is struggling to breathe, hospitalization may be necessary for close monitoring and treatment.
Prevention:
Hand hygiene:
Wash hands frequently with soap and water to prevent the spread of viruses that can cause croup.
Avoid exposure:
Limit contact with individuals who have respiratory infections, especially during peak croup season (fall and early winter).
Vaccinations:
Maintain up-to-date vaccinations, including the measles-mumps-rubella (MMR) vaccine, which protects against some viruses associated with croup.
Complications:
Respiratory distress:
Severe cases of croup can lead to difficulty breathing and respiratory distress.
Obstructive breathing:
Inflammation and swelling of the airway may obstruct airflow, requiring immediate medical intervention.
Recurrent croup:
Some children may experience recurrent episodes of croup, especially if they are prone to respiratory infections or have underlying conditions that affect airway function.
Influenza (FLU):
Flu is a contagious respiratory illness caused by influenza viruses that infect the nose, throat, and sometimes the lungs. It can cause mild to severe illness, and at times can lead to death. The best way to prevent flu is by getting a flu vaccine each year.
Symptoms:
Fever:
Often high, usually above 100.4°F (38°C).
Cough:
Dry or productive (producing mucus).
Sore throat
Runny or stuffy nose
Diagnosis:
Clinical assessment:
Based on symptoms and physical examination by a healthcare provider.
Rapid influenza diagnostic tests (RIDTs): Swabbing the nose or throat to detect influenza virus antigens. Results are available within 15-30 minutes.
Reverse transcription-polymerase chain reaction (RT-PCR) test:
More sensitive than RIDTs and can identify specific strains of influenza virus. Results may take longer (several hours to days).
Treatment:
Antiviral medications:
Recommended for individuals at high risk of complications or severe illness,
such as:
- Oseltamivir (Tamiflu)
- Zanamivir (Relenza)
- Peramivir (Rapivab)
Prevention:
Annual influenza vaccination: Recommended for everyone 6 months of age and older.
Hand hygiene:
Wash hands frequently with soap and water, or use alcohol-based hand sanitizer.
Respiratory hygiene:
Cover your mouth and nose with a tissue when coughing or sneezing, and dispose of tissues properly.
Complications:
Pneumonia:
Bacterial or viral pneumonia can develop as a complication of influenza.
Bronchitis:
Inflammation of the bronchial tubes.
Sinus infections:
Infection of the sinuses.
Ear infections:
Especially in children.
Exacerbation of chronic conditions:
Influenza can worsen pre-existing medical conditions like asthma, diabetes, or heart disease.
SARs:
Severe acute respiratory syndrome (SARS) is a respiratory illness caused by a virus. The illness usually begins with a high fever. Patients also may have chills or other symptoms, including headache, general feeling of discomfort, body aches and diarrhoea.
Symptoms:
Fever:
Often high, above 100.4°F (38°C).
Chills and body aches:
Severe muscle pain and general discomfort.
Cough:
Initially dry and non-productive, progressing to a productive cough with mucus.
Difficulty breathing:
Shortness of breath and rapid breathing.
Sore throat:
Irritation or pain in the throat.
Diagnosis:
Clinical evaluation:
Based on symptoms and travel history to affected areas.
Laboratory tests:
Real-time polymerase chain reaction (RT-PCR) tests to detect SARS-CoV, the virus causing SARS, in respiratory samples.
Imaging:
Chest X-ray or CT scan may show characteristic changes in the lungs, such as pneumonia or acute respiratory distress syndrome (ARDS).
Treatment:
Supportive care:
Includes rest, fluids, and medications to relieve symptoms.
Antiviral therapy:
Drugs such as ribavirin and corticosteroids may be used, although their effectiveness is debated.
Oxygen therapy:
Provided if oxygen levels are low.
Mechanical ventilation:
For severe cases of respiratory distress.
Prevention:
Hand hygiene:
Regularly wash hands with soap and water or use alcohol-based hand sanitizers.
Respiratory hygiene:
Cover mouth and nose when coughing or sneezing, and dispose of tissues promptly.
Avoid close contact:
Especially with individuals showing symptoms of respiratory illness.
Travel precautions:
Follow travel advisories and avoid visiting areas with known outbreaks.
Complications:
Respiratory failure:
Severe cases can progress rapidly to acute respiratory distress syndrome (ARDS) and require intensive care.
Organ failure:
Due to systemic effects of the infection.
Long-term effects:
Some individuals may experience persistent symptoms or complications affecting multiple organs.
Tuberculosis (TB):
Tuberculosis (TB) is an infectious disease that most often affects the lungs and is caused by a type of bacteria. It spreads through the air when infected people cough, sneeze or spit. Tuberculosis is preventable and curable. About a quarter of the global population is estimated to have been infected with TB bacteria.
Symptoms:
Chronic cough:
Lasting more than three weeks, sometimes with bloody sputum.
Chest pain:
Pain or discomfort in the chest.
Coughing up blood
Hemoptysis, or blood in the sputum.
Weight loss:
Unintentional weight loss and loss of appetite.
Fever:
Low-grade fever, usually in the afternoon or evening.
Diagnosis:
Tuberculin skin test (TST) or Mantoux test:
A small amount of PPD tuberculin is injected under the skin of the forearm. After 48 to 72 hours, a healthcare professional will check for a raised, hard area or swelling at the injection site.
Blood tests:
Such as interferon-gamma release assays (IGRAs) like QuantiFERON-TB Gold or T-SPOT.TB, which detect the immune response to TB bacteria.
Treatment:
Antibiotic therapy:
Typically involves a combination of antibiotics taken for at least six months to effectively kill the TB bacteria and prevent the development of antibiotic resistance. Common medications include:
- Isoniazid (INH)
- Rifampin (RIF)
- Ethambutol (EMB)
- Pyrazinamide (PZA)
- Directly Observed Therapy (DOT):
Ensures that patients take their medications as prescribed, which is crucial for preventing drug resistance.
Surgery:
In some cases, surgery may be necessary to remove infected tissue or drain fluid-filled cavities in the lungs.
Prevention:
Vaccination:
The Bacillus Calmette-Guérin (BCG) vaccine is used in many countries to prevent severe forms of TB in children.
Screening and early detection:
Especially for individuals at higher risk of TB infection, such as healthcare workers and those with HIV/AIDS.
Infection control measures:
In healthcare settings to prevent the spread of TB from patients with active disease.
Complications:
Drug-resistant TB: Due to incomplete or improper treatment, TB bacteria can become resistant to antibiotics, making treatment more difficult and sometimes less effective.
Spread of infection:
Without proper treatment and infection control measures, TB can spread from the lungs to other parts of the body, such as the kidneys, spine, or brain.
Organ damage:
Severe cases of TB can lead to organ damage, including lung damage and kidney failure. TB remains a significant global health concern, but with early diagnosis, appropriate treatment, and preventive measures, its impact can be reduced.
VITAMIN D
INTRODUCTION:
Respiratory tract infections (RTIs) are a leading cause of morbidity and mortality in children worldwide, significantly impacting healthcare systems and quality of life. Among the various preventive and therapeutic strategies explored, the role of vitamin D has garnered substantial attention. Vitamin D, traditionally known for its critical role in bone metabolism and calcium homeostasis, is now recognized for its immunomodulatory effects, which may influence susceptibility to infections, including those affecting the respiratory tract. The potential connection between vitamin D and respiratory health in children is supported by a growing body of evidence indicating that vitamin D deficiency is prevalent among pediatric populations and may correlate with an increased incidence and severity of RTIs. The immunomodulatory functions of vitamin D, including the enhancement of innate immune responses and modulation of adaptive immunity, suggest a plausible mechanism by which adequate vitamin D levels could confer protection against respiratory pathogens. Vitamins are essential nutrients that play crucial roles in maintaining overall health, including respiratory health. They contribute to the proper functioning of the immune system, protect against oxidative stress, and help maintain the structural integrity of respiratory tissues. This guide provides an overview of key vitamins that influence respiratory health, their mechanisms of action, and the impact of deficiencies on respiratory tract infections (RTIs).
Vitamin D as an Immune System Regulator:
Vitamin D has an important influence on the host’s immune system, modulating both innate and adaptive immunity and regulating the inflammatory cascade. The hypothesis of the immunoregulatory role of vitamin D derives from the discovery that there are several interactions between vitamin D and the immune system. The majority of immune cells express VDRs, mainly after they themselves have been stimulated. The mechanism by which vitamin D regulates inflammation and immunity appears to be pleiotropic; it controls macrophage and dendritic cell activities and various Toll-like receptormediated events in neutrophils, and it diminishes the function of human dendritic cells by decreasing maturation, antigen presentation and the production of cytokines such as interleukin (IL)-12 and IL-23. Moreover, treating macrophages with 1,25(OH)D results in the expression of various cytokines and chemokines, including CXCL8, IL-6, and IL-12, and tumor necrosis factor (TNF)-? . Additionally, vitamin D induces the expression of two antimicrobial peptides—cathelicidin and ?-defensin—that are widely expressed in the body and play a key role in innate immunity owing to their chemotactic action and toxin neutralization. Vitamin D shifts cytokine expression from a type-1 to a type-2.
Vitamin D and respiratory infections in children:
In children, infections are a major cause of morbidity and mortality. Numerous studies have identified an association between inadequate vitamin D concentrations and RTIs in children. Initially, an association between vitamin D deficiency and RTIs in children was found after a higher incidence of respiratory infections was found among infants and children with rickets. The increased incidence of RTIs in these children was probably caused by both compromised lung compliance due to the rib deformities associated with severe rickets and poor nutritional status. Later, the prototypical example of a connection between vitamin D insufficiency and susceptibility to infectious disease was found to be TB; studies published over the past twenty years have noted the link between decreased serum calcitriol concentrations and increased severity and/or susceptibility to TB infection. Gradually, other RTIs in children have also been linked to vitamin D. The evidence that the peak of viral infections is in the winter months when synthesis of vitamin D across the skin is naturally impaired supported the association. In addition, vitamin D deficiency in pregnant women may result in an increased risk of RTIs in their infants. It has been shown that serum 25(OH)D levels during pregnancy can condition the expression of certain tolerogenic genes connected with diseases other than congenital rickets. Thus, vitamin D supplementation during pregnancy appears to have a beneficial effect on children’s health.
Vitamin D supplementation:
Available data support a role for vitamin D deficiency in the risk of pediatric TB, rAOM and severe bronchiolitis, whereas further studies are needed to confirm an association in children with recurrent pharyngotonsillitis, ARS and CAP. Maintenance of adequate vitamin D status could be an effective and inexpensive prophylactic method against these RTIs, but the supplementation regimen has not been clearly defined. In addition to the lack of consensus on whether and in whom there is a need of vitamin D supplementation as well as on the ideal regimen, countries may have different recommendations according to the characteristics of their population. A clarification of the functional effect of VDRs polymorphisms also in relation to ethnicity, sun exposure, skin characteristics, and fat absorption may influence the recommended regimen. At the moment, the supplementation schemes associated with a successful outcome are those which evaluated cholecalciferol 1000 IU daily for 8 weeks in children treated for TB and 1000 IU daily for 4 months in those with a history of rAOM, whereas no benefit was associated with a single high dose of cholecalciferol (100,000 IU) or with a shortterm oral supplementation (1000–2000 UI daily for 5 days) in children with CAP. Another approach could be the maternal vitamin D supplementation during pregnancy in order to reduce the future RTIs risk in the offspring, but again the ideal supplementation regimen has not been defined. For this reason, well-defined evidence-based guidelines on the serum 25(OH)D levels associated with disease risk and recommended supplementation regimens are urgently needed.
Sources:
Sunlight exposure, fatty fish (e.g., salmon, mackerel, sardines), fortified dairy products, and supplements.
Uses:
Plays a crucial role in modulating the immune system, reducing the risk of infections such as tuberculosis and viral respiratory infections. Enhances the production of antimicrobial peptides in the respiratory epithelium. May help in reducing inflammation in the airways and improving lung function.
Mechanisms:
Immune System Modulation:
Vitamin D modulates both the innate and adaptive immune systems. It enhances the pathogen-fighting effects of monocytes and macrophages (white blood cells) and decreases inflammation.
Antimicrobial Peptide Production:
Stimulates the production of antimicrobial peptides such as cathelicidin and defensins, which have broad-spectrum antibacterial, antiviral, and antifungal properties.
Inflammation Reduction:
Reduces the production of pro-inflammatory cytokines and increases the production of anti-inflammatory cytokines, helping to control excessive inflammatory responses that can damage lung tissue.
Tablets and capsules:
Types of Infections:
Influenza, pneumonia, and other severe respiratory infections.
Forms:
Often available as vitamin D3 capsules or softgels.
Dosage:
Dosage may vary widely based on individual needs and deficiency levels, often prescribed in doses ranging from 1000 IU to 5000 IU daily.
Mechanism:
Modulates the immune response, enhances production of antimicrobial peptides, and reduces inflammation, crucial for managing severe respiratory infections.
Home Remedies for Respiratory Tract Infections:
Respiratory tract infections (RTIs) are common in children, causing discomfort, school absenteeism, and frequent medical visits. While antibiotics and antivirals are essential for severe cases, many parents also use home remedies to ease symptoms. These traditional treatments, like honey, herbal teas, steam inhalation, and saline drops, are popular for their perceived safety, low cost, and minimal side effects. However, scientific evidence supporting their effectiveness varies, highlighting the need for critical evaluation to offer evidence-based advice to parents and healthcare providers. Examples of such remedies are provided below:
1. Steam Inhalation:
Usage:
Inhaling steam to relieve nasal congestion and clear mucus.
Scientific Evidence:
Some studies suggest steam inhalation can provide symptomatic relief for nasal congestion and sinusitis by moisturizing the nasal passages. However, the evidence is mixed, and some studies indicate limited benefits.
Safety for Paediatrics:
Should be used with caution to avoid burns. Adult supervision is necessary. Recommended to use cool mist humidifiers for younger children.
2. Honey:
Usage:
Used to soothe sore throats and suppress coughs.
Scientific Evidence:
Studies have shown that honey can be more effective than over-the-counter cough medications in reducing the frequency and severity of cough in children. It also has antimicrobial properties.
Safety for Pediatrics:
Not recommended for children under one year old due to the risk of botulism.
3. Hydration:
Usage:
Maintaining adequate fluid intake to help thin mucus and prevent dehydration.
Scientific Evidence:
Adequate hydration is supported by health guidelines to help maintain mucus membrane function and ease symptoms of RTIs.
Safety for Pediatrics:
Safe and highly recommended. Ensure children drink plenty of water, broth, and other clear fluids.
4. Saline Nasal Drops:
Usage:
Using saline drops to moisten nasal passages and clear mucus.
Scientific Evidence:
Clinical studies support saline nasal irrigation as an effective method to reduce nasal congestion and improve nasal hygiene.
Safety for Pediatrics:
Safe for all ages, including infants. Use a bulb syringe for gentle application.
5. Ginger Tea:
Usage:
Drinking ginger tea to reduce inflammation and soothe throat irritation.
Scientific Evidence:
Ginger has anti-inflammatory and antioxidant properties that can help alleviate symptoms of RTIs. However, more clinical research is needed to confirm its effectiveness.
Safety for Pediatrics:
Generally safe in moderate amounts. Monitor for any allergic reactions.
CONCLUSION:
Respiratory tract infections (RTIs) in children are a significant public health concern due to their high prevalence and potential complications. Preventive and therapeutic measures are essential. Vitamin D, known for its immunomodulatory effects, may reduce the incidence and severity of RTIs, emphasizing the importance of adequate intake through diet, supplementation, or sun exposure. In addition to medical treatments, home remedies like honey, ginger, turmeric, and saline nasal irrigation can alleviate RTI symptoms, but should complement, not replace, conventional treatments. Consulting healthcare professionals before using these remedies is crucial. Integrating vitamin D and appropriate home remedies may enhance outcomes for children with RTIs. Further research is needed to establish standardized guidelines for these interventions. A holistic approach combining preventive, medical, and supportive strategies can better protect children's health and well-being.
REFERENCES:
- Martineau, A. R., Jolliffe, D. A., Hooper, R. L., Greenberg, L., Aloia, J. F., Bergman, P., ... & Griffiths, C. J. (2017). BMJ, 356, i6583.
- Pereira, M., Dantas Damascena, A. D., Galvão Azevedo, L. M., de Almeida Oliveira, T., & da Mota Santana, J. (2020). Advances in Nutrition, 11(5), 1155-1165.
- Bergman, P., Lindh, Å. U., Björkhem-Bergman, L., & Lindh, J. D. (2013). PLoS One, 8(6), e65835.
- Charan, J., Goyal, J. P., Saxena, D., & Yadav, P. (2012). Journal of Global Infectious Diseases, 4(1), 8-14.
- Cannell, J. J., Vieth, R., Umhau, J. C., Holick, M. F., Grant, W. B., Madronich, S., ... & Giovannucci, E. (2006). The FASEB Journal, 20(6), 1068-1080.
- Chowdhury, R., Taneja, S., Bhandari, N., Kvestad, I., Strand, T. A., & Bhan, M. K. (2016). Paediatrics and International Child Health, 36(1), 30-40.
- Karras, S. N., Fakhoury, H., Muscogiuri, G., Grant, W. B., van den Ouweland, J., Colao, A., ... & Gakidis, N. (2016). Nutrition Research Reviews, 29(1), 37-48.
- Mamani, M., Mucaj, S., & Ghandi, K. (2020). Clinical Respiratory Journal, 14(1),
- 3-12.
- Aghajafari, F., Field, C. J., Kaplan, B. J., Rabi, D. M., Maggiore, J. A., & O'Beirne, M. (2013). Pediatric Infectious Disease Journal, 32(5), 456-460.
- Prentice, A., Williams, A., & Schoenmakers, I. (2021). Journal of Clinical Medicine, 10(4), 766.
- Sinha, A., Sazawal, S., Kumar, R., & Black, R. E. (2015). Journal of Tropical Pediatrics, 61(3), 167-177.
- Kligler, B., & Cohrssen, A. (2008). American Family Physician, 77(4), 517-522.
- Goldman, R. D., & Vohra, S. (2011). Canadian Family Physician, 57(1), 109-111.
- Shi, L. L., Xie, J. P., Du, X. J., Liu, Y. T., Shi, L., & Xu, Y. (2020). Journal of Traditional Chinese Medicine, 40(2), 367-376.
- Lochner, C., & DeJong, S. R. (2006). Journal of Community Health, 31(1), 1-7.
- Oduwole, O., Meremikwu, M. M., Oyo-Ita, A., & Udoh, E. E. (2014). Cochrane Database of Systematic Reviews, 4(1), CD007094.
- Kemper, K. J., & Kathi, J. (1999). Pediatrics, 103(Supplement E1), 1172-1175.
- Lissiman, E., Bhasale, A. L., & Cohen, M. (2014). Cochrane Database of Systematic Reviews, 6(1), CD006206.
- Marx, W., McKavanagh, D., McCarthy, A. L., Bird, R., Ried, K., Delaney, G. P., & Isenring, E. (2015). Journal of Human Nutrition and Dietetics, 28(1), 86-96.


 P. SRI RAMCHARAN *
P. SRI RAMCHARAN *
 10.5281/zenodo.13787075
10.5281/zenodo.13787075