Vitiligo is a challenging autoimmune disorder characterized by the selective destruction of melanocytes, resulting in depigmented patches on the skin, mucous membranes, and occasionally hair. Its etiology involves a complex interplay of humoral and cell-mediated immune responses, with interleukin (IL)-17-mediated pathways and the interferon (IFN)-?/CXCL10 axis playing pivotal roles. Various morphological subtypes such as trichrome, quadri-chrome, and inflammatory vitiligo add to its clinical diversity. While not sex-linked, familial predisposition is observed in a significant portion of patients. Current treatment modalities including topical steroids, phototherapy, and photochemotherapy focus primarily on symptom management and halting disease progression, albeit with limited efficacy and satisfaction levels. Emerging therapies such as excimer laser and topical calcipotriol offer promising alternatives. Corticosteroids and pimecrolimus are commonly employed to modulate immune responses and reduce inflammation, aiming to promote repigmentation. However, despite advancements, effective management of vitiligo remains a substantial challenge for dermatologists. Future research endeavors should target unraveling its complex pathogenesis to develop innovative, targeted therapies that address the underlying mechanisms and improve patient outcomes.
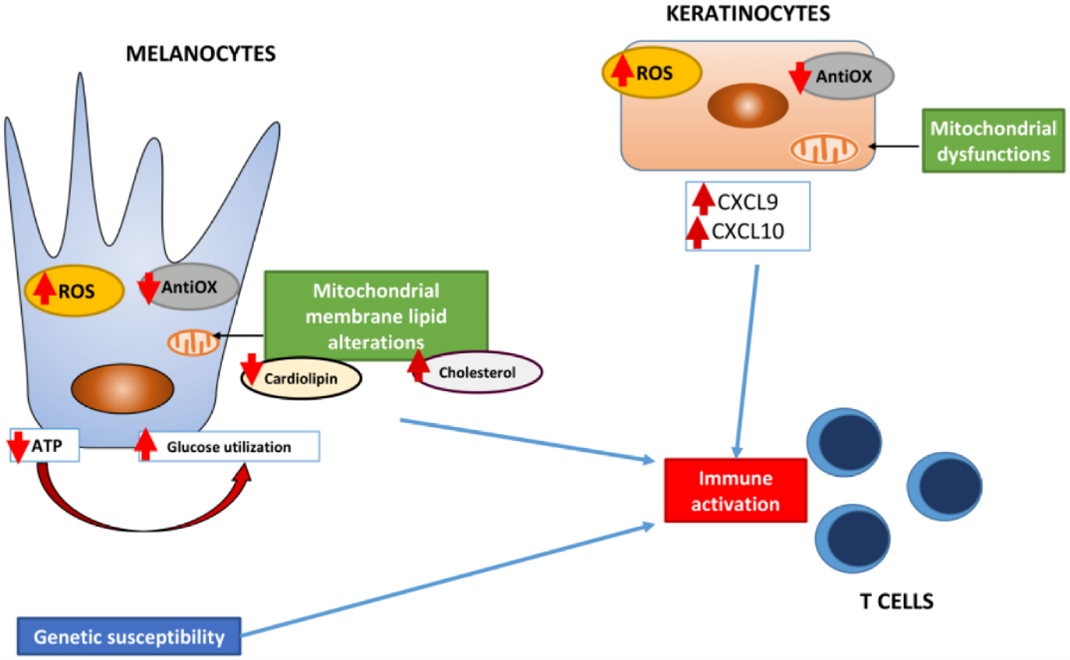
Alternative concepts include:
- Oxidative stress, specifically from hydrogen peroxide, in the setting of reduced cellular defense mechanisms.
- Inherent functional defect of melanocytes.
- Reduction of melanocytes due to dysregulation of their survival and apoptosis
- Toxicity from neurochemical transmitters.
Viruses (e.g., CMV). vitiligo patients and their relatives are at increased risk of other autoimmune diseases, including autoimmune thyroiditis, type 1 diabetes mellitus, pernicious anemia and Addison's disease, suggesting that vitiligo is also an autoimmune disease. These early observations were later confirmed by genome wide association (GWA) studies, which found that many common genetic variations in vitiligo patients encode congenital (NLRP1, IFIH1, casp7, c1qtnf6, trif) and adaptive immune system components (FOXP3, BACH2, CD80, CCR6, PTPN22, IL2R, alpha GZMB, HLA class I and II). [2,4,5,6,7,8,9]
Etiology
The etiology is unknown, but various theories shed light on its potential origins:
- Auto immunity:
Vitiligo is often associated with other autoimmune diseases like thyroiditis and type 1 diabetes. This suggests a possible role of immune system in attacking melanocytes, the cells responsible for producing pigments.
- Cytotoxicity:
Metabolites formed during melanin synthesis may potentially harm melanocytes, leading to their destruction.
- Neutral:
Chemical mediators released at nerve endings might either directly destroy melanocytes or inhibit melanin production.
- Free radicals:
Excess free radicals in the body could be toxic to melanocytes, contributing to their demise.
- Convergent:
It’s possible that a combination of these factors, such as autoimmunity, cytotoxicity, neutral factors, and free radicals, collectively contributes to the development of vitiligo.
- Genetics:
Certain genes, like NALP1, have been implicated in making individuals more susceptible to vitiligo. However, the specific mechanisms controlled by these genes are still unclear.
- Triggering:
While genetics may predispose someone to vitiligo, external triggers such as stress, thyroid dysfunction, skin injury, severe sunburns, chemicals and certain medication may initiate or exacerbate the condition in susceptible individuals.
- Immune System Involvement:
the immune system likely plays a significant role in the destruction of pigments cells, supporting the classification of vitiligo as an autoimmune disease. Vitiligo is a complex condition with multiple potential causes, including genetics predisposition, autoimmune reactions, environmental triggers, and immune system dysfunction. However, further research is needed to fully understand the interplay of these factors in the development and progression of vitiligo. [2,5]
Epidemiology:
It's interesting to note the prevalence of vitiligo across different demographics. The distribution between urban and rural areas could suggest potential environmental factors at play, although genetic predisposition is also a significant factor in vitiligo. The equal frequency across global regions and ethnic groups suggests a universal aspect to its occurrence, although there may be variations in how it presents or is perceived culturally. affecting 0.5- 2 percent of the global population in both adults and children.

The distribution of vitiligo among the patients was 53.2% in males (n=74) and 46.8% in females (n=65). Among the total 139 patients 89 (64%) were from urban areas and the remaining 50 (36%) were from rural areas. The Mean ± SD age of the patients was 25.06 ± 17.6 years. Treating vitiligo, especially during its active progressive stage, is indeed challenging, often requiring a combination of approaches including topical treatments, phototherapy, and sometimes surgical interventions. [2,4,5]
Types of Vitiligo
There are three major types of vitiligo are as follows:
Segmental vitiligo starts as well as stays in one side of body. It is an autoimmune disease. It is clear early age groups, affecting about 30 percent of children diagnosed with vitiligo. It responds well to treatment.
It is an autoimmune disease as well as often mirrors on both sides of the body. It is most common ty vitiligo observed in 90?ses. They often appear on skin that is commonly exposed to the sun, the face, neck, and hands.
Mixed Vitiligo intersection of both types in the rare cases where segmental becomes non-segmental. [5,6,9,10, 11]
DIAGNOSIS AND TREATMENT:
Diagnosing vitiligo involves a comprehensive approach that includes medical history assessment, physical examination, and specific diagnostic tests. Your doctor will inquire about your medical history and scrutinize your skin to rule out other skin conditions like dermatitis or psoriasis. They may use a special lamp emitting ultraviolet light to examine your skin for signs of vitiligo.

In addition, your doctor may perform a skin biopsy, taking a small sample of affected skin, and order blood tests to check for underlying autoimmune conditions such as anemia or diabetes. The Wood's light, a type of ultraviolet light, can be particularly useful in diagnosing vitiligo, especially in individuals with lighter skin tones. This diagnostic tool can also help determine the extent and activity of the disease and monitor response to treatment. Furthermore, in individuals diagnosed with vitiligo, it's important to differentiate between complete absence of pigment, hypopigmentation, and normal skin, which can be challenging in light-complexioned patients. However, in classical presentations of vitiligo, especially in symmetrical types, the diagnosis is usually straightforward and can often be made confidently in primary care settings.
Lastly, considering the association between vitiligo and autoimmune thyroid disease, your doctor may recommend a blood test to check thyroid function as part of the diagnostic process. [2,5,8,9,11,12,13]
Treatments:
Treating vitiligo aims to control autoimmune damage to melanocytes and stimulate their migration from surrounding skin and adnexal reservoirs. Treatment options include pharmacological, surgical, and physical approaches, which can sometimes be combined. However, treating vitiligo can be challenging and frustrating for both patients and physicians. The choice of treatment depends on various factors such as age, extent of skin involvement, progression speed, and impact on daily life. Medications and light-based therapies are available but results can be unpredictable and side effects may occur. Therefore, trying self-tanning products or makeup might be suggested initially.
If drug, surgical, or therapeutic interventions are pursued, it may take several months to assess effectiveness, and multiple approaches or combinations may be required. Even if initial treatment is successful, results may not be permanent, and maintenance therapy with topical medications may be recommended to prevent relapse. While no medication can halt the progression of vitiligo, some drugs, alone or in combination with light therapy, may help restore skin tone to some extent. Overall, managing vitiligo requires patience and ongoing monitoring to find the most effective treatment for each individual. [2,4,5,6,7,8,9,11,13,14,15,16]
Various treatments used for treating vitiligo:
- Corticosteroids:
corticosteroids are sometimes prescribed to treat vitiligo, especially in cases where there is active inflammation. Then work by reducing inflammation and suppressing the immune response that may be attacking melanocytes (cells responsible for skin pigmentation). However, it’s essential to use them under the guidance of a healthcare professional, as they can have side effects and may not be suitable for all individuals or all types of vitiligo. [2,4,5,9,11,15,16]
- Topical Immunomodulators:
Topical immunomodulators, such as tacrolimus (Protopic) and pimecrolimus (Elidel), are also used in the treatment of vitiligo. They work by modulating the immune response in the skin, potentially reducing inflammation and halting the progression of vitiligo. These medications are often prescribed for localized areas of vitiligo and are generally considered safer for long-term use compared to corticosteroids, especially on sensitive areas like the face and genital areas. [2,5,6]
- Antioxidants:
Antioxidants play a crucial role in protecting the skin from oxidative stress, which is believed to contribute to the development and progression of vitiligo. While more research is needed to fully understand the role of antioxidants in vitiligo management, some studies suggest that antioxidant supplementation may have potential benefits for individuals with vitiligo. Here are some antioxidants that have been studied in relation to vitiligo:
Vitamin E is a powerful antioxidant that helps protect the skin from damage caused by free radicals. Some studies have suggested that vitamin E supplementation may help reduce oxidative stress and support melanocyte function in individuals with vitiligo.
Vitamin C is another potent antioxidant that plays a critical role in skin health and immune function. It helps neutralize free radicals and regenerate other antioxidants, such as vitamin E. Some research suggests that vitamin C supplementation may help improve repigmentation in individuals with vitiligo.
Alpha-lipoic acid is a powerful antioxidant that helps regenerate other antioxidants, such as vitamins C and E. It has been studied for its potential role in protecting against oxidative stress and promoting skin health in individuals with vitiligo.
Selenium is a trace mineral with antioxidant properties that may help protect the skin from damage caused by oxidative stress. Some studies have suggested that selenium supplementation may help improve repigmentation in individuals with vitiligo.
Polyphenols are a group of compounds found in plant-based foods that have antioxidant and anti-inflammatory properties. Some research suggests that polyphenol-rich foods, such as green tea, may help reduce oxidative stress and inflammation in individuals with vitiligo. It's important to note that while antioxidants may have potential benefits for individuals with vitiligo, more research is needed to fully understand their effectiveness and optimal dosing. Additionally, antioxidant supplementation should be used under the guidance of a healthcare professional to ensure safety and efficacy. [6,9]
- Phototherapy:
Phototherapy is a common and effective treatment option for vitiligo. It involves exposing the skin to specific wavelengths of light, typically ultraviolet (UV) light, to stimulate repigmentation of the affected areas. There are several types of phototherapies used for vitiligo:
- Narrowband UVB (NB-UVB) phototherapy:
Narrowband UVB (ultraviolet B) phototherapy is a common treatment for vitiligo. It involves exposing the skin to a specific wavelength of UVB light using a special lamp. This treatment is effective in stimulating repigmentation of the skin by activating melanocytes. Narrowband UVB phototherapy is generally considered safer and more effective than PUVA therapy, with fewer side effects. It is often recommended for widespread vitiligo or when vitiligo affects large areas of the body. Treatment sessions are usually conducted several times per week over a period of several months. As with any medical treatment, it's important to undergo narrowband UVB phototherapy under the supervision of a dermatologist who can monitor your progress and adjust the treatment as needed to achieve the best results while minimizing potential side effects. [2,4,9,11,14,16]
- Broadband UVB (BB-UVB) phototherapy:
BB-UVB phototherapy uses a broader range of UVB wavelengths compared to narrowband UVB. While it can be effective for vitiligo, narrowband UVB is generally preferred due to its higher efficacy and lower risk of side effects. [2,4,14]
- PUVA (psoralen plus ultraviolet A) therapy:
PUVA therapy involves taking psoralen, a medication that sensitizes the skin to UVA light, followed by exposure to UVA light. This treatment is effective in promoting repigmentation of vitiligo patches but carries a higher risk of side effects, including skin aging and an increased risk of skin cancer, compared to UVB therapy. [2,6,9,15,16]
Systemic PUVA (psoralen plus ultraviolet A) therapy involves taking psoralen, a medication that increases the skin's sensitivity to ultraviolet light, followed by exposure to ultraviolet A (UVA) light. This treatment is used for widespread vitiligo that hasn't responded to other treatments. PUVA therapy works by stimulating repigmentation of the skin by activating melanocytes. However, systemic PUVA therapy carries some risks, including an increased risk of skin cancer and cataracts, so it's usually reserved for cases where other treatments have been ineffective or when vitiligo is extensive and significantly affecting the individual's quality of life. It's important to undergo PUVA therapy under the supervision of a dermatologist who can monitor for potential side effects and adjust the treatment regimen as needed.[2]
Topical PUVA (psoralen plus ultraviolet A) therapy involves applying psoralen directly to the affected areas of the skin, followed by exposure to ultraviolet A (UVA) light. This treatment is often used for localized vitiligo, particularly in cases where other treatments have not been effective or are not suitable. Topical PUVA therapy is generally considered safer than systemic PUVA because it exposes only the affected areas of the skin to the medication and UV light, minimizing the risk of systemic side effects. However, it still carries some risks, such as skin irritation and increased sensitivity to sunlight. As with any vitiligo treatment, it's essential to undergo topical PUVA therapy under the guidance of a dermatologist who can monitor your progress and adjust the treatment as needed to achieve the best results while minimizing potential side effects.[2] Excimer lasers: Excimer lasers deliver targeted UVB light to vitiligo patches, allowing for precise treatment of affected areas. Excimer laser therapy is particularly useful for treating small, localized patches of vitiligo and may be more convenient for patients who have difficulty accessing phototherapy clinics. [2,14,16]
5. Phototherapy is typically administered in a dermatologist's office or specialized phototherapy clinic. Treatment schedules vary depending on the type and severity of vitiligo, but patients typically undergo multiple sessions over several weeks or months to achieve optimal results. It's essential to undergo phototherapy under the supervision of a healthcare professional who can monitor your progress and adjust the treatment regimen as needed. Additionally, sun protection measures should be followed during and after phototherapy sessions to minimize the risk of sunburn and skin damage. [2,4,5,6,8,9,13,14,15]
6. Microphototherapy:
Microphototherapy is a newer treatment option for vitiligo that involves the use of targeted narrowband UVB light delivered through a device equipped with an array of LED lights. This treatment aims to stimulate repigmentation of the skin by specifically targeting the affected areas with precise doses of UVB light. Microphototherapy is often considered safe and well-tolerated, with minimal risk of side effects compared to traditional phototherapy methods. It may be particularly beneficial for treating small or hard-to-reach areas of vitiligo, such as the face or hands. However, like any medical treatment, the effectiveness of microphototherapy can vary from person to person, and results may not be immediate. It's essential to discuss this option with a dermatologist who can evaluate your specific situation and determine if microphototherapy is suitable for you.[2]
7. Monochromatic Excimer Light Therapy: Monochromatic excimer light therapy is another treatment option for vitiligo. It involves using a specialized excimer laser or excimer lamp to deliver high-intensity UVB light at a specific wavelength directly to the affected areas of the skin. This targeted approach aims to stimulate repigmentation by promoting the proliferation of melanocytes in the affected areas. Excimer light therapy is often used for localized vitiligo, particularly for small patches or areas where other treatments have not been effective. It's generally well-tolerated and can produce noticeable results with regular treatments over time. As with any medical treatment, it's essential to consult with a dermatologist who can assess your specific condition and determine if monochromatic excimer light therapy is a suitable option for you. They can also provide guidance on the frequency and duration of treatment sessions to achieve the best results while minimizing potential side effects. [2,14,16]
8. Calcineurin inhibitors:
Calcineurin inhibitors, such as tacrolimus and pimecrolimus, are immunomodulatory medications that have been used off-label for the treatment of vitiligo. They work by suppressing the immune response in the skin, which may help to halt the progression of vitiligo and promote repigmentation of affected areas. Topical calcineurin inhibitors are typically prescribed for localized vitiligo, particularly in areas where other treatments may not be suitable, such as the face and genital areas. They are often considered safer for long-term use compared to topical corticosteroids, especially on thin or sensitive skin. While calcineurin inhibitors can be effective in some cases, their use in vitiligo treatment is still being studied, and their effectiveness may vary from person to person. It's important to use them under the guidance of a healthcare professional who can monitor your progress and adjust the treatment regimen as needed. Additionally, it's essential to follow the prescribed application instructions and discuss any potential side effects or concerns with your doctor. [9,11,15,16]
- JAK (Janus kinase) inhibitors:
JAK (Janus kinase) inhibitors are a class of medications that work by blocking the activity of certain enzymes involved in the immune response. While JAK inhibitors have shown promise in treating various inflammatory and autoimmune conditions, including rheumatoid arthritis and psoriasis, their use in vitiligo is still being explored. Recent research has investigated the potential of JAK inhibitors for treating vitiligo, particularly for cases that are resistant to other treatments or involve widespread or rapidly progressing disease. Preliminary studies have shown promising results, with some individuals experiencing significant repigmentation of vitiligo patches after treatment with JAK inhibitors. Currently, topical and oral JAK inhibitors are being studied in clinical trials for vitiligo. These medications are thought to work by suppressing the immune response and promoting the proliferation and activation of melanocytes, the pigment-producing cells in the skin. While the use of JAK inhibitors for vitiligo is still investigational, early findings suggest that they may offer a new treatment option for individuals with vitiligo, particularly those who have not responded to other treatments. However, more research is needed to determine their long-term safety and effectiveness in treating vitiligo. It's essential to consult with a dermatologist or healthcare professional to discuss the potential benefits and risks of JAK inhibitors for vitiligo, as well as any ongoing clinical trials or treatment options that may be available. [6,15]
- Vitamin D3:
Vitamin D3 supplementation has been explored as a potential adjunctive treatment for vitiligo due to its immunomodulatory effects and its role in melanocyte function. Some studies suggest that vitamin D3 may help regulate the immune response and promote repigmentation in individuals with vitiligo. However, the evidence supporting the use of vitamin D3 supplements as a standalone treatment for vitiligo is limited, and more research is needed to determine its effectiveness. Additionally, vitamin D3 supplementation should be used under the guidance of a healthcare professional, as excessive vitamin D intake can lead to adverse effects. While vitamin D3 may have potential benefits for individuals with vitiligo, it is not considered a primary treatment for the condition. Instead, it may be used as part of a comprehensive treatment plan that includes other conventional therapies, such as phototherapy, topical treatments, or systemic medications. If you're considering vitamin D3 supplementation for vitiligo, it's essential to consult with a dermatologist or healthcare provider to discuss its potential benefits and risks in your specific case. [9,15]
- Surgical Epidermal Grafting:
Surgical epidermal grafting is a procedure used to treat stable vitiligo patches, particularly those that have not responded to other treatments. During the procedure, a small piece of normally pigmented skin is removed from a donor site on the patient's body, such as the thigh or buttock. The epidermis (outer layer of skin) from the donor site is then transplanted onto the depigmented areas of skin affected by vitiligo. This technique allows for the transfer of melanocytes, the pigment-producing cells, from the donor skin to the vitiligo-affected skin, promoting repigmentation. Surgical epidermal grafting is often used for localized vitiligo patches or areas where other treatments have been unsuccessful. While surgical epidermal grafting can be effective, it is a surgical procedure that carries risks, including potential scarring at the donor and recipient sites. Additionally, it may require multiple sessions to achieve satisfactory results. It's important to discuss the potential benefits and risks of this procedure with a dermatologic surgeon or dermatologist who specializes in vitiligo treatment. They can evaluate your specific situation and determine if surgical epidermal grafting is an appropriate option for you. [2,11,16,17]
- Epidermal Cell Transplantation:
Epidermal cell transplantation is a surgical procedure used to treat vitiligo, particularly in cases where other treatments have not been effective. During the procedure, a small sample of the patient's normally pigmented skin is taken, typically from an inconspicuous area of the body. The sample is then processed in a laboratory to isolate melanocytes, the pigment-producing cells, from the epidermis. Once isolated, the melanocytes are transplanted onto the depigmented areas of skin affected by vitiligo. This technique allows for the transfer of functional melanocytes to the vitiligo-affected areas, promoting repigmentation. Epidermal cell transplantation can be performed using various methods, including non-cultured epidermal suspension (NCES) and cultured autologous melanocyte transplantation (CAM). These methods differ in the processing and preparation of the melanocytes for transplantation. While epidermal cell transplantation can be effective in repigmenting vitiligo-affected skin, it is a surgical procedure that requires expertise and careful technique. Additionally, it may require multiple sessions to achieve satisfactory results. It's important to consult with a dermatologic surgeon or dermatologist who specializes in vitiligo treatment to determine if epidermal cell transplantation is an appropriate option for you, taking into account your specific condition and treatment goals. [2,5]
- Laser treatment:
Laser treatment is a promising option for vitiligo management, particularly for localized patches. Here are some laser treatments commonly used for vitiligo:
This treatment delivers targeted ultraviolet B (UVB) light to the vitiligo-affected areas. The laser emits a specific wavelength of UVB light, which stimulates melanocyte production and pigmentation in the skin. Excimer laser therapy is effective for small, localized patches of vitiligo and can be used in combination with other treatments.
- Fractional laser therapy:
Fractional laser treatment involves delivering laser energy to microscopic columns of skin, creating small wounds to stimulate the skin's healing response. Fractional lasers, such as fractional CO2 or fractional erbium lasers, have been used to promote repigmentation in vitiligo patches by inducing melanocyte migration and proliferation.
- Q-switched Nd: YAG laser:
Q-switched Nd: YAG lasers emit short pulses of high-energy light, which are absorbed by melanin in the skin. These lasers have been used to induce repigmentation in vitiligo patches by stimulating melanocyte activation and migration. However, results may vary, and multiple sessions may be required for optimal outcomes. Laser treatments for vitiligo are generally safe and well-tolerated, with minimal downtime. However, the effectiveness of laser therapy can vary depending on factors such as the type of vitiligo, the location and size of the affected areas, and individual response to treatment. It's essential to consult with a dermatologist or healthcare professional to determine the most appropriate laser treatment option for your specific condition and treatment goals. They can evaluate your case and provide personalized recommendations tailored to your needs. [9,15,17]
- Cosmetic cover-ups:
Cosmetic cover-ups can be an effective way to conceal vitiligo patches and improve the appearance of the skin. There are several options available: a. Camouflage makeup: Specialized camouflage makeup products are designed to match the individual's skin tone and provide long-lasting coverage for vitiligo patches. These products are typically waterproof and smudge-resistant, providing a natural-looking finish. b. Self-tanning products: Self-tanners or bronzers can help even out skin tone by temporarily darkening the skin. These products can be applied to vitiligo patches to help blend them with the surrounding skin. c. Temporary tattoos: Temporary tattoos or body art can be used to cover up vitiligo patches and create decorative designs on the skin. These tattoos can last for several days to weeks and provide a fun and creative way to conceal vitiligo. d. Derma blend: Derma blend is a brand of high-coverage makeup products designed to cover skin imperfections, including vitiligo patches. Their products are available in a range of shades and formulas to suit different skin types and coverage needs. e. Medical tattooing: Also known as micropigmentation or paramedical tattooing, this technique involves tattooing pigment into the skin to match the surrounding skin tone and camouflage vitiligo patches. Medical tattooing should be performed by a trained professional with experience in treating vitiligo. It's important to choose cosmetic cover-up options that are safe for your skin and provide the desired level of coverage. You may need to experiment with different products and techniques to find what works best for you. Additionally, it's essential to maintain proper skincare and sun protection to protect the skin and prevent further damage. [2,4,8]
- Depigmentation therapy:
Depigmentation therapy, which involves bleaching the remaining normal skin to match the vitiligo-affected areas, may be considered as a treatment option. This approach is typically reserved for individuals with extensive vitiligo who have not responded to other treatments or who find their condition difficult to manage. Depigmentation therapy usually involves the application of a depigmenting agent, such as monobenzone, to the unaffected areas of the skin. This agent gradually lightens the skin over time, resulting in overall depigmentation.

It's essential to note that depigmentation therapy is a significant decision and should be thoroughly discussed with a dermatologist who can provide guidance on its risks, benefits, and suitability for your specific situation. Additionally, depigmentation therapy is permanent, and once the depigmentation process is complete, the skin will remain permanently lighter in color. Therefore, careful consideration and counseling are essential before pursuing this treatment option. [2,4,5,8,13,15]
- Traditional Remedies:
Traditional remedies for vitiligo vary widely and may include herbal treatments, dietary changes, and topical applications. While some people may find relief from these remedies, it's essential to approach them with caution and consult with a healthcare professional before trying them, as their effectiveness and safety can vary. Here are some traditional remedies that people may use for vitiligo:
- Babchi (Psoralea corylifolia):
Babchi seeds are commonly used in Ayurvedic medicine for vitiligo treatment. They contain psoralens, which can make the skin more sensitive to sunlight and may help repigment the affected areas when combined with sun exposure.
Some research suggests that ginkgo biloba extract may help improve repigmentation in vitiligo by stimulating melanocyte activity. However, more studies are needed to confirm its effectiveness.
Turmeric contains curcumin, which has anti-inflammatory and antioxidant properties. Some people may apply turmeric paste topically to vitiligo patches to help reduce inflammation and promote healing.
Copper is involved in melanin production, and some traditional remedies involve taking copper supplements or using copper utensils to drink water.
Khellin is a plant-derived substance that has been used in traditional medicine for vitiligo treatment. It works similarly to psoralen by sensitizing the skin to sunlight.
Radish seeds are sometimes ground into a paste and applied topically to vitiligo patches, although there is limited scientific evidence to support their effectiveness.

It is important to remember that while some traditional remedies may provide relief for some individuals, they may not work for everyone, and their safety and efficacy are not always well-established. Consulting with a dermatologist or healthcare professional is crucial before trying any traditional remedy for vitiligo to ensure it is safe and appropriate for your specific condition. [2,4,11]
Siddha medicine is a traditional system of medicine that originated in ancient India and is practiced primarily in Tamil Nadu. It encompasses various herbal remedies, dietary recommendations, and lifestyle practices to maintain health and treat various ailments, including vitiligo. In Siddha medicine, vitiligo is often referred to as "ven kushtam" or "ven suram," and treatments aim to balance the body's doshas (energetic forces) and restore harmony to the body and mind. Some common remedies and practices used in Siddha medicine for vitiligo include:
Siddha practitioners may prescribe herbal formulations containing a combination of herbs, minerals, and other natural ingredients believed to have depigmenting or repigmenting properties. These formulations are often tailored to the individual's constitution and specific symptoms.
Dietary modifications may be recommended to support overall health and balance the doshas. This may include consuming a balanced diet rich in fruits, vegetables, whole grains, and herbs believed to have therapeutic properties.
Siddha medicine emphasizes the importance of detoxification to remove toxins from the body and restore balance. Therapies such as purgation, emesis, and herbal baths may be recommended to cleanse the body and promote healing.
Siddha practitioners may also recommend lifestyle modifications, including stress management techniques, regular exercise, and adequate rest, to support overall well-being and improve the body's ability to heal. While Siddha has a long history of use for various health conditions, including vitiligo, scientific evidence supporting Its effectiveness is limited. As with any alternative or complementary therapy, it's essential to consult with a qualified Siddha practitioner or healthcare professional before trying Siddha remedies for vitiligo. They can provide personalized recommendations based on your individual health needs and ensure that any treatments are safe and appropriate for you.[2]
Homeopathy offers various remedies for vitiligo, depending on individual symptoms and constitution. Some common homeopathic remedies used for vitiligo include:
This remedy may be suitable for individuals with dry, scaly, or itching vitiligo patches, particularly when there is a history of suppressed skin conditions.
Recommended for individuals with vitiligo who experience burning sensations or restlessness, especially at night.
Indicated for individuals with vitiligo who have a delicate constitution and are prone to coldness, sweating on the head, and easily catching colds.
Useful for individuals with vitiligo who have a tendency towards unhealthy skin, itchiness, and burning sensations. It may be prescribed when there are associated skin conditions like eczema or psoriasis.
Suitable for individuals with vitiligo who are generally sensitive and may experience burning pains or weakness, especially in the eyes.
Indicated for vitiligo patches with a warty appearance or when there is a history of vaccination or suppressed skin conditions.
Recommended for individuals with vitiligo who tend to be overweight and easily fatigued, with a tendency towards clammy hands and feet. It's important to consult with a qualified homeopathic practitioner for personalized treatment recommendations tailored to your individual symptoms, constitution, and overall health. Homeopathic remedies should be used under the guidance of a professional to ensure their safety and effectiveness.[2]
Yoga therapy can complement traditional medical treatments for vitiligo by helping to reduce stress, boost immune function, and improve overall well-being. While yoga therapy alone may not directly treat vitiligo, it can be beneficial as part of a holistic approach to managing the condition. Here are some ways yoga therapy may be helpful for individuals with vitiligo:
Stress is often cited as a trigger for vitiligo flare-ups or exacerbations. Yoga practices such as deep breathing, meditation, and relaxation techniques can help reduce stress levels, promote relaxation, and improve coping mechanisms.
Some studies suggest that yoga may have immune-modulating effects, potentially enhancing the body's immune response. Strengthening the immune system can be beneficial for individuals with vitiligo, as it may help prevent further progression of the condition.
Certain yoga poses and practices can improve blood circulation and lymphatic flow, which may support overall skin health and potentially aid in the delivery of nutrients to the skin cells.
Yoga encourages mindfulness and body awareness, helping individuals become more attuned to their bodies' needs and signals. This heightened awareness may facilitate better self-care practices and early recognition of symptoms or changes in the skin.
Vitiligo can have a significant impact on self-esteem and body image. Engaging in yoga therapy can promote self-acceptance, self-confidence, and a positive body image, fostering a sense of empowerment and resilience. It's important for individuals with vitiligo to work with a qualified yoga instructor who understands their specific needs and limitations. Modified yoga poses may be necessary for individuals with skin sensitivity or depigmented areas to prevent irritation or injury.[2]
Traditional Chinese Medicine (TCM) offers various treatments for vitiligo, focusing on restoring balance to the body and addressing underlying imbalances believed to contribute to the condition. TCM approaches vitiligo as a manifestation of internal disharmony, often involving deficiencies in qi (vital energy), blood, or yin and yang imbalance. Here are some common TCM treatments for vitiligo:
Chinese herbal formulas are tailored to the individual's specific pattern of disharmony and may include a combination of herbs believed to tonify the blood, nourish yin, and invigorate qi. Some commonly used herbs for vitiligo include Dong Quai (Dang Gui), and Ginseng (Ren Shen), Tong-Qiao-Huo-Xue decoction, Xiao-Yao powder and Si-Wu decoction.
Acupuncture involves the insertion of thin needles into specific points on the body to stimulate qi flow and restore balance. It is believed to regulate the body's energy flow and may help improve circulation, reduce inflammation, and promote healing in vitiligo-affected areas.
Moxibustion involves burning dried mugwort (Artemisia vulgaris) near acupuncture points to stimulate circulation and promote healing. It is often used in combination with acupuncture for vitiligo treatment.
TCM dietary recommendations for vitiligo typically involve consuming foods believed to tonify qi and blood, such as dark leafy greens, legumes, and nourishing soups. Avoiding foods that are considered to exacerbate imbalances, such as spicy or greasy foods, may also be recommended.
Topical herbal ointments or pastes may be prescribed to apply directly to vitiligo-affected areas to promote repigmentation and skin healing. It's essential to consult with a qualified TCM practitioner or herbalist who can assess your individual pattern of disharmony and provide personalized treatment recommendations. TCM treatments for vitiligo may take time to show results, and it's important to be patient and consistent with treatment. [2,8]
Vitiligo presents a complex interplay of immune dysregulation and melanocyte destruction, resulting in significant challenges for both patients and clinicians. Despite advancements in understanding its pathogenesis and the development of various treatment modalities, achieving satisfactory outcomes remains elusive. Current therapies primarily focus on symptom management and halting disease progression rather than offering a definitive cure. While conventional treatments like topical steroids and phototherapy provide some relief, emerging options such as excimer laser and topical calcipotriol offer promise for improved outcomes. However, the quest for more effective and targeted therapies continues, given the persistent emotional burden and psychosocial impact vitiligo imposes on affected individuals. Future research endeavors should aim at unraveling the intricate mechanisms underlying vitiligo pathogenesis, paving the way for innovative therapeutic approaches that not only halt disease progression but also facilitate repigmentation and enhance patient quality of life. Collaborative efforts between researchers, clinicians, and patients are crucial in addressing the unmet needs in vitiligo management and bringing about meaningful advancements in its treatment paradigm.


 Prajakta D. Gawade * 2
Prajakta D. Gawade * 2
 Manasi V. Shelke 2
Manasi V. Shelke 2
 Rahul R. Vishwakarma 2
Rahul R. Vishwakarma 2
 Harshal Vishe 1
Harshal Vishe 1





 10.5281/zenodo.11045812
10.5281/zenodo.11045812