Psychiatric disorders such as depression, schizophrenia, hypertension and anxiety represent complex medical challenges with roots in both neurobiological and environmental factors. This review examines the multifaceted etiology of these conditions, with a particular emphasis on genetic predispositions, neurobiological markers, and environmental influences like trauma and socioeconomic stress. Genetic studies reveal that polygenic contributions, including variations in neurotransmitter pathways (e.g., serotonin and dopamine), significantly increase susceptibility to psychiatric conditions. Concurrently, structural brain changes such as enlarged ventricles and cortical abnormalities further illuminate neurobiological foundations, particularly in disorders like schizophrenia. Environmental factors, ranging from early-life stress to ongoing socioeconomic adversities, interact dynamically with genetic predispositions, creating unique gene-environment interaction profiles that affect disease onset, progression, and response to treatment. Given the complexity of these interactions, there is a growing interest in personalized interventions, integrating conventional therapies with alternative modalities. This review explores camphor-based therapies as an emerging complementary approach. Camphor, traditionally valued for its neurostimulant properties, shows potential in modulating mood and anxiety through its effects on neurotransmitter pathways. Here, we synthesize current insights on psychiatric disorder etiology, discuss gene-environment interplay, and evaluate camphor’s role in innovative therapeutic strategies, proposing a foundation for future, integrative approaches to mental health treatment.
Schizophrenia, Psychiatric disorders, etiology, socioeconomic, neurobiological markers.
Psychiatric disorders, encompassing conditions like depression, anxiety, and schizophrenia, are among the most challenging and enigmatic health issues worldwide. Their origins lie in a complex interplay between genetic predispositions, neurobiological abnormalities, and a range of environmental stressors, each contributing to the unique pathology of mental health disorders. Recent advancements in genomics and neuroimaging have revealed insights into the biological underpinnings of these disorders, identifying critical markers such as neurotransmitter imbalances and structural brain changes that influence mental health outcomes. Simultaneously, a growing body of research highlights the profound role of environmental factors such as early life trauma, socioeconomic stress, and lifestyle factors in modulating psychiatric symptoms and disease progression [1,3]. In response to the multifactorial nature of psychiatric etiology, there is an increasing emphasis on integrative therapeutic approaches that bridge traditional and alternative medicine. This article explores the potential of camphor-based modalities as a complementary intervention.
Traditionally recognized for its neurostimulant and anxiolytic properties, camphor may offer therapeutic benefits by modulating neurotransmitter systems and enhancing mood stability. By examining both established and emerging perspectives on psychiatric disorder etiology, this review seeks to uncover novel avenues for treatment, emphasizing a holistic approach that respects the complexity of mental health and aims for more personalized, adaptive care strategies.
- Neurobiological Determinants: Genetic Contributions
- Heritability Studies and Genetic Predispositions
Psychiatric diseases, including depression and anxiety, are significantly told by inheritable factors, as shown through heritability studies involving family, binary, and relinquishment studies. Major depressive complaint (MDD), for case, has been estimated to have a heritability rate of around 40- 50, while generalized anxiety complaint and affiliated conditions show analogous inheritable benefactions. Studies of binary and family cohorts reveal that close cousins of individualities with psychiatric diseases have a markedly advanced threat of developing analogous conditions, supporting the strong part of inherited inheritable factors [7,8]. The inheritable base of these diseases has been further illustrated through the identification of specific threat- associated genes. For case, genes related to the serotonin transporter (SLC6A4), brain- deduced neurotrophic factor (BDNF), and dopamine pathways have been linked to heightened vulnerability to anxiety and depressive diseases. Variants in these genes can lead to dysregulations in neurotransmitter systems, impacting mood regulation and stress responses. also, genome-wide association studies (GWAS) have linked polygenic threat factors, which inclusively contribute to the inheritable element of psychiatric conditions. These findings emphasize the polygenic nature of psychiatric diseases, indicating that multiple genes with small individual goods contribute to overall threat [7,9].
- The Part of Epigenetics
While genetics establish a birth vulnerability, environmental factors play a pivotal part in modulating gene expression, a miracle best understood through epigenetics. Epigenetic mechanisms, similar as DNA methylation, histone revision, and non-coding RNA relations, influence how genes are expressed without altering the DNA sequence itself. For case, exposure to early life stress or trauma can spark lasting epigenetic changes that increase the threat for psychiatric conditions latterly in life. Epigenetic variations on genes involved in the stress response similar as those governing the hypothalamic- pituitary- adrenal (HPA) axis have been associated with a lesser threat of developing depression and anxiety [10,11]. Also, epigenetic changes have counteraccusations for treatment responsiveness. Epigenetic labels are decreasingly being studied as implicit predictors of remedial issues, especially in psychotherapeutic and pharmacologic interventions. This rigidity in gene expression due to environmental exposures suggests that while inheritable predilection is important, life gests and their impact on the genome are inversely pivotal in understanding psychiatric diseases [10,12]. By combining perceptivity from heritability tudies and epigenetic exploration, our understanding of psychiatric diseases' etiology becomes further comprehensive, pointing towards substantiated remedial approaches that regard for both inheritable background and environmental history.
Neurotransmitter Imbalances in Depression and Anxiety: Serotonin, Dopamine, GABA, and Norepinephrine
Psychiatric conditions like depression and anxiety are explosively told by dysregulations in crucial neurotransmitter systems. These include serotonin, dopamine, gamma- aminobutyric acid (GABA), and norepinephrine. Each of these neurotransmitters plays a specific part in mood and emotional regulation, and their imbalances can lead to characteristic symptoms seen in these diseases.
- Serotonin
Serotonin, frequently linked to mood stability, impacts sleep, appetite, and emotional processing. Low situations of serotonin have been associated with passions of sadness, perversity, and increased vulnerability to depressive occurrences. In anxiety diseases, serotonin imbalance can lead to heightened stress responses and increased anxiety perceptivity. This understanding forms the base of picky serotonin reuptake impediments (SSRIs), which enhance serotonin vacuity in the brain to help palliate depressive and anxious symptoms [13,15].
B. Dopamine
Dopamine regulates provocation, price perception, and pleasure, and its insufficiency can lead to apathy, lack of interest in conditioning, and low energy, common in depressive countries. In anxiety, dopamine dysregulation might affect in an incapability to witness positive underpinning, leading to heightened solicitude and avoidance actions. also, dopamine imbalances can affect cognitive functioning, contributing to symptoms like indecisiveness and poor attention, frequently observed in both depression and anxiety [14].
C. Gamma-Aminobutyric Acid (GABA)
GABA is the primary inhibitory neurotransmitter, responsible for reducing neuronal excitability and producing comforting goods. inadequate GABA exertion has been linked to anxiety, as it reduces the brain's capability to regulate stress signals, leading to hyperarousal and pressure. In some individualities with depression, reduced GABA can also contribute to passions of restlessness and incapability to relax, further complicating mood dysregulation. Treatments that increase GABA exertion, like certain anti-anxiety specifics, aim to enhance these inhibitory goods, furnishing symptom relief [17].
D. Norepinephrine
Norepinephrine plays a critical part in attention, thrill, and the body’s stress response. Low norepinephrine situations can lead to reduced alertness, energy, and an incapability to concentrate, which are common in depression. In anxiety diseases, norepinephrine dysregulation can contribute to symptoms of hypervigilance, fear, and heightened stress reactivity. Imbalances in this neurotransmitter produce challenges in conforming to stressors, frequently leading to habitual solicitude and heightened physical symptoms like increased heart rate and muscle pressure [13,16]. Understanding how these neurotransmitters contribute to psychiatric symptoms aids in developing targeted treatments. For illustration, specifics and curatives that stabilize these neurotransmitter situations are extensively used in clinical settings to help palliate symptoms of depression and anxiety, paving the way for better internal health issues.
Neuroanatomy and Brain Structures in Depression and Anxiety
Depression and anxiety are associated with structural and functional changes in specific brain regions, particularly the amygdala, hippocampus, and prefrontal cortex.
- Amygdala: The amygdala plays a crucial part in emotional processing and fear responses. Studies show jacked exertion in the amygdala among individualities with anxiety and depressive diseases, particularly in response to negative or fear- converting stimulants. This increased reactivity can lead to a heightened perception of trouble, buttressing passions of anxiety and aggravating mood diseases [18,20].
- Hippocampus: The hippocampus, critical for memory conformation and emotion regulation, frequently shows reduced volume in cases with depression. habitual stress and dragged exposure to high cortisol situations are allowed to contribute to hippocampal atrophy, which is linked to difficulties with memory and emotional adaptability. similar structural changes may uphold symptoms like patient sadness, reflection, and cognitive difficulties seen in depressive diseases [23,22].
- Prefrontal Cortex: The prefrontal cortex (PFC) is essential for decision- timber, impulse control, and emotional regulation. Dysfunctions in the PFC, frequently observed in depression and anxiety, are associated with disabled cognitive control and emotional dysregulation. Specifically, a weakened connection between the PFC and amygdala may reduce an existent’s capability to manage negative feelings effectively, contributing to symptoms of impulsivity and patient solicitude [18].
Endocrine and HPA Axis Dysregulation
The hypothalamic- pituitary- adrenal (HPA) axis is pivotal forthe body’s response to stress. In response to stress, the hypothalamus releases corticotropin- releasing hormone (CRH), which stimulates the pituitary to release adrenocorticotropic hormone (ACTH), eventually leading tocortisol release from the adrenal glands. Cortisol helps rally energy for managing with stress,but habitual stress disruptsthis system.
1.Habitual Stress and Cortisol Dysregulation Dragged stress can beget HPA axis dysregulation, leading to constantly high or inadequately regulated cortisol situations. This cortisol imbalance has been linked to inflammation and
neurotoxicity, which may vitiate brain areas similar as the hippocampus and prefrontal cortex, aggravating symptomsof depression and anxiety. patient HPAdysregulation therefore contributes to mood insecurity, cognitive impairments, and heightened stress perceptivity [19,21].
2.HPA Axis and Psychiatric diseases
Psychiatric diseases substantiation suggests that people with depression and anxiety frequently have a hyperactive HPA axis, performing in inordinate cortisol release. This overactivity can consolidate negative feelings, produce a heightened stress response, and reduce adaptability against everyday stressors, compounding the inflexibility and continuity of psychiatric symptoms [23]. Both neuroanatomical changes and HPA axis dysregulation interact to produce a natural foundation for the continuity and complexity of symptoms in depression and anxiety. Understanding these mechanisms highlights the significance of interventions that target both neural circuits and stress response systems in treating these conditions.
Part of the Hypothalamic-Pituitary-Adrenal (HPA) Axis in Stress Responses
The HPA axis is a primary element of the body’s stress response system, coordinating the release of hormones to manage stress. Upon encountering stress, the hypothalamus releases corticotropin- releasing hormone (CRH), which signals the pituitary gland to cache adrenocorticotropic hormone (ACTH). ACTH also stimulates the adrenal glands to release cortisol, a hormone that mobilizes energy by adding blood sugar situations and modulating vulnerable responses. Cortisol also acts in a feedback circle to inhibit farther HPA axis activation, helping the body return to a balanced state after a stressor passes [19].
Impact of Chronic Stress and Cortisol Dysregulation on Psychiatric Disorders
Habitual stress can lead to patient HPA axis activation, performing in sustained high cortisol situations. This prolonged cortisol release disrupts normal brain functions, particularly in areas like the hippocampus and prefrontal cortex, which are involved in mood regulation and cognition. similar dislocation is linked to symptoms of depression, anxiety, and cognitive impairment. Over time, this dysregulated cortisol product can also vitiate the vulnerable system, adding vulnerability to inflammation and farther amplifying stress perceptivity [23,21].
Neuroinflammation in Depression and Anxiety
Increased inflammation is frequently observed in individualities with depression and anxiety, with elevated situations of seditious labels like cytokines (e.g., interleukin- 6 and excrescence necrosis factor- nascence). habitual stress can complicate this response by driving vulnerable cells in the brain (microglia), which release seditious chemicals, promoting neuroinflammation. This seditious state interferes with neurotransmitter function and neuroplasticity, potentially leading to symptoms like fatigue, low mood, and anhedonia (incapability to feel pleasure) [22].
Mechanisms Linking Neuroinflammation to Psychiatric Symptoms
1.Dislocation of Neurotransmitter Systems
Inflammatory cytokines can alter the conflation and release of crucial neurotransmitters, including serotonin and dopamine. For illustration, inflammation may increase the metabolism of tryptophan, a precursor to serotonin, reducing serotonin situations and therefore contributing to depressive symptoms.
2. Impact on Neuroplasticity
Habitual inflammation can drop brain- deduced neurotrophic factor (BDNF), which is essential for neuroplasticity. Reduced BDNF situations may hamper the brain's capability to acclimatize and recover from stress, sustaining depressive and anxiety- related symptoms.
3. Interaction with the HPA Axis
Elevated seditious labels can further spark the HPA axis, immortalizing the cycle of stress and inflammation. This commerce exacerbates cortisol dysregulation, which, in turn, intensifies the seditious response, creating a feedback circle that contributes to the continuity of psychiatric diseases [23,21].
Understanding these processes underscores the significance of remedial approaches targeting both HPA axis regulation and seditious pathways in treating anxiety and depression.
- Environmental Determinants:
1. Childhood and Early Life Adversities
Impact of Adverse Childhood Experiences (ACEs) on Long-term Mental Health
Adverse childhood experiences (ACEs), similar as family violence, poverty, and maternal loss, are well-proved to have a continuing impact on internal health. This experience can affect the brain’s stress- response systems, including the hypothalamic- pituitary- adrenal (HPA) axis. The HPA axis, responsible for regulating cortisol situations, can come dysregulated due to early life stress, leading to habitual cortisol release, which is associated with heightened vulnerability to mood diseases latterly in life. exploration shows that ACEs can affect brain structures like the amygdala and prefrontal cortex, which are involved in emotional regulation and impulse control, contributing to diseases similar as anxiety and depression in majority [18].
The Role of Trauma, Neglect, and Abuse as Risk Factors
Trauma, neglect, and abuse during early development are significant threat factors for psychiatric conditions. Childhood trauma, particularly abuse, can increase perceptivity to stress and affect in a prolonged state of hypervigilance, a particularity generally observed in PTSD. Neglect, where emotional and social requirements are unmet, has been linked to disabled connectivity in brain regions related to social and emotional functioning, potentially leading to difficulties in social connections, reduced adaptability, and a lesser liability of internal health diseases similar as depression and anxiety in majority [24].
2. Social and Environmental Stressors
Modern Lifestyle Factors: Work-related Stress, Social Media, and Economic Pressures
Contemporary social and environmental factors also significantly impact internal health. Job- related stress, especially in largely demanding or insecure places, has been shown to increase the threat of anxiety and depression. Social media, another ultramodern life element, frequently exacerbates passions of inadequacy and low tone-regard, especially in youngish people, as it encourages social comparison. likewise, profitable insecurity and job instability can contribute to habitual stress, which not only affects internal well- being but also raises cortisol situations, promoting a natural terrain conducive to anxiety and depressive diseases [25].
Chronic Stress and Lack of Social Support
Habitual Stress and Lack of Social Support habitual stress without acceptable social support has a considerable impact on cerebral adaptability and can lead to psychiatric vulnerabilities. Social support acts as a buffer against the goods of stress by reducing cortisol situations and enhancing managing mechanisms. In its absence, the sustained cortisol situations associated with habitual stress can beget inflammation and increased threat for diseases like depression. also, the lack of social bonds can vitiate the development of neural pathways associated with stress regulation, amplifying the goods of both ACEs and ongoing life stress on internal health [26].
3. Lifestyle Factors
Impact of Sleep, Diet, and Physical Exertion on Mental Health
Each life factor sleep, diet, and physical exertion affects internal health profoundly, frequently in interrelated ways. Sleep quality, for case, is pivotal for cognitive function, emotional regulation, and adaptability against stress. Poor sleep has been linked to mood diseases like anxiety and depression, as it disrupts neurotransmitter function and the body's capability to manage stress hormones, leading to heightened anxiety and perversity [28]. A balanced diet supports brain health by furnishing essential nutrients for neurotransmitter conflation and energy regulation. Diets high in reused foods and sugars can complicate inflammation, which has been associated with advanced rates of depressive symptoms. By discrepancy, diets rich in omega- 3 adipose acids, vitamins, and antioxidants have been shown to appreciatively impact mood and cognitive health [29].
Physical exertion, meanwhile, influences internal health by releasing endorphins and perfecting blood inflow to the brain, which promotes neurogenesis and enhances mood. Exercise is shown to lower stress situations and reduce symptoms of depression and anxiety, incompletely through its goods on the body’s stress- response system [32].
Substance Use and its Bidirectional Relationship with Depression and Anxiety
Substance use frequently co-occurs with depression and anxiety, and a bidirectional relationship exists between them. For case, individualities with depressive symptoms may use substances like alcohol or medicines to tone- rehabilitate, while substance use itself can complicate or indeed initiate internal health conditions. Alcohol, in particular, is a depressant and can lead to or worsen depressive occurrences over time. This relationship suggests that treating internal health issues frequently requires addressing both the cerebral and physiological aspects of substance use [30].
4. Socioeconomic Status and Environmental Inequalities
Influence of Poverty, Neighborhood Violence, and Access to Mental Health Resources
Socioeconomic status (SES) and environmental factors play critical places in internal health. Poverty can produce a cycle of stress and insecurity, adding vulnerability to internal health issues by limiting access to quality food, safe casing, and healthcare coffers. People in lower SES classes frequently witness heightened exposure to neighborhood violence, which can lead to habitual stress and trauma responses, therefore raising the threat of PTSD and other anxiety diseases. also, limited access to coffers, including internal health services, means that numerous individualities with lower SES don't admit timely or effective internal health care [33].
Disparities in Mental Health Care Based on Socioeconomic Factors
Mental health care disparities are significantly influenced by socioeconomic factors, with access to care often depending on income, insurance coverage, and geographic location. In lower-income areas, there are frequently fewer mental health services and a lack of mental health professionals, which leaves people without adequate support. These disparities mean that those in underserved communities often face longer durations of untreated mental illness, leading to worsened outcomes over time. Addressing these disparities is essential for improving public mental health, as equitable access to mental health care can help reduce the broader social and economic impacts of untreated mental illnesses [31].
- Interaction Between Neurobiological and Environmental Factors
In understanding the complexity of mental health, it's essential to explore how both genetic and environmental factors interact to shape individual susceptibility and resilience. These influences span genetic predispositions, environmental modifications of gene expression, and protective factors that contribute to mental health outcomes.
Gene-Environment Interactions
Gene-environment interactions refer to the way genetic vulnerabilities are affected by environmental conditions, which can significantly influence mental health. For instance, individuals with certain genetic markers may have a heightened response to stress, increasing their risk of developing mental health disorders such as depression or anxiety when exposed to adverse life events. A notable example is the interaction between serotonin transporter genes and stress exposure, where individuals with specific genetic variations are more susceptible to stress-related depression [34].
In Gene-environment interactions, environmental factors are not just external triggers; they can activate or suppress genetic predispositions. This interplay suggests that genes and environment co-determine the trajectory of mental health development, often through the modification of neurobiological pathways associated with mood, cognition, and behavior [35,36].
Epigenetic Modifications
Epigenetics adds another layer to the gene-environment dynamic, illustrating how environmental exposures, particularly during sensitive developmental periods, alter gene expression without changing the underlying DNA sequence. Early-life experiences, such as nurturing or trauma, can lead to chemical changes in DNA (e.g., methylation), which then affect gene expression linked to stress responses and emotional regulation. These epigenetic changes are critical because they can produce long-term effects on behavior and increase vulnerability to disorders like PTSD, depression, or anxiety [38].
For instance, adverse childhood experiences (ACEs) have been shown to lead to lasting changes in gene expression, contributing to heightened emotional reactivity and a greater likelihood of mental health issues in adulthood. These epigenetic modifications illustrate how environmental factors can "leave a mark" on one’s genome, with potential impacts across generations [35].
- Role of Resilience and Protective Factors
Resilience, or the capacity to cope and recover from stress, serves as a buffer against both genetic and environmental risks for mental health issues. Neurobiologically, resilience is associated with efficient stress response regulation, possibly involving the prefrontal cortex, amygdala, and hippocampus—brain areas responsible for managing emotional responses. Protective factors like strong social support networks, access to resources, and adaptive coping strategies can significantly enhance resilience, even in those with genetic or environmental vulnerabilities. Supportive relationships, for example, are found to activate neural pathways that reinforce emotional regulation and promote recovery from stress [39].
Furthermore, interventions targeting resilience can alter neurobiological responses to stress, potentially reducing the risk for mental health disorders in at-risk populations. Developing resilience early on through interventions like positive parenting, mental health support, and community resources can thus be a powerful approach in preventing mental health disorders despite genetic predispositions or adverse environments [34]. Together, gene-environment interactions, epigenetic modifications, and resilience illustrate how intertwined neurobiological and environmental factors are in influencing mental health, creating a nuanced framework that highlights both risk and protective factors in mental illness development and prevention.
- Current Treatment Approaches and Implications
Effective treatment of psychiatric disorders like depression and anxiety often requires an integrative approach. This involves pharmacological interventions, psychotherapy, and holistic care, each grounded in an understanding of neurobiology, individual needs, and environmental factors. Here’s a breakdown of each approach:
Pharmacological Treatments
Advances in neurobiology have profoundly informed medication strategies for mental health. Antidepressants, particularly selective serotonin reuptake inhibitors (SSRIs), are widely used to manage depression and anxiety. By increasing serotonin availability in the brain, SSRIs target neural pathways linked to mood regulation, helping alleviate depressive symptoms.
Anxiolytics, such as benzodiazepines, are used to quickly reduce anxiety symptoms by enhancing the effect of GABA, a calming neurotransmitter. While effective, benzodiazepines are typically prescribed for short-term use due to potential dependency risks. Recent research also explores how anti-inflammatory agents and glutamate modulators might serve as novel treatments, as inflammation and glutamate dysfunction are increasingly recognized in mood disorders [40,42].
Psychotherapy and Counseling
Psychotherapy, particularly Cognitive Behavioral Therapy (CBT), is highly effective in addressing faulty thinking patterns and maladaptive behaviors linked to mental health disorders. CBT helps patients replace negative thoughts with more adaptive ones, empowering them to manage their symptoms effectively. Trauma-informed therapy is another crucial approach, especially for those with PTSD or complex trauma histories, as it incorporates safety and stability into treatment. Therapy also enables patients to process environmental factors such as past traumas or ongoing stress, promoting resilience and adaptive coping. Integrating environmental aspects into therapy like addressing relationship dynamics or providing strategies for stress management has been shown to improve treatment outcomes and reduce relapse [44,41].
Holistic and Integrative Approaches
Holistic treatments aim to address both body and mind, providing alternative strategies that can enhance traditional treatments. Lifestyle interventions, such as regular exercise, have shown to reduce anxiety and depression by promoting endorphin release and improving brain plasticity. Mind-body techniques, including mindfulness, yoga, and meditation, have gained traction for their ability to decrease stress and improve emotional regulation. These techniques are particularly effective as adjunctive treatments, helping patients manage stress and cultivate resilience. Moreover, alternative therapies like acupuncture and herbal supplements are also explored in managing anxiety symptoms, though more research is needed for conclusive evidence [43]. An integrated care approach that considers biological, psychological, and social factors has shown significant promise. By combining pharmacological, psychotherapeutic, and holistic strategies, integrated care addresses the multifaceted nature of mental health disorders. Such comprehensive treatment approaches recognize the complex interactions between genetic predispositions, environmental stressors, and neurobiological mechanisms, allowing for tailored care that meets the full spectrum of patient needs [45]. This holistic view not only enhances symptom management but also emphasizes prevention and long-term mental wellness, making it a crucial model for future mental health care.
- Future Directions and Research Gaps
In understanding and treating mental health disorders, several promising avenues are expanding the scope and precision of treatment options. Key future directions include advances in precision psychiatry, deeper insights into the neurobiology of resilience, and the development of interdisciplinary approaches that integrate diverse scientific perspectives.
Precision Psychiatry
Precision psychiatry aims to tailor mental health treatments to individual profiles, incorporating genetic, neurobiological, and environmental data. By examining the unique genetic and neurobiological markers in each person, this approach could lead to highly customized treatments. For instance, researchers are investigating how certain genetic markers might influence antidepressant efficacy or increase susceptibility to side effects. In this context, pharmacogenomics studying the genetic basis of drug response holds particular promise in guiding antidepressant and antipsychotic choices, potentially improving outcomes for patients with treatment-resistant conditions.
Precision psychiatry also considers environmental factors, such as early-life trauma, which may inform personalized therapy approaches in ways that account for past experiences and stress levels. This emerging field could fundamentally transform psychiatry from a one-size-fits-all model to one that maximizes individual response and minimizes side effects [40,42].
Advancements in Understanding the Neurobiology of Resilience
Resilience, the ability to adapt to and recover from adversity, has gained attention as a protective factor against mental illness. Although resilience has psychological and social components, researchers are increasingly focusing on its neurobiological underpinnings. For instance, certain neurobiological pathways, such as those involving the hypothalamic-pituitary-adrenal (HPA) axis, may play a role in an individual's ability to manage stress. Studies have also examined how brain plasticity particularly in regions like the hippocampus and prefrontal cortex may contribute to resilience. Research on how gene expression can be altered in response to supportive or stressful environments (epigenetic modifications) is shedding light on how resilience can potentially be strengthened. Understanding these mechanisms could lead to novel therapeutic approaches aimed at boosting resilience through lifestyle interventions, pharmacological options, or cognitive training [41,44].
Interdisciplinary Approaches
As mental health is influenced by a multitude of factors, an interdisciplinary approach is critical for future research and treatment innovations. Integrating social, psychological, and biological sciences enables a holistic understanding of mental health disorders. For example, combining neurobiological insights with sociological perspectives on stress and trauma can provide a fuller picture of how societal conditions influence mental health. Similarly, integrating psychological models of cognitive-behavioral patterns with genetic data could reveal why certain individuals are more vulnerable to developing anxiety or depression Interdisciplinary approaches also facilitate the development of more comprehensive treatment plans that address not only the biological symptoms of disorders but also the psychological and social dimensions of recovery. This integration is increasingly being used in clinical settings where mental health treatment teams may include neuroscientists, social workers, psychologists, and psychiatrists, all working together to create personalized care plans that consider the whole person [45].
Research Gaps
Despite these advances, several gaps remain. For precision psychiatry, more longitudinal studies are needed to determine the long-term effects and efficacy of genetically tailored treatments. Additionally, while the neurobiology of resilience is gaining clarity, there is still a need for research on how specific interventions can enhance resilience in diverse populations.
Finally, interdisciplinary research could benefit from increased funding and structural support, as traditional scientific research often remains siloed. Addressing these gaps will require commitment from both research institutions and funding bodies to prioritize holistic and integrated research initiatives [43].
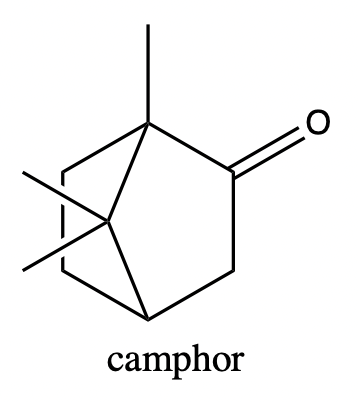
- Harnessing the Therapeutic Power of Camphor for Psychiatric Disorders
Camphor (Cinnamomum camphora), a substance derived from the wood of the camphor tree, has been historically used in traditional medicine for a variety of purposes, including as an anti-inflammatory, analgesic, and for its aromatic properties. There has been growing interest in its potential for treating psychiatric disorders, including anxiety, depression, stress, and trauma. While research on camphor’s direct effects on mental health is still limited, it is believed that its therapeutic properties may help in managing certain psychiatric conditions
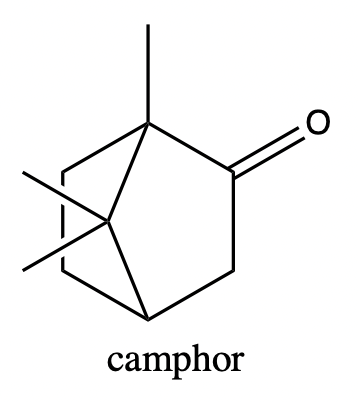

Properties of Camphor


 Riya Bokade *
Riya Bokade *
 Dr. Karna Khavane
Dr. Karna Khavane

 10.5281/zenodo.14580869
10.5281/zenodo.14580869