Abstract
Asthma management has traditionally relied on patient adherence to medication regimens and symptom tracking. Recent advancements in technology have led to the development of smart inhalers, which integrate dosing technology with digital health tools to enhance asthma care. This paper presents an overview of a smart inhaler designed to monitor medication use, track environmental triggers, and provide real-time feedback to patients and healthcare providers. The device utilizes Bluetooth connectivity to sync data with a mobile application, allowing users to record symptoms, medication adherence, and peak flow readings. Through data analytics, the inhaler can identify patterns and provide personalized recommendations, aiming to improve patient outcomes and reduce exacerbations. Clinical trials demonstrate the efficacy of smart inhalers in increasing adherence and improving overall asthma control. This innovative approach not only empowers patients but also facilitates proactive management of asthma, ultimately contributing to enhanced quality of life. Future directions include integration with electronic health records and expansion of features to address diverse patient needs.
Keywords
Asthma, Pathophysiology of Asthma, Diagnosis of asthma, Integrated Dosing Technology, Smart Inhaler.
Introduction
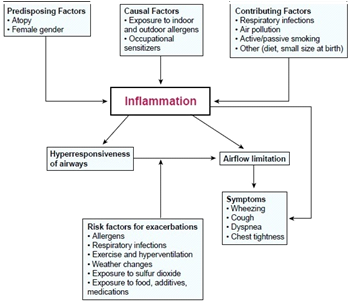
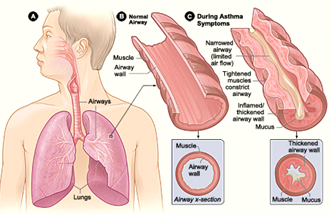
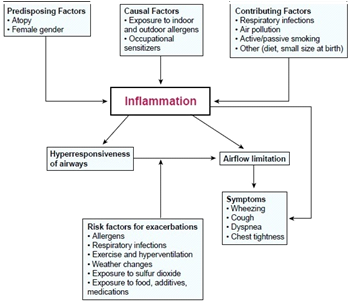
Asthma is a prevalent chronic inflammatory respiratory condition affecting millions of people worldwide and present substantial challenges in both diagnosis and management. This respiratory condition is characterized by inflammation of the airways, causing intermittent airflow obstruction and bronchial hyper responsiveness. The hallmark asthma symptoms include coughing, wheezing, and shortness of breath, which can be frequently exacerbated by triggers ranging from allergens to viral infections. The prevalence and severity of asthma are determined by a complex interplay between genetic and environmental factors. Despite treatment advancements, disparities persist in asthma care, with variation in access to diagnosis, treatment, and patient education across different demographics.
Asthma remains the most common chronic respiratory disease in Canada, affecting approximately 10% of the population. Although asthma is often believed to be a disorder localized to the lungs, current evidence indicates that it may represent a component of systemic airway disease involving the entire respiratory tract, and this is supported by the fact that asthma frequently coexists with other atopic disorders, particularly allergic rhinitis.
Despite significant improvements in the diagnosis and management of asthma over the past decade, as well as the availability of comprehensive and widely-accepted national and international clinical practice guidelines for the disease, asthma control in Canada remains suboptimal. Results from the recent reality of asthma control (TRAC) in Canada study suggest that over 50% of Canadians with asthma have uncontrolled disease. Poor asthma control contributes to unnecessary morbidity, limitations to daily activities and impairments in overall quality of life.
Types of asthma:
- Episodic asthma
- Chronic asthma
- Severe acute asthma
- Occupational asthma
- Exercise induced asthma
- Nocturnal asthma
SYMPTOMS
Symptoms of asthma can vary from person to person. Symptoms sometimes get significantly worse. This knows as an asthma attack. Symptoms are often worse at night or during exercise.
Common symptoms of asthma include:
What causes asthma?
Scientists continue to explore what causes asthma, but we do know that these factors play an important role in the development of asthma:
A family history of asthma is sarong indicator that someone is more likely to develop asthma themselves. In fact, children with a parent who has asthma are three to six times more likely to develop asthma than children without a parent with asthma.
Some people are more likely to develop allergies than other, especially if one of their parents has allergies. Certain allergic dermatitis (eczema) or allergic rhinitis (hay fever), are linked to people who get asthma
- VIRAL RESPIRATORY INFECTIONS
Viral respiratory tract infections are the most common cause of wheezing illnesses and asthma exacerbations in both children and adults. In young children, infection with viral respiratory infections can induce symptoms of acute bronchiolitis, croup, and recurrent wheezing
It is a type of asthma caused by exposure to inhaled irritants in the workplace. Occupational asthma is often a reversible condition, which means the symptoms may disappear when the irritants that caused the asthma are avoided.
When a person inhales tobacco smoke, irritating substances settle in the moist lining of the airways and can set off asthma episodes. Often, the lungs of people with asthma who smoke are in a constant state of poor asthma control. These people often have ongoing asthma symptoms.
Air pollution can increase you risk of getting asthma or can worse your symptoms if you already have asthma. Small airborne particles, found in haze,
Smoke, soot, and airborne dust can lead to serious air quality problems. Small airborne particles are called “particulate matter” or pm.
Obesity can reduce the size of the airway, lower lung capacity, and make the throat more likely to collapse while a person sleeps. People with mild narrowing of their airway may snore at night, while those with significant6 narrowing have periods where their breathing is restricted or paused.
EPIDEMIOLOGY
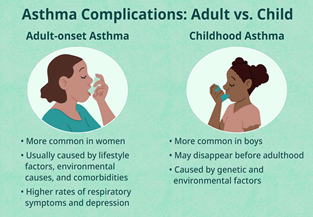
About 20 million Americans have asthma and approximately 300 million people suffer from it worldwide. Nearly 7 million of these are children, although any children asthma in their teen year. Each year 5,000 people die from asthma and it tends to run in families.
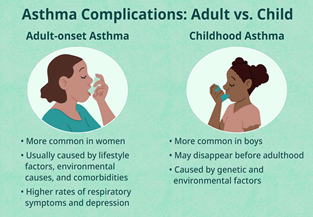
Asthma is a globally significant non-communicable disease with major public health consequences for both children adults, including high morbidity, and mortality in severe cases. We have summarized the evidence on asthma trends, environmental determinants, and long-term impacts while comparing these epidemiological features across childhood asthma and adult asthma. while asthma incidence and prevalence are higher in children, morbidity, and mortality are higher in adults. Childhood asthma is more common in boys while adult asthma is more common in women, and the reversal of this sex difference in prevalence occurs around puberty suggesting sex hormones may play a role in the etiology of asthma. The global epidemic of asthma that has been observed in both children and adults is still continuing, especially in low to middle income countries, although it has subsided in some developed countries. As a heterogeneous disease, distinct asthma phenotypes, and end types need to be develop more accurate and meaningful definitions for use in research and clinical settings. This may be facilitated by new clustering techniques such as latent class analysis, and computational phenotyping methods are being developed to retrieve information from electronic health records using natural language processing (NLP) algorithms to asthma. While some important environmental determinants that trigger asthma are well-established, more work is needed to define the role of environmental exposures in the development of asthma in both children and adults. There is increasing evidence that investigation into possible gene-by-environment and environment-by-environment interactions may help to better uncover the determinants of asthma. Therefore, there is an urgent need to further investigate the interrelationship between environmental and genetic determinants to identify high risk groups and key modifiable exposures. For children, asthma may impair airways development and reduce maximally attained lung function, and these lung function deficits may persist into adulthood without additional progressive loss. Adult asthma may accelerate lung function decline and increase the risk of fixed airflow obstruction, with the effect of early onset asthma being greater than late onset asthma. Therefore, in managing asthma, our focus going forward should be firmly on improving not only short-term symptoms, but also the long-term respiratory and other health outcomes.
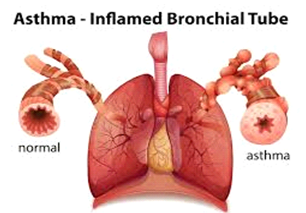
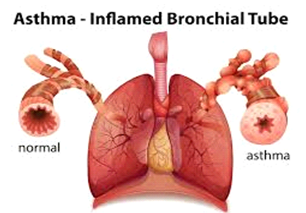
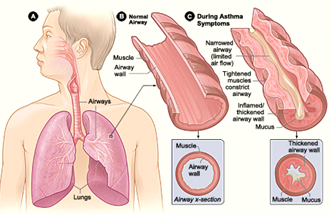
PATHOPHYSIOLOGY
Inflammation of the lining of the airways is a major factor in asthma. This inflammation is produced by your immune system.
The immunes system’s jobs is to defend your body against things that it sees as foreign and harmful, for example, bacteria, viruses, dust and chemicals. It does this by sending special cells to the organs that are being affected by these things. These cells releases chemical that produce inflammation, or swelling, around the foreign substance or substances to isolate and destroy them. Although inflammation is a defense mechanism for our bodies, it can be harmful if it occurs at the wrong time or stays around after it is no longer needed. Because our lungs are used to breathing in air with irritants, such as bacteria, viruses, pollens, and dust, all day every day, they have developed ways of dealing with this things, and normally, an inflammatory response does not occur.
But the airways in the lungs of people with asthma are more sensitive to many of these things, and the immune system in these people overreacts by releasing many different kinds of cells and other chemicals to the airways.
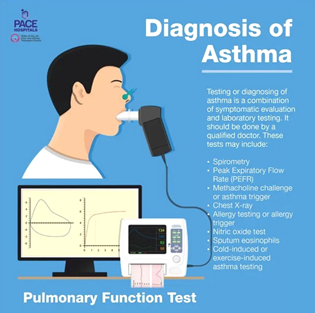
DIAGNOSIS
As asthma diagnosis is based on several factors, including a detailed medical history. A physical exam, your symptoms, and overall health and test results.
Medical history
The first step in diagnosing asthma is talking to your healthcare team about your symptoms and your health. This can provide clues as to whether asthma or something else is causing your symptoms. Your care team will likely ask about your symptoms and your exposure to substances that have been linked to asthma. Some question might include:
- What are your symptoms?
- When do you have them?
- What seems to trigger them? What about cold air, exercise, or allergies?
- Do you have hay fever or allergies?
- Does a family member have hay fever, asthma, or allergies?
- What other health problems do you have?
- What medications do you take?
- Do you often come into contact with tobacco smoke, pets, dust, or chemicals in the air?
- What do you do for a living?
Physical exam
Your doctor will start with a physical exam. They will:
- look at your nose, throat, and upper airways
- Use a stethoscope to listen for a whistling sound when you breathe
- check your skin for allergy symptoms like eczema or hives
They'll also ask you about signs of asthma such as:
- wheezing
- coughing
- breathing problems
- chest tightness
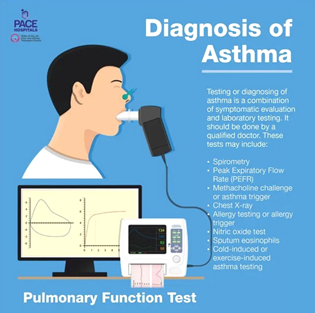
There are several tests that can help diagnose asthma, including:
A spirometer is a device that measures how much air you can breathe out and how quickly. You’ll breathe into the spirometer after breathing in until your lungs are full.
- Peak expiratory flow (PEF) test
This test measures how quickly you can exhale using maximum effort. You can take test with a handheld device or during a spirometry test.
- Bronchodilator responsiveness test
This test measures how much better you can exhale after inhaling a bronchodilator, which is a medicine that relaxes the muscles around your airways.
This test measures the amount of nitric oxide in your breath, which is a sign of inflammation in your lungs.
Your doctors may order blood tests check your immune system. They may check for high levels of eosinophils or immunoglobulin E (lge), which could be a sign of severe asthma.
You doctor may perform allergy testing using blood or skin.
You doctor may order a CT scan to examine your sinuses if they think you have a sinus infection.
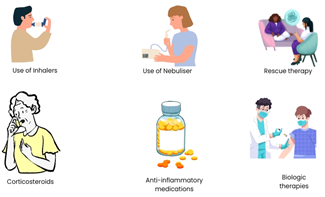
TREATMENT OF ASTHMA
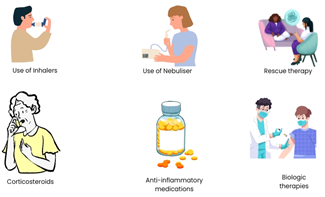
Treatment is self care and bronchodilators to prevent flare ups and manage symptoms
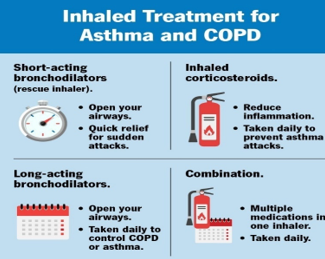
Asthma can usually be managed with rescue inhalers to treat symptoms (salbutamol) and controller inhalers that prevent symptoms (steroids). Severe cases may require longer-acting inhalers that keep the airways open (formoterol, salmeterol, tiotropium), as well as inhalant steroids.

Inhaler
Inhaler are small, handheld devices that allow you to breath medicine in through your mouth,directly to your lungs.Types including metered-dose,dry powder and soft mist inhalers. They usually treat asthma and COPD but provider may prescribe them for other condition. Bronchodilator and corticosteroid are common inhaled medication.
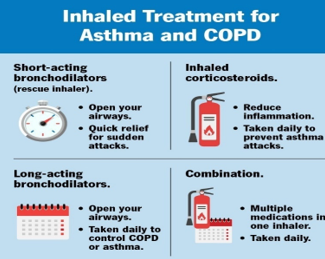
Who needs to use an inhaler?
People with chronic lung condition that affect their breathing, like asthma or chronic obstructive pulmonary disorder (COPD), most commonly use inhalers.you use daily inhalers to prevent or manage your symptoms and fast-acting inhalers during an asthma attack or COPD exacerbation
What condition do inhalertreat ?
Inhaled medication mostcommonly treat asthma and COPD. providers sometimes prescribe them to treat respiratory infections like bronchitis.
providers also use them to treat:
- cystic fibrosis.
- Diabetes.
- Flu.
- Parkinson's disease.
- Schizophrenia.
What are the different types of inhalers?
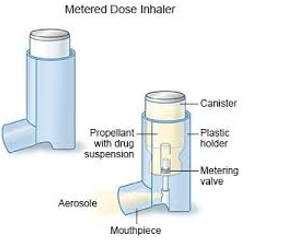
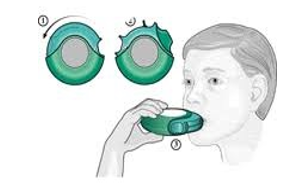
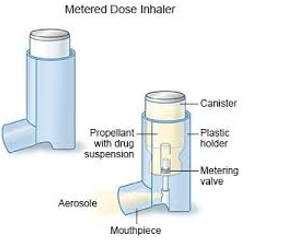
1. Metered dose inhalers.
metered dose inhalers (MDLs or pMDls), sometimes called "puffers," hold the medication in a pressurized canister. the canister sits in a handheld container with a mouthpiece. when you press on the canister, a propellant ( something that helps the medicine move out of the canister ) helps send a puff of medicine out of the mouthpiece. following the directions, you breathe the puff in through you mouth to pull yhe medicine into your lungs. MDls deliver one dose st s time from a canister that holds multiple doses.
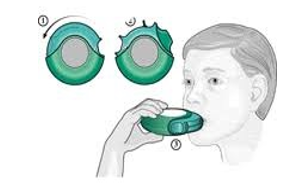
2. Dry powder inhalers.
dry powder inhaler (DPIs) store medication as a powder inside capsules or other containers that you activate when you're ready to use the inhaler. unlike MDIs, a propellant doesn't push the medicine out of a DPI. instead, you use a quick, deep breath to pull the powder out and into your lungs.
DPIs are usually tube-or disk-shaped, with a mouthpiece. some have a place to load in medicine. different instructions on how to activate and use them.
some example of dry powder inhaler devices include:
- Twisthaler.
- Flexhaler.
- Diskus.
- HandiHaler
- Ellipta.
- Breezhaler.
3. soft mist inhalers
soft mist inhaler turn liquid medication into a fire mist.you breath the mist in through your mouth to get the medicine to your lungs.

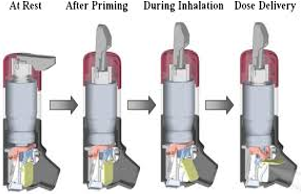
The standard MDI inhaler
MDI inhaler
A standard MDI is shown above. the MDI has been used for over 40 year and is used to deliver various types and brand of asthma medicines. it contain a pressurized inactive gas that propels a dose of medicine in each 'puff'. Each dose is released by pressing the top of the inhaler.
this type of inhaler is quick to use, small and convenient to carry. it needs good co-ordination to press the canister and breath in fully at the same time. sometimes these are known as evolvers (depending upon the manufacturer).
The standard MDI is the most widely used inhaler. however, many people do not use it to its effect. common erorinclude:
- Not making the inhaler before using it.
- Inhaling too sharply or the wrong time.
- Not holding your breath long enough after breathing in the contents.
until fairly recently, the propellant gas in MDI inhalers has been a chlorofluorocarbon (CFC) –however, due to environmental concerns these have now been phased out.
some brands of newer MDIs have much lower carbon footprint than other and many part of the country are changing patients' asthma inhalers to the type which is best for the environment. this does not affect their efficacy as an asthma inhaler.
Breath actuated MDI
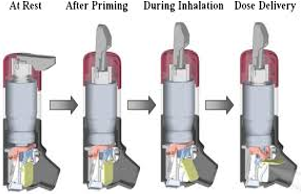
these are alternatives to the standard MDI. Some are still pressurized MDIs, but don’t need the canister on top to be pressed. theauto haler shown above is an example. another example of a breath -activated MDI is the easi-breathe inhaler.
Other breath -activated inhalers are also called dry powder inhalers. these inhalers do not contain the pressurized inactive gas to propel the medicine. A dose is triggered by breathing in at the mouthpiece.
Accuhalers, clikhalers, easyhalers, novolizer, turbohalers and twisthalers are all breath-activated dry powder inhalers.
some type3s are shown below.
accuhaler

Turbohaler

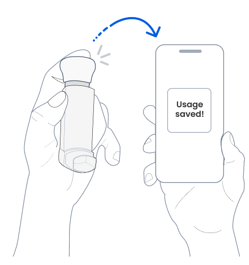
Smart inhaler
A Smart inhaler is an inhaler that technology has enhanced. A smart inhaler is an example of a digital medicine. These medical devices use technology to help collect health information. this information can help your healthcare provider make more personalized treatment decision.
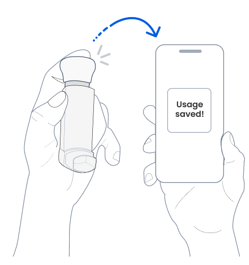
to use all a smart inhaler's features, you must link the device to corresponding app on your smartphone or mobile device. all the available smart inhalers track very dose you use. this information is then recorded in the app and can be shared with your healthcare provider.
smart inhaler can also send reminders. This can be helpful if have trouble remembering your doses. the apps for each also log use of a rescus inhaler separately from use of a mainance inhaler.

smart inhaler' networking features are essential for facilitating the smooth transfer of death to centralized platform or the system healthcare providers. These gadgets provide a connection between the patient and their care team using Bluetooth or other wireless communication protocols. this connection allows for timely interventions in addition to real-time data monitoring .automated alerts can be sent off to +provide instructions or reminder, for example, when a patient forget a dosage or use improper inhaler technique.
smart inhalers increase patient accountability and empowerment by providing real-time feedback, reminder, and personalized insights.
Benefit of smart inhalers
Integration of remote monitoring and telemedicine: smart inhalers make it possible to remotely monitor patient' asthma management, which it possible especially useful in circumstances when face-to-face visits are difficult. Through linkedplatform, healthcare clinicians may view patient inhaler usage information and symptom trends. With the use of this capacity, doctors may conduct virtual consultations without the need for in-person meeting in order to monitor patient' progress, modify treatment plans, and offer timely advice.
smart inhalers alert patient to missed or repeat doses and remind patients to take their doses on time, conveniently and automatically, depending on the time of the dose. these reminders can arrive wherever the patient is.
these devices can relieve the stress of having to remember to take medication on time, especially when there are many drugs to be remembered. They can help optimize inhalation technique and efficacy.
and finally, they track symptoms for both patient and doctors to understand how, where and when symptoms become worse, and to monitor the use of the rescue inhaler for immediate short-term relief.
How do smart inhaler work?
working with smart inhaler is simple
smart inhaler add-ons are medical devices that gather comprehensive data about every usage of inhalers. They use Bluetooth to send information to the application on the phone, which in return provides doctor or researchers with insights about asthma & COPD for better treatment.
ATTACH
put smart device on your inhaler

CONNECT
Link device with app on your phone
COLLECT
Use inhaler like before and collect data

SHARE
Get accurate treatment based on precise data
what kind of data do smart inhaler collect ?
smart inhalers collect comprehensive data about every medication usage. among others, it includes:
- medication usages
- asthma attacks occurrence
- weather conditions on inhaler use
- medication adherence
- exacerbation periods
- long term trend and statistics
How can data from smart inhalers be used?
Data from smart inhalers improves various aspects of traditional asthma & COPD care and provide opportunities for new innovation solutions;
- Remote patient monitoring
- Real-time patient screening
- Asthma exacerbations predictions
- modification of asthma & COPD therapy
- Remote treatment adjustments
- automated asthma & COPD research
- Comprehensive patient asthma & COPD history
Integrated dosing technology
Integrate dosing technology is a system that uses chemical dosing dosing pumps to accurately inject chemical into a process.
There are many types of integrated dosing technologies, including:
An Industrial equipment that accurately measures and controls the amounts of lime added to a liquid or solid material.
A system that automatically injects chemicals into a chemical feed tank for wastewater treatment. During the dosing process, chemicals are added to the water stream at precisely controlled rates by chemical metering pumps.
A positive displacement pump that injects chemical liquids into a water or gas stream at a precise flow rate.
A system that uses volumetric measurements to dispense bulk ingredients.
- Antiscalant dosing system
A system used for dosing industrial production water to prevent minerals and impurities
A system that ensures the right amount of detergent is used for each wash in commercial washing machine
A system used for the precise and controlled dosing of multiple chemical or substance.
A dosing pump is a central part of an integrated dosing system that injects a chemical or other substance into a flow of water , gas, or steam.

A seal with integrated dosing system that can be applied directly to bottles designed to hold liquid oral medications.
A solution for :

Integrating dosing and containment function into a single system
One-handed dosing of liquid oral medications

Simplifying the timing of taking the medicine
How it works
Andy is a seal with a dispensing function that is compatible with major pharmaceutical bottle mouthpieces. Once screwed onto the bottle, simply turn it upside down on a flat surface and apply a light pressure to the bottom. This action will allow the liquid to flow into the dosing chamber, where –through level markings the different capacities are clearly indicate. Thanks to a flip-top closure, it is possible to open the container with one hand and consume the medicine directly from a special spout.
REFERENCES
- lee j, McDonald C. Review: immunotherapy improves some symptoms and reduces long-term medication use in mild to moderate asthma. Ann Intern Med.2018 Aug 21;169(4):JC17
- public health agency of Canada: life and breath: respiratory disease in Canada. Ottawa, Ontario; 2007, available: http://www.phac-aspc.gc.ca/publicat/2007/ lbrdc-vsmrc/index–eng.php Accessed July 15,2010.
- Bourdin A, Gras D, Vachier l, chanez p: Upper airway 1: allergic rhinitis and asthma: united disease through epithelial cell. Thorax 2009, 64:999-1004.
- global initiative for asthma (GINS): Global strategy for asthma management and prevention. 2009 available at: http://www.ginasthma.com accessed July 15,2010.
- FitzGerald JM, boulet LP, McIvor RA, Zimmerman S, Chapman KR Asthma control in Canada remains suboptimal: the reality of asthma control (RAC study. Can Respir J 2006, 13:253-259.
- lemanske RF, busse WW: Asthma: clinical expression and molecular mechanisms. J Allergy Clin immunol 2010, 125:S95-102.
- kalpan AG, Balter MS, Bell AD, Kim H, Mclvor RA: Dignosis of asthma in adult. CMAJ 2009, 181: E210-E220.
- Kovesi T, Schuh S, spier S, Berube D, Carr S, Watson W, Mclvoe RA:Achieving control of asthma in preschoolers. CMAJ 2010, 182:E172-E183.
- Tesfaye ZT, Gebreselase NT, Horsa BA. Appropriateness of chronic asthma management and medication adherence in patient visiting ambulatory clinical of Gonder University Hospital: a cross- sectional study. World Allergy Organ j. 2018;11(1):18. (PMC free article) (pubMed)
- Salo PM, Cohn RD, Zeldin DC. Bedroom Allergen Exposure Beyond House Dust Mites. Curr Allergy Asthma Rep. 2018 Aug(10):52. (PMC free article) (PubMed)
- Piloni D, TIrelli C, Domenica RD, Conio V, Grosso A, Ronzoni V, Atonacci F, Totaro P, Corsico AG. Asthma-like symptoms: is always a pulmonary issue? Multidiscip Respire Med. 2018;13:21. (PMC free article) (PubMed)
- aggarwal B, Mulgirigama A, Berend N. Exercise-induced bronchoconstriction: prevalence, pathophysiology, patient impact, diagnosisand management. NPJ prim Care Respir Med. 2018 Aug 14;28(1): 31. (PMC free article) (PubMed)
- parnes JR, Molfino NA, Colic G, Martin U, Corren J, Mnzies-GOW a. Targeting asthma. J asthma Allergy. 2022;15:749-769. (PMC free article) (PubMed)
- Litonjua AA, Weiss ST. Is vitamin D deficiency to blame for the asthma epidemic? J Allergy Clin Immunol. 2007 Nov;120(5): 1031-5. (PubMad)
- cremer NM, Baptist AP. Race and Asthma Outcomes in Older Adults: Results from the National Asthma Survey. Allrgy Clin Immunol Pract.2020 Apr; 8(4):1294-1301.e7. (PubMed)
- song WJ, Lee JH, Kang Y, Joung WJ, Chung KF. Future Risks in patients with severe Asthma. Allergy Asthma Immunol Res. 2019 Nov; 11(6): 769-778. (PMC free article) (PubMed)
- Knightly R, Milan SJ, Hughes R, Knopp-Sihota JA, rowe BH, Normansell R, Powell C. Inhaled magnesium Sulfate in the treatment of acute asthma. Cochrane Database Syst Rev. 2017 Nov 28;11(11): CD003898. (PMC free article) (PubMed)
- Alison JA, McKeough ZJ, Johnston K, et al. Australian and New Zealand pulmonary rehabilitation guidelines. Respirology. Respirology. 2017;22(4):800-19. https://doi.org/10.1111/resp. 13025.DOI-pubMed
- spruit MA, Singh SJ, Garvey C, et al. AN official American thoracic society/European respiratory society statement: key concepts and advances in pulmonary rehabilitation. Am J Respir Crit Care Med. 2013: 188(8):13-64 .https://doi.org/10.1164/rccm.201309-1634ST.
- Jansen EM, van de Hei SJ, DIerick BjH, Kerstjens HAM, Kocks JWH, van Boven JFM. Global burden of medication non-adherence in chronic obstructive pulmonary disease (COPD) and asthma: a narrative review of the clinical and economic case for smart inhaler. J Thorac Dis. 2021 jun 1; 13(6): 3846.
- Margam R. The Importance of HER in revolutionizing Healthcare Delivery and Financial success. Artic Int J Comput Trends Technol. 2023;71: 52-5.
- vestbo J, Calveley P, Celli B, Ferguson G, Jenkins C, Jones P, et al. The TORCH (Toward a Revolution in COPD Health) survival study protocol. Eur Respire J. 2004; 24(2): 206-10.
- Taylor TE, Mols HL, Costello RW, Reilly RB. Estimation of inhalation flow profile using audio-based methods to assess inhaler medication adherence. PLoS One. 2018 Jan 1;13(1)
- chan AHY, stewart AW, Harrison J, Camargo CA, Black PN, Mitchell EA. The effect of an electronic monitoring device with audiovisual reminder function on adherence to inhaled corticosteroids and school attendance in children with asthma: A randomized controlled trial. Lancet Respir Med.2015 Mar 1:3(3):2010-9.
- Margam R. Importance of Cyber security in Electronic Health Records. Int J Innov Sci Res Technol.2023;8(7).
- Gibson PG, McDonald VM. Management of severe asthma: targeting the airways, comorbidities and risk factors.Intern MedJ.2017 Jun 1;47(6):623-31.
- kumar p, Sharma SK, Dutot V. Artificial intelligence (AI)-enabled CRM capability in healthcare: The impact on service innovation .Int J Inf Manage. 2023 Apr 1;69.
- Lidsromer N. Ashrafian H. Artificial Intelligence in Medicine. Artif Intell Med. 2022 Jan 1,1- 1858.
- Islam SMR, Kwak D, Kabir MH, Hossain M, Kwak KS. The internet of things for health care: A comprehensive Survey. IEEE Access. 2015 Jun 1;3:678-801.
- Minh Dang L, Piran MJ, Han D, Min K, Moon H. A survey on Internet of Things and cloud Computing for healthcare. Electron2019, Vol 8, page 768. 2019 July 9; 8(7)768.
- Van Gemert F, Van der Molen T, jones R, et al. The impact of asthma and COPD in sub-saharan Africa. Prime Care Respire j 2011;11:20:240-248.
- mphahlele RE, Kitchin O, Maskela R. Barriers and determinants of asthma control in children and adolescents inafrica: a systematic review. BMJ open 2021;11:e053100.
- world asthma report. 2018. Accessed 31 December 2023. http://ginasthma.org/wp-content/uploads/2022/07/GINA-Main-report-2022-FINAL-22-07-01-WMS.pdf.
- Krebs p, Duncan DT. Health App Use Among US Mobile Phone Owners: A National Survey. JMIR mHealth uHealth. 2015 Nov 4;3(4):e101.
- Chrystyn H, Audibert R, Keller M, Quaglia B, Vecellio L,Roche N.Real-life inhaler adherence and technique: Time to get smarter! Respir Med. 2019 Oct 1;158:2432.
- Roche N, Dekhijizen PRN. The evolution of pressurized metered- dose inhaler form early to modern device . J Aerosol Med Pulm Drug Deliv.2016 Aug 1;29(4):311-27.
- Honkoop P, Usmani O, Bonini M. The Current and Future Role of Technology in Respiratory Care, Pulm Ther. 2022 Jun 1;8(2):167-79
- Maken P, Gupta a, Gupta MK. A systematic review of the techniques for automatic segmentation of the human upper airway using Volumetric images. Med Biol Eng Comput. 2023 Aug 1;61(8): 1901-27.
- sorino C, Negri S, Spanevello A, Visca D, Scichilone N. Inhalation therapy devices for the treatment of abstractive lung diseases: the history of inhalers towards the ideal inhaler. Eur J Intern Med. 2020 May 1;75:15-8.
- Chapman KR, Barnes NC, Greening AP, Jones PW, Pedersen’s. Single maintenance and reliever therapy of asthma: a critical appraisal. Thorax. 2010 Aug;65(8): 747-52.
- Reddel HK, Bateman ED, Schatz M, Krishna JA, Cloutier MM. A practical Guide to Implementing SMART in Asthma Management J allergy Clin Immunol Pract. 2022 Jan 1;10(1ws):s31-8
- Howard S, Lang a, Patel M, Sharples S, Shaw D. Electronic Monitoring of Adhrence to inhaled medication in Asthma.
- Ioniuc I, Miron I, Lipu VV , Starcea IM, Azoicai A, Alexoae M, at al. Challenges in the pharmacotherapeutic Management of Pediatric Asthma. Pharmaceutical (basel). 2022.Dec 18;15(12).
- Zabczyk C, Blakey JD. The Effect of Connected ‘smart’ inhalers on Medication Adherence. Front Med Technol. 2021;3.


 Atharva Patil *
Atharva Patil *
 Yamini bisen
Yamini bisen
 Nikam harshada
Nikam harshada










 10.5281/zenodo.14029848
10.5281/zenodo.14029848