Abstract
Acne vulgaris is one of the most common dermatological disorders that afflict people in their adolescence, Acne vulgaris or simply known. As acne is a human skin disease characterized by skin with red skin (seborrhoea), blackhead and whiteheads (comedones), pinheads (papules), large papules (nodules), pimples and scarring. Acne vulgaris is a disease of pilosebaceous unit characterized by the formation of open and closed comedons, papules, pustules, nodules and cyst. Acne affect skin having dense sebaceous follicle in area including face. Acne affects physiological status and social activities. The present review focuses on epidemiology, etiology, pathogenesis, diagnosis, differential diagnosis and management of acne with pharmaceutical dosage forms of oral and topical administrations. Various medicines for acne treatment include benzoyl peroxide, antibiotics, anti-seborrheic medicine, sulphur and sodium sulfacetamide, anti-androgen medication, salicylic acid, hormonal treatment, alpha hydroxy acid, retinoids, azelaic acid, keratolytic soaps and nicotinamide. Currently laser and light devices and mirror subcision surgery have been also performed for acne treatment.
Keywords
Acne vulgaris, comedons, pilosebaceous unit, laser treatment.
Introduction
Acne vulgaris or simply known acne is a human skin disease characterized by skin(seborrhea), blackheads and whiteheads (comedons) pinhead (papules), large papules (nodules), pimple and scarring. Acne affect skin having dense sebaceous follicle in areas including face, chest and back. Acne may be inflammatory or non-inflammatory form. Due to change in pilosebaceous lesions are caused by androgen stimulation. Acne occurs commonly during adolescence affecting about 80-90% of teenagers in western world and low rate in rural societies.

Acne is usually caused by increase in androgen level like testosterone mainly during puberty in both male and female. Acne reduces over the time and tends to disappear over the age. The lesion called cyst and severe inflammatory acne called as nodulocystic. The cystic acne occurs on buttocks, armpit area, hair follicle and perspiration duct and affect the deeper skin tissue than common acne. Acne causes scarring and psychological effect such as reduced self-esteem and in rare case depression or in some case the attempt of suicide. The word refers to the presence of papules, scars, comedons and pustules. The common form of acne is known as ‘Acne vulgaris’. Many teenagers suffer from this type of acne. Acne vulgaris shows the presence of comedons. Acne rosacea is synonym of rosacea and some person not have acne comedons associated with their rosacea, hence prefer the term.
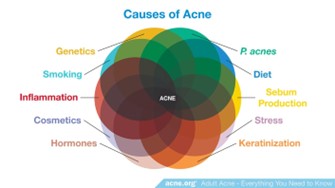
Etiology:
Acne develops when the hypersensitivity of the sebaceous glands to normal level of androgen. This process further processed by the Cutibacterium acne (C acne) which is a type of bacteria and causes inflammation which further causes acne.
Factors responsible for acne:
- Medication
- Excess exposure of UV-rays or sunlight
- Tight wear
- Oily products such as oily cosmetic products
- Disbalance of endocrine system
- Menstrual disorders
- Genetic
- Allergy of soap and detergent
- Increase in milk consumption and high glycaemic foods
- Psychological problem such as stress and anxiety and stimulating stress hormone
- Some insulin resistance may have role in acne formation [1]
Epidemiology:
Acne vulgaris affects approximately 9.4% of the global population, typically emerging during puberty due to hormonal changes. Its most prevalent among adolescences and young adults, with its occurrence declining as individual age. Although rare acne can manifest in newborn and develop later in adulthood. The prevalence of acne in boys rise from 40% at age 12 to 95% at age 16, and I girls it increases from 61% to 83% during the same period. While males tend to experience more severe form of acne during adolescence, females are more commonly affected in adulthood. Mild acne is predominant among Caucasians, while Asians and Africans are more prone to severe cases.
Increasing evidence suggests that diet play a role in acne development. A 2021 systematic review of 53 studies, including 11 interventional clinical trials and 42 observational studies, revealed that a diet high in glycemic load, foods with a high glycemic index, dairy products, chocolates, and fatty acid foods are linked to acne development. Conversely, fatty acids, vegetables, and fruits are associated with lower acne risk. Additionally, vitamin D deficiency, high-dose vitamin B6 and B12 supplements, and whey protein supplements may also contribute to acne. Other predisposing factors include genetic susceptibility (family history of severe acne) and obesity. Factors contributing to acne include oily or seborrheic skin, elevated skin surface pH, emotional stress, repetitive mechanical trauma, excessive sunlight exposure, pre-menstruation, mechanical obstruction (such as headband, shoulder pads, surgical marks, N95 respirators), use of greasy or occlusive skin care product, certain medications (such as anabolic steroids, hydantoin, benzodiazepines, ramipril, adalimumab, cyclosporin, isoniazid, lithium, iodides), congenital adrenal hyperplasia, adrenal tumours, polycystic ovarian syndrome, and body dysmorphic disorders. [2]
Causative factors and pathogenesis of acne vulgaris:
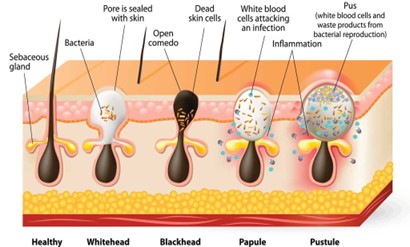
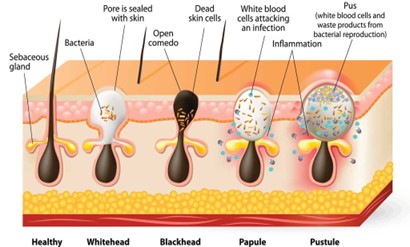
Numerous factors are thought to be pivotal in the classical development of acne vulgaris. As previously mentioned, persistent acne condition stem from heightened sebum production, endocrine influence like androgen, irregular keratinization of follicular opening, proliferation of bacterial infections, and ensuing inflammation.
Elevated sebum production:
elevated sebum production within hair follicles stands out as primary driver of acne development. According to goll nick et al. highlight the role of androgen hormones, particularly testosterone and insulin growth hormone (IGH-1), in stimulating sebum synthesis and secretion. The correlation between heightened sebum production and the intensity and recurrence of acne lesions underscores its importance in the assessment of individual with acne vulgaris.
Abnormalities in keratinization within the pilosebaceous follicles:
In individual with acne, there are abnormalities in the shedding of keratinocytes within the pilosebaceous follicles. Normally, healthy follicles shed single keratinocytes into follicular lumen, where they are eliminated. However, in acne patients, there is excessive proliferation of keratinocytes, which result in their failure to shed into the lumen. This led to accumulation of irregularly desquamated corneocytes within the pilosebaceous follicles, along with lipid and monofilaments.
Propionibacterium acne:
The cutaneous microbiota may contribute to acne pathogenesis. A metagenomic analysis revealed similar level of Propionibacterium acne on the skin of acne patients and healthy individuals, but with different strain population. Certain strain of P. acnes strains exhibits varying inflammatory potential, with type 3 being the most pro-inflammatory. Specific strains may exacerbate acne lesions through infections, an area under ongoing investigations. P. acnes and its associated antigens, particularly lipopolysaccharides, increase the expression of pro-inflammatory cytokines in sebocytes. P. acnes include IL-8 and TNF, while lipopolysaccharide induce IL-8, TNF, and IL-10. Viable p. acnes stimulate the release of IL-8, IL-11, IL-13, and granulocytes-macrophage colony stimulating factor, whereas heat killed organisms do not. Additionally, P. acne induces IL-17 expression in peripheral blood mononuclear cell, with IL-17 positive cell presents around comedones. P. acne can activate T-17 and T-1 response pathways, observed in acne lesions, by inducing IL-17A and IFNy secretion from CD4+ T cells. Moreover, P. acnes triggers NLRP3 inflammasome activation in monocytes, macrophages and sebocytes.
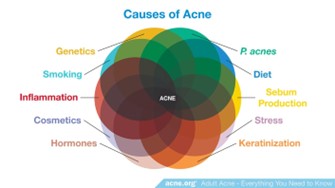
Contemporary way of life, dietary habits, and tobacco use:
The modern lifestyle, encompassing factors such as dietary choices, stress, urban noise, socioeconomic pressure, exposure to light stimuli, and variation in sleep patterns, poses a potential risk for acne development. Dietary habits can provide substrate for the synthesis of sebaceous lipids, including essential fatty acids like linolic acid. Low glycemic load diets may decrease sebum production through hormonal effects, whereas typical western diets can exacerbate acne. Severe caloric restriction can reduce sebum excretion, which can be reversed by returning to a normal diet. Alteration in dietary fat or carbohydrate intake can also influence sebum production and composition. The absence of acne in indigenous nonwestern populations in Papua New Guinea and Paraguay further support this idea. Additionally, patients with severe acne have higher level of total cholesterol, lowdensity lipoprotein (LDL), high density lipoprotein (HDL), and apolipoprotein A1 compared to healthy, age-matched controls; however, these levels remain within the normal range. The role of smoking in acne development remains uncertain. While some studies have found a positive association between smoking, the numbers of cigarettes smoked daily, and acne occurrence, other have reported no correlation or even suggested a protective effect of smoking. Smoking may potentially induce acne by increasing oxidative stress, leading to accumulation of lipid peroxide in comedones and triggering inflammation signaling pathways dependent on phospholipase A2. Certain medication such as anti-epileptic drugs and anticancer medications like tyrosine kinase inhibitors, can also cause monomorphic acne or acneiform eruptions, which resembles acne vulgaris. Additionally, the use of anabolic drugs is known to induce severe form of acne. Exposure to dioxin can result in severe comedonal acne known as chloracne.
The psychological and social impact:
Older literature suggests stress alone is unlikely to cause acne lesion to form. However, recent research indicates that stress may indeed contribute to acne development. Additionally, acne itself can cause stress, and picking at the spot can worsen the appearance, leading to a condition called acne excoriation, particularly common in emotionally stressed adolescent girls. Despite its prevalence, acne excoriation typically resolves on its own. Appearance plays a significant role in social and emotional well-being, with people often forming initial impressions based on facial appearance. Motely and Finaly were surprised to find little correlation between many psychological factors and acne severity. Their study showed that patients did not report feeling more self-conscious or lacking confidence compared to their peers.
Genetic role:
Genetic significantly influences acne development, as evidenced by numerous studies. Those with affected immediate family members are up to 3 times more likely to develop acne compared to those without a family history. Additionally, gene expression studies have shown increased level of certain proteins and peptides in acne lesions, indicating a genetic basis for the condition. [1,3,4,5,6,7]
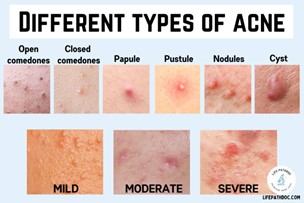
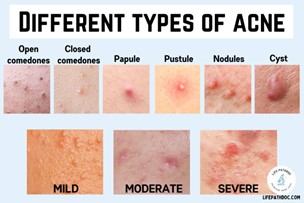
Diagnosis and assessment:
The identification of the quantity and characteristics of lesions typically forms the basis for diagnosing acne vulgaris(av). Lesions are categorized into non-inflammatory comedones, referred to as open(blackheads) or closed(whiteheads), and inflammatory lesions, including papules, pustules, cysts, or nodules. The American academy of dermatology (AAD) classified acne severity into three categories: mild, moderate and severe. Mild acne is characterized by a few to several papules and pustules along with a few nodules. Severe acne presents with numerous or extensive papules and pustules, as well as multiple nodules.
Different form of acne blemishes:
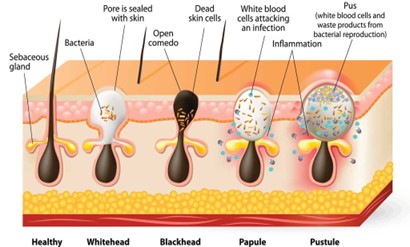
Acne manifests in various forms, such as acne conglobata, acne rosacea, acne fulminans, acne cosmetica, acne excoriee (pickers acne), acne medicamentosa, acne chloracne, and acne mechanica. However, acne vulgaris, comprising 99% of cases, is most common type, characterized by non-inflammatory comedones (open and closed) and inflammatory papules, pustules, nodules, and cyst. Closed comedones are known as whiteheads, while open comedones are referred to as blackheads. [3]
Blackheads:
Blackheads are non-inflammatory acne blemishes formed by excess oil and dead skin cells clogging hair follicles. They’re called open comedones because the skin remains exposed, appearing dark, often black and brown. Typically, mid, blackheads commonly occur on the face, arm, chest, neck, back, and shoulders.
whiteheads:
Whiteheads are tiny, non-inflammatory acne bumps caused by a blockage of oil, bacteria, and skin cells in hair follicle pores. They’re termed closed comedones because the bumps are closed and white in color. While they can appear anywhere on the body, whiteheads are most common in t-zone, which comprises the nose, chin, and forehead.
Papules:
Inflammation occurs when healthy skin reacts to bacteria, excessive oil, and increased androgen activity, resulting in swelling, heat, redness, and pain. Papules, which are inflamed lesion, serves as an intermediary stage between noninflammatory and inflammatory lesions. They appear as small pink lumps on the skin, usually less than 5mm in diameter and are not filled with pus.
Pustules:
Pustules are small, inflamed bumps caused by clogged pores with excess oil and dead skin cells. They contain fluid or pus at their center and typically appear as white pimples surrounded by red, irritated skin. While they can form anywhere on the body, pustules are most common on the shoulders, chest, back, face, neck, underarms, pubic region, and hairlines
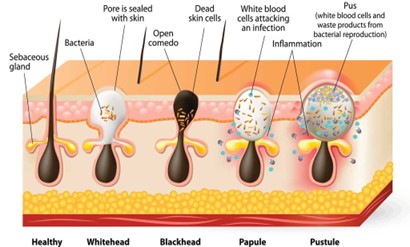
Nodules:
Nodular acne, a severe form of inflammatory acne, arises from clogged pores due to bacteria, excess oil, and dead skin cells. Unlike typical comedones, this infection penetrates deep, causing red, swollen, bumps beneath the skin surface. Over-the counter medications may not suffice, and nodules can persist for weeks or months. Larger than 5-10 mm, they often appear on the jawline or chin.
Cysts:
Cystic acne, a severe form of inflammatory acne, develops beneath the skin cells, and oil buildup. It commonly affects people of all ages with oily skin and manifest as large, painful white or red lesions filled with pus, often leading to scarring. While it can appear anywhere on the body, its most frequent on the face, arms, shoulder, back, chest, and neck. Those with cystic acne often experience both inflammatory and non-inflammatory symptoms. [3]
Impact of acne in Life:
According to a study that acne vulgaris had moderate impact on quality of life of patients and the effect was more on female patients, as compared to males. This was evidenced by a higher score among female participants, though it was not statistically significant. The result of study shows that there is need to educate the patients, as well as peer groups, about the reason for acne so as to encourage early treatment. The study also highlights that we need to be compassionate when dealing with patients of acne vulgaris. [8]
Treatments:
Principle of treatment of Acne vulgaris:
Acne treatment begins with education, discussing the cause and therapy goals. Patient should understand that mild cases can last 4-6 years, while severe cases may persist over 12 years. If oral antibiotics and topical treatment don’t work, oral isotretinoin is highly effective and likely to be prescribed. [7]
Therapeutic options:
The severity and extent of the disease largely dedicate the approach. Mild acne typically requires only topical therapy, while moderate cases benefit from both oral and topical treatments. Severe acne warrants immediate oral isotretinoin.
Various treatment modalities:
Skin hygiene:
Patients should opt for gentle skin cleansers instead of harsh scrubs and soaps, along with non-comedogenic skincare products. Patting the face dry after washing is recommended, avoiding aggressive scrubbing and picking of acne lesions to prevent scarring. Using soap-free face wash and oil-free moisturizers and sunscreen is also advisable. [2]
Topical treatment;
Topical medications take center stage in acne treatment, with common options like benzoyl peroxide, clindamycin, and retinoids.
Benzoyl peroxide (BP):
BP is widely used topical medication for acne vulgaris (AV). It decreases P. acne colonization and inflammation, with additional effects on keratolysis and sebum production. Its bactericidal and stable for treating comedonal acne, available in concentrations of 2.5%, 5%, and 10%. The FDA classifies BP as pregnancy risk category.
Retinoids:
Topical retinoids are the go-to-first choice for treating both noninflammatory and inflammatory acne. They work by reducing sebum production, regulating comedone growth, repairing damage skin, addressing hyperpigmentation and scarring, and controlling acne lesions. However, the treatment takes over three months to show results and can cause dryness and skin irritation. Tretinoin, adapalene, and tazarotene, retinaldehyde are commonly used retinoids for acne treatment. [3]
Antimicrobial:
Topical antibiotics are typically prescribed for mild to moderate inflammatory acne, targeting P. acne bacteria on the skins surface to reduce inflammation. However, due to their limited effectiveness and side effects, not all antibiotics like chloramphenicol and tetracycline are used. Erythromycin and clindamycin are the most common choices. Combining topical antibiotics with benzoyl peroxide and retinoids is more effective in preventing bacterial resistance than using them alone. These antibiotics directly reduce P. acnes colonization and inflammation when applied to the skin. Ex. Erythromycin, clindamycin etc.
Systemic treatments:
Topical retinoids should be the initial treatment choice for acne since micro comedones contribute significantly to both inflammatory and noninflammatory lesions. If topical treatment fails or acne presents as nodular lesions or scarring, oral treatments, including oral antibiotics, hormonal medications, and isotretinoin, are crucial for preventing the social and psychological distress associated with acne.
Retinoids:
Isotretinoin, a vitamin A derivative, is primarily used in systemic treatment for severe nodular or inflammatory acne and is considered a first-line option. Its effective for patients with mild to moderate acne who haven’t responded to other medications. Isotretinoin targets all four causes of acne, reducing sebum production, altering bacterial flora, and promoting shedding of keratinocytes. Treatment usually lasts 16-24 weeks but requires close monitoring due to potential adverse effects.
Antibiotics:
Oral antibiotics are typically prescribed for moderate to severe, inflammatory acne resistant to topical treatments or covering large areas of the body. Commonly used antibiotics include erythromycin, clindamycin, azithromycin, and tetracyclines like doxycycline and minocycline. These drugs inhibit P. acne growth and inflammatory mediators. Tetracyclines are popular due to their effectiveness, anti-inflammatory properties, and affordability. Doxycycline and minocycline are preferred for their better penetration into the skin and lower gastrointestinal side effects. However, there’s insufficient evidence to prove their superiority over tetracyclines, which also show less resistance development in P. acne. Limited research exists on the effectiveness of azithromycin for acne treatment. Erythromycin and clindamycin have minimal anti-inflammatory effects, reducing P. acnes levels. However, long term use can lead to resistance, limiting their efficacy. Combination therapy, such as pairing oral antibiotics with topical benzoyl peroxide or retinoids, is now preferred to enhance effectiveness and reduce resistance. Treatment duration typically lasts 12 weeks.
Hormonal drugs:
Hormonal treatment, often using oral contraceptive pills, is an alternative for treating acne in adult females and adolescents. These pills inhibit sebum production stimulated by testosterone and reduce the amount of active free testosterone in the body. Hormonal therapy can be used alone or in combination with other treatments. The beneficial effect usually become evident after 3-6 months of treatment, with a recommended duration of at least 12 months for hormonal anti-androgens. Spironolactone, an androgen receptor blocker, is sometimes combined with oral contraceptive to reduce acne-related inflammation in females. [3]
Other treatments:
Complementary treatments:
Comedones extraction can help with resistant comedones but should be used alongside conventional medication. Microdermabrasion and chemical peeling with glycolic acid or salicylic acid lack sufficient medical evidence for acne management and require further studies. Intralesional steroid injections appears effective for nodular acne but needs structured studies for proper dosage determination. Consideration of potential adverse effects of steroids is crucial before therapy. Systemic steroid can be used with isotretinoin as primary therapy in severe acne cases with systemic signs, such as acne fulminans.
Treatment of acne by light:
Light therapy methods for acne treatment include various sources like broad-spectrum visible light, lasers, and photodynamic therapy. They work by inhibiting P. acnes bacteria and/or damaging sebaceous gland. Photodynamic therapy involves applying a photosensitizing agent followed by exposure to light sources. Low-dose photodynamic therapy shows short-term effect through antimicrobial or immunomodulatory actions, while high-dose therapy destroys sebaceous glands for longer-term effects. Aminolaevulinic acid followed by red light is optimal, especially for non-inflammatory lesions. Adverse effects are generally mild and transient, but caution is needed with dark skin. Light therapies are not highly effective alone but be useful as adjuncts to medical therapies or for patients who prefer non-medical treatments. More evidence is needed to fully define their efficacy.
Alternate drugs:
Several natural products have been studied for acne treatment. Topical azelaic acid (27%) applied twice daily for six month is effective for mild to moderate acne, comparable to benzoyl peroxide, isotretinoin, and erythromycin. However, it may cause skin irritation. Tea tree oil is also effective when applied topically for acne treatment. A vaccine tested successfully in mice against inflammatory acne awaits confirmation in humans. Genome sequencing of P. acnes bacteriophage therapy for acne, potentially addressing long-term antibiotic therapy and bacterial resistance issues.
CONCLUSION:
Acne is a common inflammatory skin condition that often leads to depression and social embarrassment, particularly in adults. Understanding its key pathogenic factor is crucial for developing effective therapies. While traditional treatments like topical and systemic medication are well-known, drug resistance remains a challenge. Monotherapy approaches are not always effective, prompting the search for innovative drug candidates and combination therapies. Laser and light treatments, along with minor surgeries, offer additional options. Genome sequencing advancements hold promise for future bacteriophage therapies. Overall, a comprehensive approach is essential for managing acne effectively, considering both existing and emerging studies.
REFERENCES:
- Sutaria AH et al. Acne vulgaris. StatPearls Publishing; 2024 Jan
- Alexander KC Leung et al. Dermatology: how to manage acne vulgaris. Drug in context. 2021; 10:2021-8-6
- Mallikarjun vasam et al. Acne vulgaris: a review of the pathophysiology, treatment, and recent nanotechnology-based advances. Biochemistry and biophysics reports, volume 36, December 2023, 101578.
- Sara Moradi tuchayi et al. Acne vulgaris. Nature reviews Disease Primer, September 2015, article number: 15029
- Manoj Suva et al. A brief review on acne vulgaris: Pathogenesis, diagnosis and treatment. Research and reviews: journal of pharmacology Jan 2015. ISSN:22309861, volume 4, Issue 3
- Febyan et al. Acne vulgaris in adults: A brief review on diagnosis and management. International journal of Research and review, vol.7; Issue 5; May 2020
- Mukesh Kumar Chaudhary A review on treatment options for acne vulgaris. world journal of pharmacy and pharmaceutical sciences. Volume 5, Issue 7, 524-545, June 2016.
- Amit Batra et al. To study the impact of acne vulgaris on the quality of life of patients, university of Toronto medical journal. Volume 92, number 1, December 2014.
- Balaji adityan et al. Profile of acne vulgaris- A hospital-based study from south India. Indian Journal of dermatology venerology and leprology. May-June 2009, vol 75, issue 3.
- Manjunath hulmani et al. Knowledge, attitude and practice towards acne vulgaris among acne patients. International journal of research in dermatology. 2017 march;3(1):107-112
- S.K. Janani and Raman Sureshkumar, international journal of pharmaceutical sciences and research, 2019; vol. 10(7): 3155-3177.
- Ak Mohiuddin, A comprehensive review of acne vulgaris, clinical research in in dermatology: open access, ISSN Online: 2378-1726, June 17, 2019.
- K. kameswararao et al. A brief review on acne vulgaris. Research journal of pharmacology and pharmacodynamics, vol. 11, issue-03, July September 2019.
- Andrea L. Zaenglein et al. Guidelines of care for the management of acne vulgaris. American academy of dermatology, Inc. Published by Elsevier, feb 17, 2016. Volume 74, number 5.
- John S. Barbieri et al. Trends in oral antibiotic prescription in dermatology, 2008 to 2016. Jama dermatology, 2019 Mar; 155(3): 290-297.
- James J. Leyden, New understanding f the pathogenesis of acne, journal of American Academy of dermatology, may 1995, volume 32, number 5, Part 3.
- Hirohiko Akamatsu et al. Control of human sebocyte proliferation in vitro by Testosterone and 5-Alpha-Dihydrotestosterone is dependent on the localization of sebaceous glands. The journal of investigative dermatology vol. 99, no. 04 October 1992.
- Siri Knutsen-Larson et al. Acne vulgaris: Pathogenesis, Treatment, and needs Assessment. Department of dermatology. 30(2012) 99-106.
- Sanjay K Rathi, Acne vulgaris treatment: the current scenario Indian journal of dermatology. 2011 Jan;56(1):7-13.
- James J Leyden et al. Propionibacterium levels in patients with and without acne vulgaris. The journal of investigative dermatology, Oct 1975, vol. 65, no. 04.


 Piyush Lekhraj Yadav*
Piyush Lekhraj Yadav*
 Prajakta Dattatraya Gawade
Prajakta Dattatraya Gawade
 Manasi Vishwas Shelke
Manasi Vishwas Shelke
 Rahul Rakesh Vishwakarma
Rahul Rakesh Vishwakarma
 Harshal Ashok Vishe
Harshal Ashok Vishe

 10.5281/zenodo.13921575
10.5281/zenodo.13921575