Abstract
Nanotechnology has emerged as a revolutionary force in the field of pharmaceutics, presenting unprecedented opportunities for enhancing drug delivery and therapeutic outcomes. This comprehensive review explores the multifaceted applications of nanotechnology in pharmaceutics, spanning from innovative drug delivery systems to diagnostic and therapeutic modalities. The article delves into the principles underpinning nanoscale formulations, emphasizing their potential to overcome challenges associated with traditional drug delivery. Nano carriers, such as liposomes, nanoparticles, and dendrimers, are dissected for their unique abilities to improve drug solubility, bioavailability, and targeted delivery. Moreover, the review scrutinizes the integration of nanotechnology in diagnostics, exemplifying the convergence of imaging and therapeutic functionalities within a single Nano platform. Key considerations, including biocompatibility, toxicity, and regulatory aspects, are critically assessed to provide a holistic understanding of the translational potential of nanotechnology in pharmaceutics. The article concludes by envisioning future directions and challenges, highlighting the transformative impact of nanotechnology on the landscape of pharmaceutical research and development.
Keywords
A review on Nanotechnology as Transformative Paradigms in Drug Delivery and Therapeutics.
Introduction
In the dynamic realm of pharmaceutics, the integration of nanotechnology has emerged as a ground-breaking frontier, promising transformative shifts in drug delivery and therapeutic strategies. Nanotechnology, operating at the nanoscale, harnesses the unique properties exhibited by materials at this level, presenting novel opportunities to address longstanding challenges in the field. This review embarks on an exploration of the multifaceted role played by nanotechnology in pharmaceutics, focusing on its potential to revolutionize drug delivery systems and redefine therapeutic paradigms Traditional drug delivery approaches have faced hurdles related to poor bioavailability, non-specific targeting, and inadequate solubility, limiting the efficacy of pharmaceutical interventions. The advent of nanotechnology offers a panoply of solutions to these issues, providing a platform for the design and implementation of advanced drug delivery systems. Nanoscale carriers, such as liposomes, nanoparticles, and dendrimers, have demonstrated exceptional capabilities in enhancing drug solubility, prolonging circulation times, and enabling targeted delivery to specific tissues or cells. This exploration will delve into the fundamental principles governing nanotechnology in pharmaceutics, dissecting the intricate interactions between Nano carriers and biological systems. By unravelling these mechanisms, we aim to elucidate how nanotechnology can overcome traditional constraints, fostering a deeper understanding of its potential applications in therapeutic interventions. Beyond drug delivery, nanotechnology has paved the way for innovative diagnostic and therapeutic modalities, blurring the lines between imaging and treatment. The convergence of diagnostics and therapeutics within a single Nano platform opens new avenues for precision medicine, promising more effective and personalized healthcare solutions. As we embark on this exploration, it is imperative to acknowledge the ethical, safety, and regulatory dimensions that accompany the integration of nanotechnology into pharmaceutical practices. This review aims to provide a comprehensive overview of the current state of nanotechnology in pharmaceutics, offering insights into its potential applications, challenges, and future directions. By examining the transformative impact of nanotechnology on drug delivery and therapeutics, we endeavour to contribute to the evolving landscape of pharmaceutical research and development, where the minuscule becomes monumental in shaping the future of medicine.
History of nanotechnology [4, 7] Long some time recently the time of nanotechnology, individuals were unconsciously coming over different Nano sized objects and utilizing Nano-level forms. In old Egypt, colouring hair in dark was common and was for a long time accepted to be based on plant items such as henna. Be that as it may, later investigate on hair tests from old Egyptian burial destinations appeared that hair was colored with glue from lime, lead oxide, and water. In this colouring handle, galenite (lead sulphide, PBS) nanoparticles are shaped. The antiquated Egyptians were able to form the colouring glue respond with sulphur (portion of hair keratin) and deliver little PBS nanoparticles which given indeed and steady dyeing. Likely the foremost popular illustration for the old utilize of nanotechnology is the Lycurgus Glass (fourth century CE). This antiquated roman container has unordinary optical properties; it changes its colour based on the area of the light source. In normal light, the container is green, but when it is lit up from inside (with a candle), it gets to be ruddy. The later investigation of this glass appeared that it contains 50–100 nm Au and Ag nanoparticles, which are dependable for the bizarre colouring of the glass through the impacts of Plasmon excitation of electrons. The antiquated utilize of nanotechnology does not halt here, in reality, there's prove for the early utilize of nanotechnology forms in Mesopotamia, Old India, and the Maya.
Challenges occurred due to current drug delivery systems [2]
Current drug delivery systems face several challenges, including issues related to efficacy, side effects, and patient compliance. For example, traditional oral delivery may result in poor bioavailability, while intravenous administration can lead to systemic toxicity. Furthermore, achieving precise drug targeting remains a challenge, often resulting in off-target effects. The immune system's response to foreign substances can also impact the effectiveness of drug delivery systems. Additionally, issues like stability, scalability, and the potential for developing resistance pose ongoing concerns.
- Limited Bioavailability: Many drugs exhibit poor absorption or degradation in the digestive system, reducing their bioavailability and effectiveness.
- Off-Target Effects: Non-specific distribution of drugs can lead to unintended effects on healthy tissues, causing side effects and limiting therapeutic outcomes.
- Immune Response: The body's immune system can recognize and eliminate drug carriers, reducing the efficacy of delivery systems.
- Stability Issues: Some drugs are inherently unstable, and maintaining their stability during storage and transportation is a significant challenge
- Patient Compliance: Complex dosing regimens or unpleasant administration methods can result in poor patient adherence to prescribed treatments.
- Invasive Procedures: Certain drug delivery methods, such as injections, may be invasive, causing discomfort and decreasing patient acceptance.
- Resistance Development: Prolonged use of certain drugs may lead toxicity the development of resistance in pathogens, rendering the treatment less effective over time.
What is Nano- particle [5]
Nanoparticles, a cornerstone of nanotechnology, are minuscule structures with dimensions typically ranging from 1 to 100 nanometres. These materials exhibit unique properties due to their small size, setting them apart from bulk materials and even fine particles. The realm of nanoparticles encompasses a wide variety of substances, including metals, polymers, lipids, and ceramics, each offering distinctive features that make them invaluable across numerous scientific disciplines.
One fundamental aspect of nanoparticles is their size-to-surface ratio. As particles shrink to the nanoscale, their surface area increases dramatically in comparison to their volume. This phenomenon leads to enhanced reactivity and specific behaviours, rendering nanoparticles highly versatile. For instance, the increased surface area facilitates better interactions with surrounding molecules, making nanoparticles exceptional candidates for various applications, particularly in the field of drug delivery.
In the realm of medicine, nanoparticles have revolutionized drug delivery systems. The unique physical and chemical properties of nanoparticles allow for the encapsulation of therapeutic agents, protecting them from degradation and improving their solubility. Additionally, their size enables efficient transport across biological barriers, such as the blood-brain barrier, enabling targeted delivery to specific tissues or cells. This precision in drug delivery minimizes side effects and enhances therapeutic efficacy, marking a paradigm shift in pharmaceutical research and development.
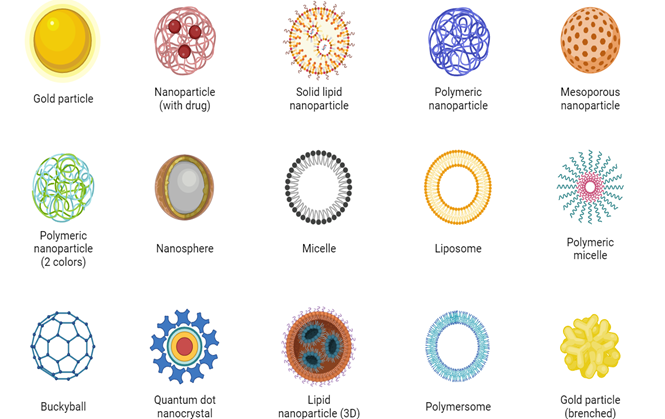
Nanoparticles come in various types, each with distinct properties and applications. Here are some common types of nanoparticles
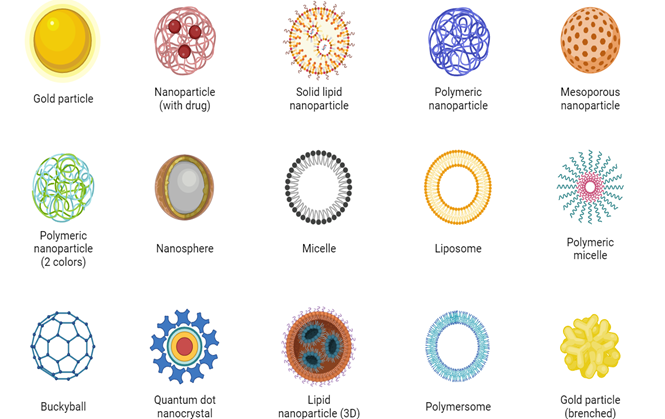
Fig no 1
1. Metal Nanoparticles:
- Gold Nanoparticles: Known for their unique optical properties, gold nanoparticles find applications in imaging, diagnostics, and photo thermal therapy for cancer treatment.
- Silver Nanoparticles: Exhibit antimicrobial properties and are used in various consumer products, wound dressings, and water purification.
2. Polymeric Nanoparticles:
- Liposomes: Spherical vesicles composed of lipid bilayers, liposomes are widely used in drug delivery due to their ability to encapsulate both hydrophobic and hydrophilic substances.
- Polymeric Micelles: Formed by amphiphilic block copolymers, these nanoparticles improve drug solubility and stability, aiding in targeted drug delivery.
3. Ceramic Nanoparticles:
- Silica Nanoparticles: Have a wide range of applications, including drug delivery, imaging, and catalysis, due to their porous structure and biocompatibility.
- Titania Nanoparticles: Known for their photo catalytic properties, used in environmental applications and for self-cleaning surfaces.
4. Magnetic Nanoparticles:
- Iron Oxide Nanoparticles: Exhibit magnetic properties and are employed in biomedical applications such as magnetic resonance imaging (MRI) and targeted drug delivery.
5. Carbon-Based Nanoparticles:
- Carbon Nanotubes: Cylindrical structures with unique mechanical and electrical properties, used in various fields, including electronics, materials science, and drug delivery.
- Fullerenes: Spherical carbon molecules with applications in drug delivery, diagnostics, and materials science.
6. Semiconductor Nanoparticles:
- Quantum Dots: Semiconductor nanoparticles with quantum confinement effects, used in imaging, displays, and photovoltaics due to their tunable optical properties.
7. Metal Oxide Nanoparticles:
- Zinc Oxide Nanoparticles: Employed in sunscreens, electronics, and antimicrobial applications due to their UV-blocking properties and biocompatibility.
- Titanium Dioxide Nanoparticles: Used in sunscreens and photo catalysis, known for their ability to absorb UV radiation.
8. Biodegradable Nanoparticles:
- Chitosan Nanoparticles: Derived from chitin, chitosan nanoparticles find applications in drug delivery and wound healing due to their biocompatibility and biodegradability.
9. Hybrid Nanoparticles:
- Silica-Coated Nanoparticles: Combine the properties of metal or semiconductor nanoparticles with the stability and biocompatibility of a silica shell, used in various applications, including imaging and drug delivery.
Nanotechnology in drug delivery systems [14,15,16,17]
- Nanotechnology has emerged as a new and promising method of drug delivery that is revolutionizing medicine. This technology involves the use of materials at the nanometre scale, typically less than 100 nanometres in size. The application of nanotechnology in drug delivery provides many advantages and solves many problems associated with traditional drug delivery.
- One of the key benefits of nanotechnology in drug delivery is the ability to increase the bioavailability of drugs. Many compounds have poor solubility or stability, preventing them from being absorbed in the body. Nanoparticles have a high surface-to-volume ratio, providing a good way to encapsulate and protect drugs, increasing their solubility and stability. This increases the bioavailability of the drug, resulting in a better therapeutic response.
- In addition, nanotechnology enables targeted delivery of drugs; these is a significant improvement over the nonspecific distribution found in traditional methods. By functionalizing nanoparticles with ligands that recognize cells or tissues, drug carriers can be directed to the desired site of action. This approach can reduce off-target results, reduce side effects, and increase the effectiveness of the drug. For example, in cancer treatment, nanoparticles can be designed to selectively target cancer cells, thereby increasing the effectiveness of chemotherapy while protecting healthy cells.
- The immune system’s response to foreign substances causes problems in drug delivery. Nanotechnology offers solutions that allow the creation of drug carriers that can bypass or alter the immune system. Surface modification of nanoparticles prevents their recognition and elimination by the immune system, thus prolonging circulation and improving drug delivery to the target.
- Safety problems with some drugs can also be solved with nanotechnology. Nanoparticles act as protective carriers, preventing chemical degradation and maintaining their stability during storage and transportation. This is particularly important for biopharmaceuticals and gene therapy, where maintaining good molecular integrity is essential for treatment.
- Patient compliance is important in the success of drug treatment. Nanotechnology offers solutions to increase patient compliance by offering alternative and more patient-friendly medication management methods. For example, nanoscale formulations could lead to improved oral drug delivery that increases drug absorption and reduces dosing frequency.
- This increases patient comfort and can lead to better outcomes. Invasive procedures associated with some drug delivery methods, such as injection, can be reduced with nanotechnology. Nanoparticles can be designed to effectively overcome biological barriers and enable barrier-free drug delivery. This would be particularly useful for diseases affecting the central nervous system where it is very difficult to cross the blood-brain barrier. Nanoparticles can be designed to carry therapeutic agents across this barrier, opening new avenues for the treatment of neurological diseases.
- Nanotechnology also solves the problem of drug resistance through long-term drug use. The precise targeting ability of nanoparticles reduces all healthy tissues to the drug, thus reducing the high selectivity that led to the development of the drug.
- This is important in the context of antibiotics, where inappropriate use of antibiotics increases the risk of antibiotic resistance. In summary, nanotechnology in drug delivery represents a transformative method that can solve many problems associated with traditional approaches.
- From improving drug bioavailability to enhancing target delivery to improving safety and patient compliance, the use of nanotechnology is diverse and promising. As research in this field continues, nanotechnology should play an important role in the future development of medicine, providing better solutions and personal healing.
Need of nanotechnology in drug delivery [2, 5, 6]
In the contemporary landscape of healthcare, the need for nanotechnology and novel drug delivery systems has become increasingly pronounced, driven by a confluence of factors shaping the demands and challenges of modern medicine.
- Precision Medicine and Personalization:
Nanotechnology allows for the creation of targeted drug delivery systems, enabling precision in medicine. Tailoring treatments to individual patient profiles enhances efficacy while minimizing side effects. This personalized approach is particularly crucial in addressing the genetic and molecular diversity observed in patient populations.
- Overcoming Biopharmaceutical Challenges:
Many conventional drugs face challenges related to poor solubility, limited bioavailability, and non-specific distribution. Nano-carriers, such as nanoparticles and liposomes, offer solutions by improving drug stability, enhancing solubility, and facilitating controlled release. This is vital in maximizing therapeutic impact and minimizing adverse effects.
- Enhanced Therapeutic Efficacy:
Novel drug delivery systems allow for the controlled and sustained release of therapeutic agents. This not only prolongs the duration of drug action but also improves patient compliance. For chronic conditions, sustained drug release can lead to better disease management and overall improved outcomes.
- Crossing Biological Barriers:
Nanotechnology enables the design of drug delivery systems that can overcome biological barriers, such as the blood-brain barrier. This is particularly relevant in neurological disorders where delivering therapeutic agents to specific brain regions is a significant challenge.
- Minimizing Side Effects:
Targeted drug delivery helps minimize systemic exposure of drugs to healthy tissues, reducing side effects. This is crucial in enhancing the safety profile of medications and improving the quality of life for patients undergoing treatments for various medical conditions.
- Facilitating Combination Therapies:
Nanotechnology provides a platform for the development of combination therapies, where multiple drugs or therapeutic agents can be encapsulated within a single Nano carrier. This approach allows for synergistic effects, addressing complex diseases more comprehensively.
- Advances in Imaging and Diagnostics:
The integration of nanotechnology in imaging modalities enables not only improved diagnostics but also real-time monitoring of therapeutic responses. This contributes to the development of theranostic approaches, where diagnosis and therapy are integrated into a single platform.
- Responding to Global Health Challenges:
In the face of emerging infectious diseases and global health threats, rapid and targeted drug delivery becomes crucial. Nanotechnology offers the potential for developing effective antiviral and antibacterial agents with enhanced specificity and efficiency.
Action mechanism of nanoparticles in drug delivery system [2]
When outlined to dodge the body's defines components nanoparticles have advantageous properties that can be utilized to progress medicate conveyance. Different nanoparticle definitions have been spread in sedate improvement in an endeavour to extend adequacy, security and tolerability of joined drugs. Nanoparticle based definitions have appeared tall solvency, control discharge, progressed pharmacokinetic and pharmacodynamics properties. Molecule measure, surface charge and shape play critical parts in making successful nanoparticle conveyance frameworks that work through assortment of mechanisms
Molecule measure and measure dissemination are the foremost vital characteristics since these decide the chemical and physical properties of nanomaterials. The hydrodynamic estimate and measure conveyance decide the in vivo dispersion, natural destiny, harmfulness, and focusing on capacity of these nanomaterial’s for medicate conveyance framework. They can control sedate stacking, its discharge and soundness. It has been detailed that nanomaterial’s are beneficial over smaller scale scale particles and due to little estimate and high mobility that make them able of higher cellular take-up appropriate for more extensive extend of cellular and intracellular targets .
Surface charge is more often than not communicated and measured in terms of the nanomaterial’s zeta potential which reflects the electrical potential of particles that's impacted by its composition and the medium in which it is scattered. Zeta potential having an esteem of ± 30 mV have been detailed to be steady in suspension leads to avoiding conglomeration of particles. Surface charge of nanomaterials is significant to medicate stacking. Drugs can be stacked through a number of forms such as covalent conjugation, hydrophobic interaction, charge-charge interaction or embodiment. Stacking of particles depends upon nature of the sedate as well as nature of target atom, too changes the surface charge. By changing zeta potential connection or adsorption of charged atom can be decided on the surface of nanoparticle.
Joining of a medicate on or in nanomaterial’s is alluded to as medicate stacking. A perfect nanoparticles sedate conveyance frame workought to have a tall drug-loading capacity without conglomeration. Tall sedate stacking capacity can minimize organization or the number of doses. Dispensability is required for smooth and effective conveyance of the drugs. Sedate stacking can be finished in a few ways; in any case, sedate stacking and capture productivity depend on sedate solvency within the nanoparticles, scattering medium, nanomaterial’s measure and composition, medicate atomic weight (MW) and solvency, drug-nanomaterial’s interaction, and/or the nearness of surface useful bunches (i.e. carboxyl, amine, ester, etc.) on either the drugs or on the nanomaterial’s.
On Focusing on of tumour leads to progressing chemotherapy by nanomaterial’s give an exceedingly particular and flexible stage for cancer treatment. Upgraded penetrability and maintenance empowers particular localization in tumour suddenly due to fenestrated blood vessels as in case of sedate stacked liposome (doxorubicin-liposome complex). It has been appeared to viably move forward specific localization in human tumours in vivo of small-molecule drugs such as doxorubicin as illustrated by Nano size liposomes target tumours suddenly since of the fenestrated blood vessels. Usually due to upgraded porousness and consequent sedate retention. Focusing on of nanomaterial’s as sedate conveyance vehicles or Nano carriers for site-specific conveyance contains a number of preferences over focusing on ligand-drug conjugates. Productive medicate stacking of tall concentrations of sedate inside the Nano carriers can be conveyed particularly to the target cell or tissue when a ligand interatomic with its receptor which comes about within the conveyance of huge payloads of restorative operator relative to number of ligand-binding destinations. This is often beneficial in imaging tumour through the increment in tumour flag to foundation ratio. The Nano carriers are joined to the ligand and the medicate is stacked autonomous of the coupling of ligands. This moreover bypasses sedate action which will be due to arrangement of ligand-drug complex conjugate or inactivated by possibly forceful coupling response. An expansive number of ligand atoms can be connected to the Nano carriers depending upon the measure of the nanomaterial’s and the estimate of the medicate to extend the likelihood of authoritative to target cells particularly for those with moo official affinities. Dynamic focusing on empowers effective dissemination of the carriers within the tumour, in this manner lessening the return of sedate back to the circulation that may be caused by tall intratumoral weight and, when ligand is as it were connected to the carrier due to the little measure of the conjugate, it can as it were extravagate at the infection location but not in typical vasculature, and as such, the ligand cannot connected with the target epitopes of ordinary tissues maintaining a strategic distance from side effects.
- Binding to the receptor site
Official to the receptor destinations Routine sedate carriers lead to adjustment of the medicate dispersion profile because it is conveyed to the MPS (Mono Phagocytic Framework) such as liver, spleen, lungs, and bone marrow. In any case, nanoparticles as sedate carriers can be recognized by the have resistant framework when intravenous managed causing them to be cleared by phagocytes from the circulation. The measure of the nanoparticles, surface hydrophobicity, and surface coating functionalities decide the level of blood components (e.g. opsonins) that tie to its surface affecting the in vivo destiny of nanoparticles. To upgrade the chances of victory in sedate focusing on, it is imperative to avoid the opsonization whereas drawing out the circulation of nanoparticles in vivo. The nanoparticles can accomplish this by pre-coating with hydrophilic polymers and/or surfactants or by utilizing nanoparticles with biodegradable hydrophilic copolymers such as PEG (Polyethylene Glycol). Nanoparticles experience extravasation amid section into tumor tissues which happens by implies of the improved porousness and maintenance (EPR) impact. In this way, drugs carried by nanoparticles for conveyance or Nano- empowered drugs at the lower measure extend are ideal to the upper submicron and micron sizes to realize longer circulation half-lives through the decreased macrophage mononuclear take-up and more productive cellular uptake. It has been detailed that the vascular pore measure of lion's share of strong tumors ranges between 380nm-780nm. Depending upon sort of tumor, development rate, and microenvironment, organization of vasculature may contrast. Thus, to reach at tumor destinations estimate of the Nano carriers must be littler than cutoff pore breadth.
The process of diffusing or dissolution drug in the body, which is loaded into nanoparticle, is known as drug release while biodegradation refers to collapsing the drug delivery system inside the body. Both drug release and biodegradation are important to consider when developing a nanoparticle drug delivery system. Besides active components, solubility, diffusion and particle size also determines the effectiveness of the drug. High surface to volume ratio is leads to faster drug release at the surface due to small size of particles. In contrast, larger particles have large cores, which allow more drugs to be encapsulated per particle and give slower release. Thus, manipulation of particle size provides a trigger to tuning drug release rates. The interaction of nanomaterial’s with cells provides an advantage to cross through the blood brain barrier. The blood brain barrier consists of a tightly packed layer of endothelial cells surrounding the brain that prevents high-molecular weight molecules from passing through it. The ability of nanoparticles to pass through the blood brain barrier is an important advantage for drug delivery systems for effective treatments. However, the efficacy of nanoparticles toward the treatment of neurological disorders, like brain tumor, stroke, and Alzheimer’s disease, have been largely constrained in spite of the advances and breakthroughs in nanotechnology-based medical approaches. Targeting of drugs to the central nervous system remains for the future success and development of nanotechnology-based diagnostics and therapeutics in neurology.
Synthesis of nanoparticles [39]
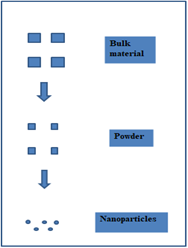
- Top to down approach
The first macroscopic structures are used in the top-down methodology. The techniques start with bigger particles, which are then processed through a series of steps to become nanoparticles. These methods' primary drawbacks are their extensive installation requirements and high setup costs. Large-scale production is not suitable for the methods due to their high cost. The procedure is appropriate for use in lab settings. The method is predicated on material grinding. Soft samples are unsuitable for these techniques.
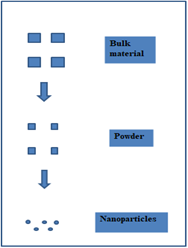
Fig No 2 Top To Down Approach
Methods in top-down approach:
- Physical vapor deposition.
- Chemical vapor deposition
- Ion implantation
- Electron beam lithography
- X-ray lithography
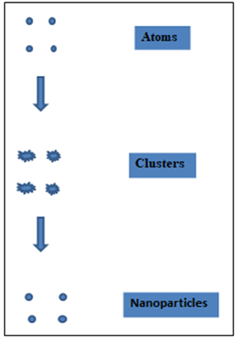
- Bottom up approach
The process of producing nanomaterial’s through bottom-up methods involves reducing the size of material components to the atomic level and then developing nanostructures through an extra step. The physical forces operating at the Nano scale integrated basic units into more substantial, stable structures as the process continued. The self-assembly concept of molecular recognition serves as the foundation for the methodology. Growing more and more of one's type from oneself is known as self-assembly. For the purpose of producing nanoparticles for sale, several of these methods are either in the early stages of development or are only now being applied.
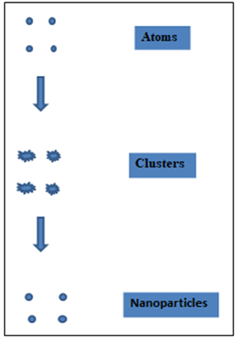
Fig no 3 Bottom up approach
Methods in a bottom-up approach:
- Sol-gel synthesis
- Colloidal precipitation
- Hydrothermal synthesis
- Organometallic chemical route
- Electrode position
Applications of nanoparticles
Using a Nano particulate delivery method to target tumours. [17, 1
- Nanoparticles will be able to deliver a concentrated dose of medicine in the region of the tumour targets via the improved permeability and retention impact or active nanoparticles. This is the rationale for using nanoparticles for tumour targeting.
- By limiting medication distribution to the target organ, nanoparticles will lower the amount of drugs exposed to healthy tissues. A study showed that mice treated with doxorubicin embedded in poly (isohexylcynoacrylate) Nano spheres showed increased doxorubicin concentrations in their liver, spleen, and lungs compared to mice treated with free doxorubicin
Nanoparticles for Verbal Conveyance of Peptides and Proteins [32, 33]
Critical propels in biotechnology and organic chemistry have driven to the revelation of various bioactive atoms and immunizations based on peptides and proteins. The improvement of reasonable carriers remains a challenge, as the bioavailability of these atoms is restricted by the epithelial boundary of the gastrointestinal tract and their helplessness to gastrointestinal corruption by stomach related proteins. Polymer nanoparticles empower the epitome of bioactive particles and ensure them from enzymatic and hydrolytic debasement. For illustration, nanoparticles typifying affront were found to preserve affront movement and lower blood glucose levels in diabetic rats for up to 14 days after verbal organization. The surface zone of the human mucous layer is 200 times that of the skin62. The gastrointestinal tract gives different physiological and morphological obstructions to the conveyance of proteins and peptides.
-
- Proteolytic proteins within the intestinal lumen, such as pepsin, trypsin, and chymotrypsin.
- Proteolytic proteins (endopeptidases) within the brush border film.
- Intestinal microbiota.
- Mucosal layer and internal layer of epithelial cells. The histological structure of the mucous film is expecting to viably anticipate the assimilation of particles from the environment. A vital methodology to overcome the gastrointestinal boundary is to convey drugs in colloidal carrier frameworks such as nanoparticles. This progresses the interaction instrument between the sedate conveyance framework and the epithelial cells of the gastrointestinal tract.
Nanoparticles for Gene delivery [27, 29]
Polynucleotide immunizations work by conveying qualities encoding important antigens to have cells where they are communicated, creating the antigenic protein inside the region of proficient antigen showing cells to start resistant reaction. Such immunizations deliver both humoral and cell mediated resistance since intracellular generation of protein, as restricted to extracellular testimony, invigorates both arms of the safe framework.
Anti-Microbial Techniques [37, 38]
One of the most punctual Nano medicine applications was the utilize of Nano crystalline silver, which is as an antimicrobial operator for the treatment of wounds, A nanoparticle cream has been appeared to battle staph diseases. The nanoparticles contain nitric oxide gas, which is known to slaughter microbes. Thinks about on mice have appeared that utilizing the nanoparticle cream to discharge nitric oxide gas at the location of staph abscesses essentially diminished the contamination. Burn dressing that's coated with Nano capsules containing antibiotics. In case a disease begins the [31] Harmful microscopic organisms within the wound causes the Nano capsules to break open, discharging the antibiotics. This permits much speedier treatment of a contamination and decreases the number of times a dressing must be changed. A welcome thought within the early think about stages is the end of bacterial contaminations in an understanding inside minutes, instead of conveying treatment with anti-microbial over a period of weeks. CONCLUSION
The integration of nanoparticles into drug delivery systems represents a ground-breaking frontier in pharmaceutical research. This comprehensive review has highlighted the multifaceted benefits and applications of nanoparticle-based delivery, showcasing their ability to enhance drug solubility, bioavailability, and targeted release. The versatility of nanoparticles, from liposomes to polymeric carriers, opens avenues for tailored therapeutic strategies, paving the way for personalized medicine. Despite the remarkable progress, challenges like potential toxicity and long-term effects necessitate further exploration. Future endeavours should focus on refining nanoparticle designs, optimizing manufacturing processes, and ensuring rigorous safety assessments. As we delve deeper into this promising field, the convergence of nanotechnology and drug delivery holds immense potential for revolutionizing treatment paradigms and improving patient outcomes, marking a pivotal era in pharmaceutical innovation.
REFERENCE
- Siddiqui AA, Iram F, Siddiqui S, Sahu K. Role of natural products in drug discovery process. Int J Drug Dev Res. 2014;6(2):172–204.
- P Prabhakar*, Mamoni Banerjee, Nanotechnology in Drug Delivery System: Challenges and Opportunities, J. Pharm. Sci. & Res. Vol. 12(4), 2020, 492-49
- Barber DJ, Freestone IC. An investigation of the origin of the colour of the Lycurgus Cup by analytical transmission electron microscopy. Archaeometry. 1990; 32(1):33–45.
- Buentello, F.S., Persad,D.L., Court,E.B., Martin, D.K., Daar, A.S., and Singer, P.,A. (2005). Nanotechnology and the developing world. PLoS Medicine, 5(2): 383-386.
- Kingsley, J.D., Dou, H., Morehead, J., Rabinow, B., Gendelman, H.E. and Destache, C.J. (2006). Nanotechnology: a focus on nanoparticles as a drug delivery system. J Neuroimmune Pharmacol, 1(3): 340-50. 3. Ochekpe, N.A., Olorunfemi, P.O. and Ngwuluka, N.C. (2009). Nanotechnology and Drug Delivery Part 1: Background and Applications. Tropical Journal of Pharmaceutical Research, 8 (3): 265-274
- Noel, C.K.H., Tin, C.T.C., Emily, F.Y.H. and Queenie, L.T.K. (2015). Nano targeted drug delivery system. The University of Hong Kong, 1-2. 12. Jabbari, A. and Sadeghian, H. (2012). Novel drug delivary systems –Amphiphilic Cyclodextrins, Synthesis, Utilities and Application of Molecular Modeling in Their Design. 331-351. 13. Kaparissides, C., Alexandridou, S., Kotti, K. and Chaitidou, S. (2006). Recent Advances in Novel Drug Delivery Systems. AZoM.com Pty Ltd, pp1-14.
- Sakamotoa, J.H., De Vena, A.L. Godina, B., Blancoa, E. Serdaa, R.E., Grattonia, A., Ziemysa, A., Bouamrania, A., Hua, T., Ranganathana, S.I., Rosaa,E.D., Martineza, J.O., Smida, C.A., Buchanana, D.R.M., Leea, D.S.Y., Srinivasana, D.S., Landrya, M., Meyna, A., Tasciottia, E., Liua, X., Decuzzia, P.E. and Ferraria, M.B.C. (2010). Enabling individualized therapy through nanotechnology. Pharmacol Res, 62(2): 57–89.
- Gelperina, S., Kisich, K., Iseman, M.D. and Heifets, L. (2005). The Potential Advantages of Nanoparticle Drug Delivery Systems in Chemotherapy of Tuberculosis. American Journal of respiratory and critical care medicine, 172: 1487-1490.
- Cagdas, M., Sezer, A.D. and Bucak, S. (2014). Application of nanotechnology in drug delivary- Liposomes as Potential Drug Carrier Systems for Drug Delivery. pp1-32.
- Siepmann F, Herrmann S, Winter G, Siepmann J. A novel mathematical model quantifying drug release from lipid implants. J Control Release. 2008;128:233–40
- S. Soares, J. Sousa, A. Pais, and C. Vitorino, “Nanomedicine: Principles, properties, and regulatory issues,” Front. Chem., vol. 6, no. AUG, pp. 1–15, 2018.
- K. Jain and S. Thareja, “In vitro and in vivo characterization of pharmaceutical nanocarriers used for drug delivery,” Artif. Cells, Nanomedicine Biotechnol., vol. 47, no. 1, pp. 524–539, 2019.
- Kumar and C. K. Dixit, “Methods for characterization of nanoparticles,” Adv. Nanomedicine Deliv. Ther. Nucleic Acids, pp. 44–58, 2017.
- R. S. and J. W. L. Jr., “Nanoparticle-based targeted drug delivery,”vol. 86, no. 3, pp. 215–223, 2009.
- M. B., “Nanosize drug delivery system,” Curr. Pharm. Biotechnol., vol. 14, no. 15, p. 1221, 2013.
- Gonda, N. Zhao, J. V Shah, H. R. Calvelli, N. L. Francis, and V.Ganapathy, “Engineering Tumor-Targeting Nanoparticles as Vehicles for Precision Nanomedicine,” Med One, vol. 2019, no. 4,pp. 1–30, 2019.
- V. C. R. M. O. A. & Khungar, “Design of Nanoparticle-Based Carriers for Targeted Drug Delivery,” J. Nanomater., vol. 2016, no.1, pp. 1–15, 2016.
- Yu et al., “Receptor-targeted nanocarriers for therapeutic delivery to cancer,” vol. 7688, 2010.
- R. L. Adam D. Friedman, Sarah E. Claypool, “The Smart Targeting of Nanoparticles,” Curr Pharm Des, vol. 19, no. 35, pp. 6315–6329, 2013.
- Y. H. B. and K. Park, “Targeted drug delivery to tumors: Myths,reality and possibility,” J Control Release, vol. 153, no. 3, pp. 198–205, 2011.
- J. McMillan, E. Batrakova, and H. E. Gendelman, Cell delivery oftherapeutic nanoparticles, vol. 104, no. Table I. 2011.
- O. Gamucci, A. Bertero, M. Gagliardi, and G. Bardi, “BiomedicalNanoparticles: Overview of Their Surface Immune-Compatibility,” Coatings, vol. 2014, no. 4, pp. 139–159, 2014.
- N. Schmiedebergs and A. Pharmacol, “PEGylation as a strategy forimproving nanoparticle-based drug and gene delivery,” Adv DrugDeliv Rev., vol. 99, pp. 28–51, 2016.
- M. F. Elvin Blanco, Haifa Shen, “Principles of nanoparticledesign for overcoming biological barriers to drug delivery,” Nat Biotechnol., vol. 33, no. 9, pp. 941–951, 2016.
- Zhang, Y. Hu, and Z. Pang, “Modulating the tumormicroenvironment to enhance tumor nanomedicine delivery,”Front. Pharmacol., vol. 8, no. DEC, pp. 1–16, 2017.
- Chenthamara et al., “Therapeutic efficacy of nanoparticles androutes of administration,” Biomater. Res., vol. 23, no. 1, pp. 1–29, 2019.
- M. Teleanu, I. Negut, V. Grumezescu, A. M. Grumezescu, and R. I. Teleanu, “Nanomaterials for drug delivery to the centralnervous system,” Nanomaterials, vol. 9, no. 3, pp. 1–18, 2019
- C. Wang, X. Hu, Y. Gao, and Y. Ji, “ZnO nanoparticles treatmentinduces apoptosis by increasing intracellular ROS levels in LTEP-a-2 cells,” Biomed Res. Int., vol. 2015, 2015.
- E. Barci?ska, J. Wierzbicka, A. Zauszkiewicz-Pawlak, D. Jacewicz,A. Dabrowska, and I. Inkielewicz-Stepniak, “Role of Oxidative andNitro-Oxidative Damage in Silver Nanoparticles Cytotoxic Effectagainst Human Pancreatic Ductal Adenocarcinoma Cells,” Oxid. Med. Cell. Longev., vol. 2018, 2018.
- L. Zhang, L. Wu, Y. Si, and K. Shu, “Size-dependent cytotoxicityof silver nanoparticles to Azotobacter vinelandii: Growth inhibition, cell injury, oxidative stress and internalization,” PLoS One, vol. 13,no. 12, pp. 1–13, 2018.
- E. Åkerlund, M. S. Islam, S. McCarrick, E. Alfaro-Moreno, and H.L. Karlsson, “Inflammation and (secondary) genotoxicity of Ni andNiO nanoparticles,” Nanotoxicology, vol. 13, no. 8, pp. 1060–1072, 2019.
- R. G. and H. Xie, “Nanoparticles in Daily Life: Applications, Toxicity and Regulations,” J Env. Pathol Toxicol Oncol, vol. 37,no. 3, pp. 209–230, 2018.
- De Campos AM, Sánchez A, Alonso MJ. Chitosan nanoparticles: a new vehicle for the improvement of the delivery of drugs to the ocular surface. Application to cyclosporin A. Int J Pharm. 2001;224:159–68.
- .Haque S, Md S, Sahni JK, Ali J, Baboota S. Development and evaluation of brain targeted intranasal alginate nanoparticles for treatment of depression. J Psychiatr Res. 2014;48:1–12.
- .Román JV, Galán MA, del Valle EMM. Preparation and preliminary evaluation of alginate crosslinked microcapsules as potential drug delivery system (DDS) for human lung cancer therapy. Biomed Phys Eng Expr. 2016;2:035015.
- Garrait G, Beyssac E, Subirade M. Development of a novel drug delivery system: chitosan nanoparticles entrapped in alginate microparticles. J Microencapsul. 2014;31:363–72.
- Goswami S, Naik S. Natural gums and its pharmaceutical application. J Sci Innovative Res. 2014;3:112–21.
- Zhang L, Gu F, Chan J, Wang A, Langer R, Farokhzad O. Nanoparticles in medicine: therapeutic applications and developments. Clin Pharmacol Ther. 2008;83:761–9.
- Nilesh patil1*, rajveer bhaskar, vishal vyavhare, rahul dhadge, vaishnavi khaire, yogesh patil, overview on methods of synthesis of nanoparticles, review article, int j curr pharm res, vol 13, issue 2, 11-16


 Vinit Khairnar*
Vinit Khairnar*
 Sudarshan kale
Sudarshan kale
 shraddha vaishnav
shraddha vaishnav
 chaitali markand
chaitali markand
 10.5281/zenodo.10933213
10.5281/zenodo.10933213