Abstract
The study investigates the incidence of Type 2 Respiratory Failure (T2RF) in hypothyroidism among 200 patients, exploring various parameters including age, gender, symptoms, exposure history, and comorbidities. T2RF, characterised by inadequate oxygenation of blood and retention of carbon dioxide, is a critical respiratory condition often associated with underlying medical disorders. Hypothyroidism, a common endocrine disorder resulting from decreased thyroid hormone production, can predispose individuals to respiratory complications, including T2RF, due to metabolic and respiratory muscle dysfunction. Results reveal a 41% incidence of T2RF among participants, indicating a significant burden of respiratory compromise in hypothyroid patients. Symptom analysis indicates prevalent manifestations such as cough with sputum, shortness of breath, and hot flashes, reflecting the clinical complexity of hypothyroidism. Age-wise distribution underscores an increasing trend of T2RF with advancing age, emphasising the need for tailored interventions for older populations prone to respiratory complications. Gender analysis suggests a higher incidence of T2RF among females compared to males within the sampled population, highlighting potential gender-specific risk factors or physiological differences contributing to respiratory dysfunction. Environmental and medical exposures, such as radiation and medication, are identified as potential risk factors, necessitating further exploration of their impact on respiratory health in hypothyroid patients. Comorbidity analysis reveals overlapping health conditions among patients with T2RF, including diabetes mellitus, hypertension, chronic obstructive pulmonary disease, coronary artery disease, and chronic kidney disease. Additionally, smaller cohorts exhibit pneumonia, obstructive sleep apnea, bronchial asthma, and unspecified comorbidities, with varying associations to T2RF. These findings underscore the complex interplay of age, gender, environmental exposures, and comorbidities in the development of T2RF in hypothyroidism, highlighting the importance of comprehensive patient assessment and targeted interventions in clinical management.
Keywords
Type 2 Respiratory Failure, Hypothyroidism.
Introduction
Respiratory failure and hypothyroidism stand as distinctive entities within the vast landscape of medical conditions,
each posing unique challenges to the intricate balance of the human body.
Type 2 Respiratory Failure, a condition marked by inadequate gas exchange in the lungs, and Hypothyroidism, characterised by diminished thyroid hormone production, are critical areas of study in the realm of healthcare.
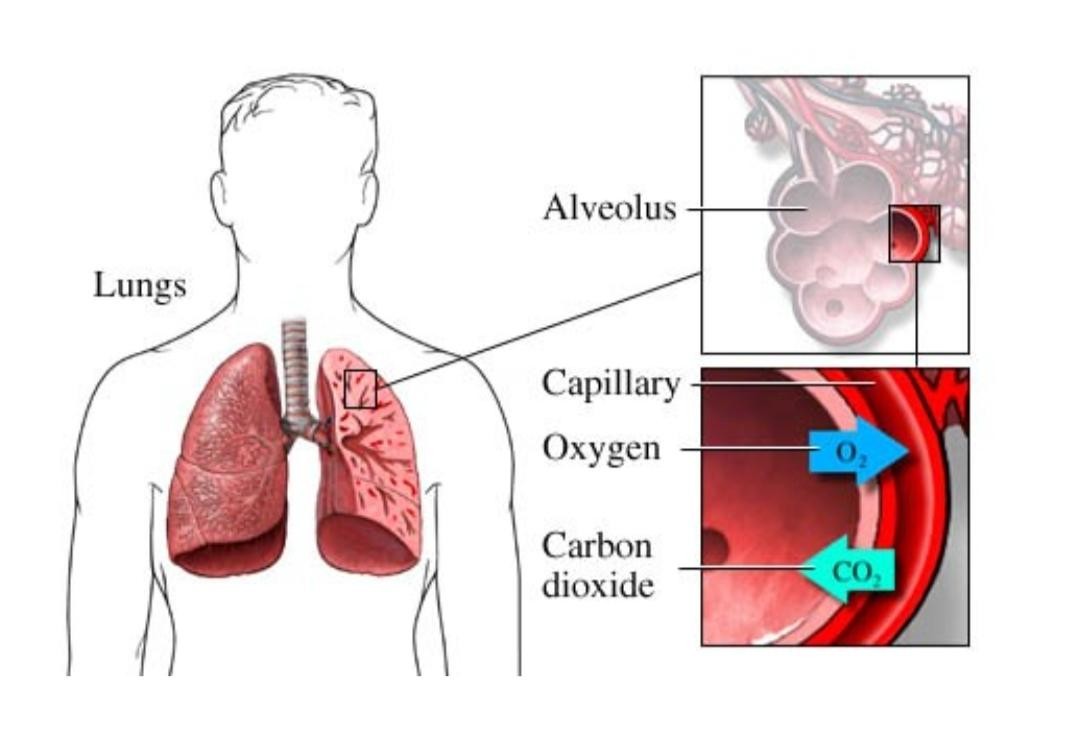
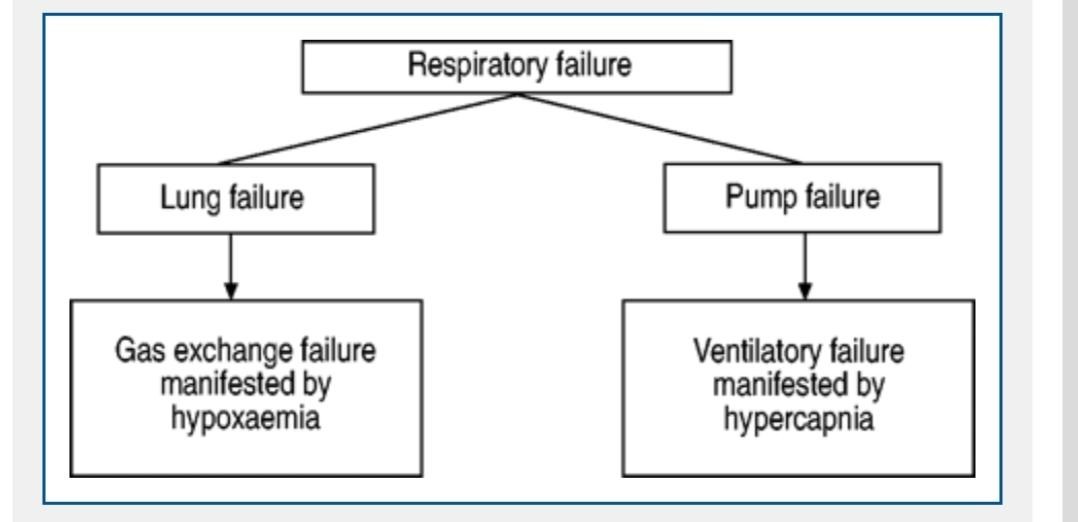
Image 01; Type 2 Respiratory Failure
1.1 Type 2 Respiratory Failure:
Type 2 Respiratory Failure, also known as hypercapnic or ventilatory failure, involves an inability to effectively eliminate carbon dioxide (CO2) from the bloodstream through the respiratory system. This failure stems from compromised lung function, often associated with chronic respiratory diseases such as chronic obstructive pulmonary disease (COPD), neuromuscular disorders, or severe chest wall abnormalities.
At its core, respiratory failure involves the inability of the respiratory system to fulfil its primary function: the exchange of oxygen and carbon dioxide between the air and blood. In Type 2 Respiratory Failure, the focus is on the inadequate removal of CO2, primarily driven by ventilatory inefficiency. Unlike Type 1 Respiratory Failure, which is marked by low oxygen levels in the blood, Type 2 Respiratory Failure is distinguished by elevated CO2 levels.
1.1.1 Aetiology of Type2 Respiratory Failure
Type 2 Respiratory Failure is primarily caused by conditions that undermine the efficiency of the respiratory system, leading to an inability to adequately eliminate carbon dioxide (CO2) from the bloodstream. The key contributors to this respiratory insufficiency encompass a range of chronic respiratory diseases and factors affecting respiratory muscle function.
|
Chronic Respiratory Diseases
|
Other Causes
|
- Chronic Obstructive Pulmonary Disease
- Neuromuscular disorders like myasthenia gravis, amyotrophic lateral sclerosis
|
- Chest wall abnormalities like severe kyphoscoliosis
- Respiratory muscle weakness like muscle dystrophy
- Altered respiratory drive
- Ventilatory insufficiency
|
Table 01; Aetiology of Type 2 Respiratory Failure
1.1.1.1 Chronic Respiratory Diseases
1.1.1.1.1. Chronic Obstructive Pulmonary Disease (COPD)
A predominant factor, COPD, which includes chronic bronchitis and emphysema, is a leading cause of Type 2 Respiratory Failure. The progressive nature of COPD results in airway obstruction, inflammation, and damage to lung tissues, impairing the exchange of gases in the alveoli.
1.1.1.1.2. Neuromuscular Disorders:
Conditions affecting the nerves and muscles involved in respiration, such as amyotrophic lateral sclerosis (ALS), myasthenia gravis, or Guillain-Barré syndrome, can lead to weakened respiratory muscles and reduced ventilatory capacity.
1.1.1.2 Chest Wall Abnormalities:
Severe Kyphoscoliosis: Deformities in the chest wall, particularly severe kyphoscoliosis, can restrict lung expansion and negatively impact respiratory mechanics, contributing to Type 2 Respiratory Failure.
1.1.1.3 Respiratory Muscle Weakness:
Muscle Weakness: Conditions that weaken the respiratory muscles, such as muscular dystrophy or certain metabolic myopathies, compromise the ability to generate adequate respiratory effort, resulting in inefficient ventilation.
1.1.1.4 Altered Respiratory Drive:
Central Respiratory Drive Dysfunction: Disorders affecting the central respiratory centres in the brain, such as certain neurological conditions or drug-induced respiratory depression, can disrupt the signals that regulate breathing, leading to inadequate ventilation.
1.1.1.5 Combined Effects:
In many cases, the causes of Type 2 Respiratory Failure are multifactorial, with a combination of chronic respiratory diseases, neuromuscular factors, and chest wall abnormalities contributing to the overall ventilatory inefficiency.
The intricate interplay of these elements underscores the complexity of Type 2 Respiratory Failure and necessitates a comprehensive approach to its diagnosis and management.
1.1.1.6 Ventilatory Inefficiency:
The hallmark of Type 2 Respiratory Failure lies in the inability of the respiratory system to effectively remove CO2 during exhalation. This inefficiency stems from a combination of factors, including impaired gas exchange in the lungs, diminished respiratory muscle strength, and altered respiratory drive.
As a result, the levels of carbon dioxide in the bloodstream rise, leading to respiratory acidosis: a condition where the blood becomes more acidic.
Understanding the diverse array of factors that can precipitate Type 2 Respiratory Failure is essential for clinicians, as it guides targeted interventions and therapeutic strategies. Addressing the underlying causes while managing the associated symptoms is pivotal in optimising patient outcomes and improving the overall respiratory function in individuals affected by this condition.
1.1.2 Epidemiology of Type 2 Respiratory Failure
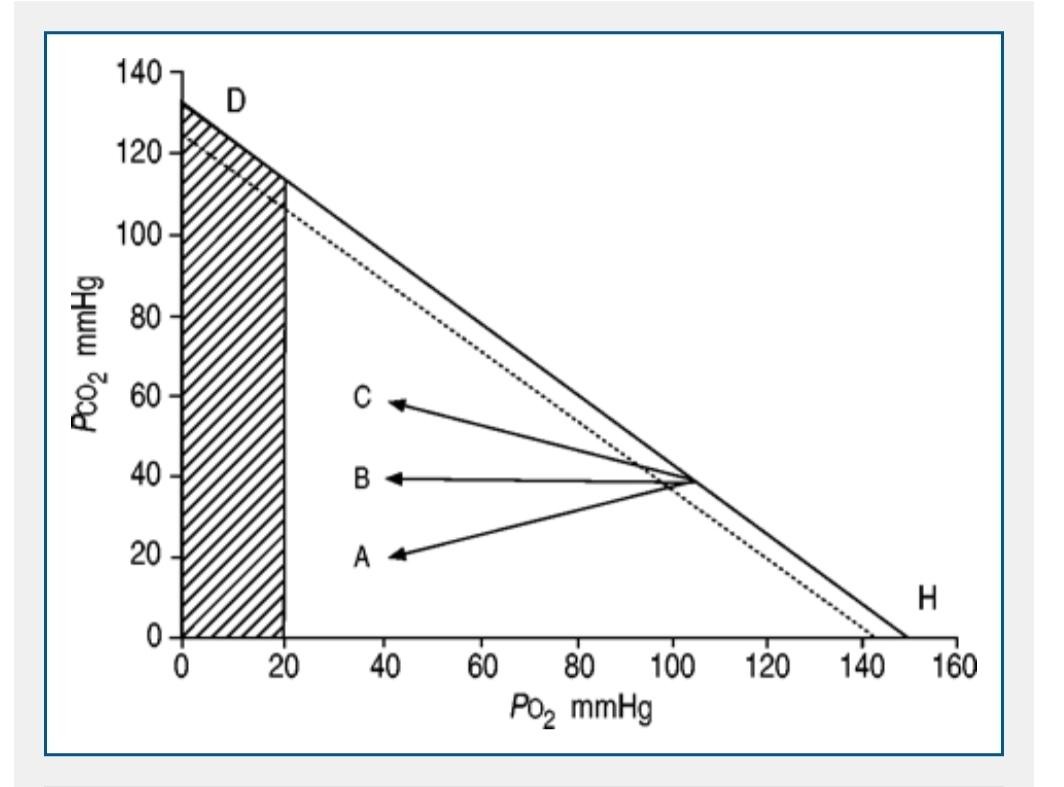
The prevalence of Type 2 respiratory failure increases with age, and smoking is a major risk factor. Geographically, areas with high levels of air pollution may experience a higher incidence.
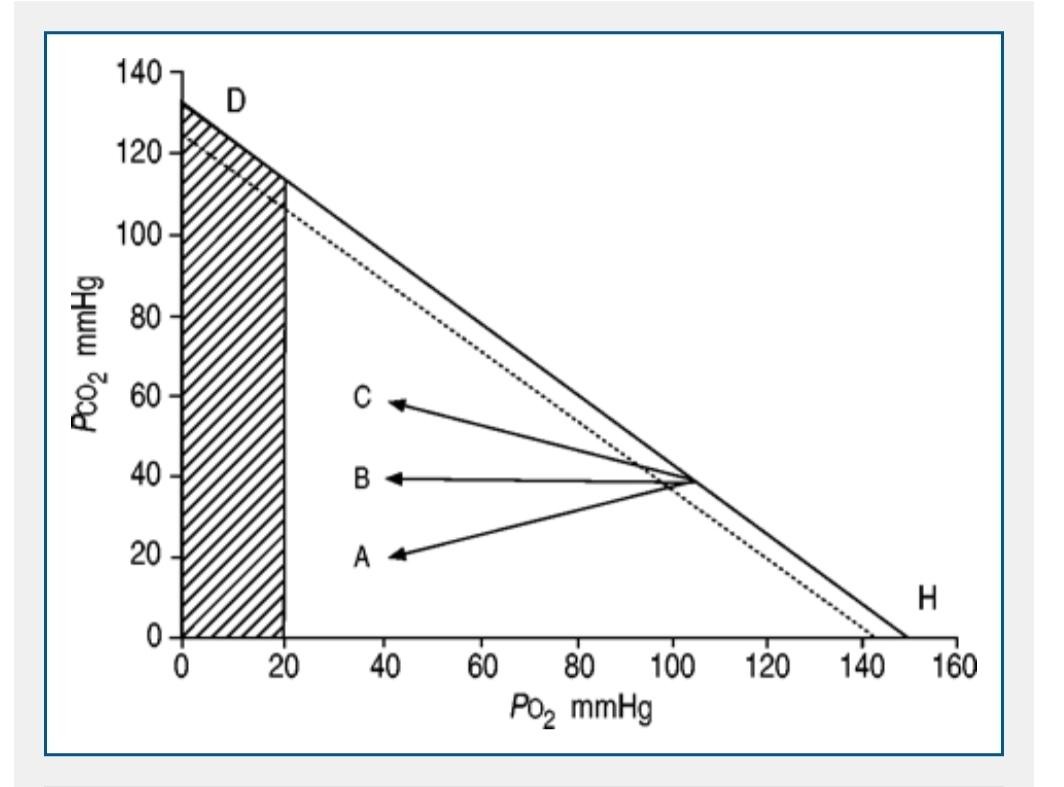
Image 02; Epidemiology of Type 2 Respiratory Failure
Additionally, comorbidities such as obesity and cardiovascular diseases contribute to the burden of Type 2 respiratory failure. Understanding its epidemiology is crucial for public health planning, early detection, and management strategies to improve outcomes for affected individuals.
- The incidence is approximately 137.1 per 100,000 individuals in the US.
- Mortality rate is approximately 29%-42%
- India contributes to 15.69% of global chronic respiratory diseases.
1.1.3 Pathophysiology of Type 2 Respiratory Failure:
Type 2 Respiratory Failure is a complex medical condition characterised by the inability to effectively eliminate carbon dioxide (CO2) from the bloodstream, leading to elevated levels of this gas in the blood, known as hypercapnia.
To comprehend the pathophysiology of Type 2 Respiratory Failure, it is essential to dissect the intricate mechanisms that govern respiratory function and understand how disruptions in these processes contribute to ventilatory insufficiency.
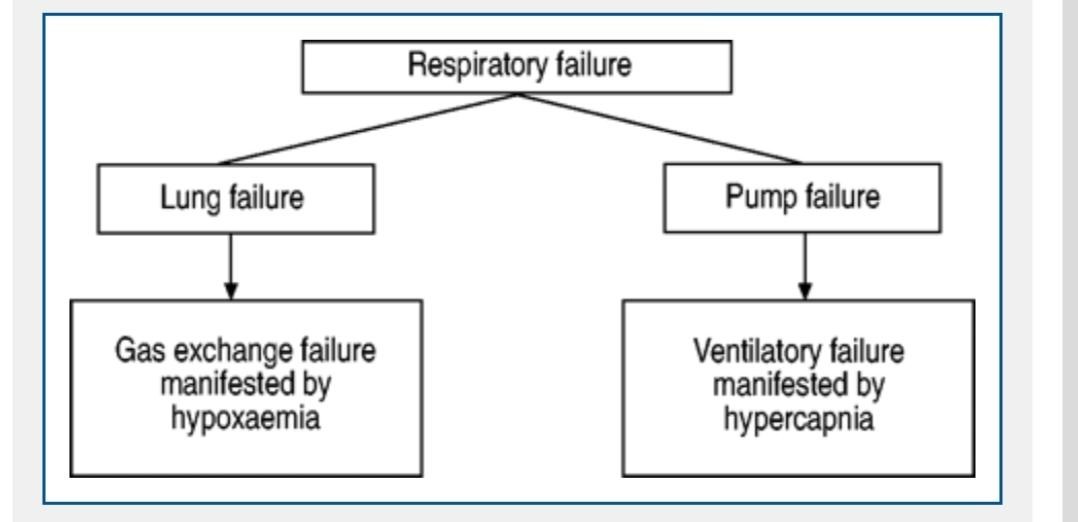
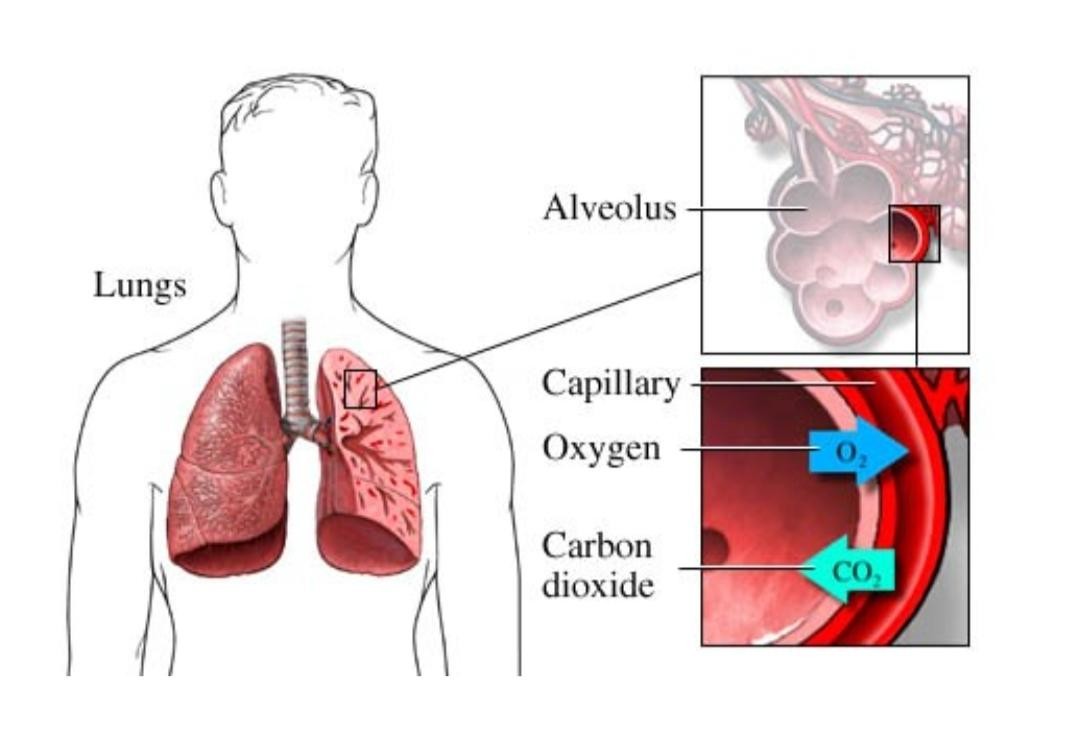
Image 03; Pathophysiology of Type 2 Respiratory Failure
1.1.3.1 Gas Exchange in the Alveoli:
The journey begins within the alveoli, the tiny air sacs in the lungs where the exchange of oxygen and carbon dioxide takes place. In a healthy respiratory system, inspired air, rich in oxygen, travels through the airways to reach the alveoli.
Simultaneously, deoxygenated blood from the body flows through the pulmonary capillaries surrounding the alveoli. This sets the stage for the diffusion of oxygen into the bloodstream and the release of carbon dioxide from the blood into the alveoli.
1.1.3.2 Ventilation-Perfusion Mismatch:
In Type 2 Respiratory Failure, disruptions in this delicate dance of gas exchange occur. One prominent factor is a ventilation-perfusion mismatch, where certain areas of the lungs receive inadequate ventilation despite sufficient blood flow.
This mismatch can arise from conditions like chronic obstructive pulmonary disease (COPD), where airway obstruction and tissue damage compromise airflow to specific lung regions.
1.1.3.3 Impaired Gas Exchange:
As a consequence of impaired ventilation-perfusion matching, alveolar-capillary gas exchange becomes inefficient. The alveoli fail to adequately clear carbon dioxide, leading to its accumulation in the bloodstream. This scenario is exacerbated by the fact that individuals with Type 2 Respiratory Failure often have compromised lung function, reducing the overall surface area available for gas exchange.
1.1.3.4 Respiratory Muscle Weakness:
Another crucial facet of Type 2 Respiratory Failure involves the muscles responsible for respiration. The diaphragm and intercostal muscles play a pivotal role in expanding and contracting the thoracic cavity, facilitating breathing. In conditions like neuromuscular disorders or severe chest wall abnormalities, respiratory muscle weakness ensues.
This weakness translates to a diminished ability to generate the necessary negative pressure for inhalation and positive pressure for exhalation, further contributing to inefficient ventilation.
1.1.3.4 Altered Respiratory Drive:
The central respiratory centres in the brain govern the rhythm and depth of breathing. Disruptions in this regulatory system can stem from neurological conditions or medications that suppress respiratory drive.
For example, certain central nervous system depressants may impede the signals that initiate and sustain the respiratory process, resulting in hypoventilation and subsequent hypercapnia.
1.1.3.5 Compensatory Mechanisms:
The body employs compensatory mechanisms in an attempt to address the rising carbon dioxide levels. One such mechanism is an increase in respiratory rate. While this may initially help mitigate hypercapnia, it is often unsustainable in the long term, especially in the presence of chronic respiratory diseases or neuromuscular disorders that limit the effectiveness of this compensatory response.
1.1.3.6 Respiratory Acidosis:
As carbon dioxide accumulates in the bloodstream, it combines with water to form carbonic acid, leading to respiratory acidosis. This acidosis, characterised by a decrease in blood pH, can have profound effects on various physiological processes. It not only impacts the respiratory system but also influences cardiovascular function and electrolyte balance.
The pathophysiology of Type 2 Respiratory Failure is a multifaceted interplay of disruptions in gas exchange, respiratory muscle function, and central regulatory mechanisms. This intricate web of factors underscores the complexity of this condition and necessitates a holistic approach to its diagnosis and management.
By unravelling these physiological intricacies, healthcare professionals can tailor interventions that address the specific challenges posed by Type 2 Respiratory Failure, ultimately improving patient outcomes and restoring respiratory equilibrium.
|
Gas Exchange in the Alveoli
?
Ventilation-Perfusion Mismatch
?
Impaired Gas Exchange
?
Respiratory Muscle Weakness
?
Altered Respiratory Drive
?
Compensatory Mechanisms
?
Respiratory Acidosis
?
Respiratory Failure
|
Image 04; Pathophysiology of Type 2 Respiratory Failure
1.1.4 Clinical Presentations of Type2 Respiratory Failure:
Patients with Type 2 Respiratory Failure often present with symptoms such as dyspnea (shortness of breath), increased respiratory rate, and a bluish tint to the skin and mucous membranes due to inadequate oxygenation, known as cyanosis. The severity of these symptoms can vary, ranging from mild respiratory distress to acute respiratory failure requiring immediate medical intervention.
In essence, Type 2 Respiratory Failure encapsulates a complex interplay of physiological factors that disrupt the delicate balance of respiratory function. This condition demands a nuanced understanding of its underlying causes and a tailored approach to management that addresses both the respiratory inefficiency and the associated symptoms.
The clinical manifestations of Type 2 Respiratory Failure are diverse and reflective of the underlying challenges in ventilatory function. This condition, marked by the inability to adequately eliminate carbon dioxide (CO2) from the bloodstream, gives rise to a spectrum of symptoms that encompass respiratory distress, altered physical signs, and systemic effects. Understanding the clinical presentations is crucial for timely diagnosis and effective management.
1.1.4.1 Dyspnea (Shortness of Breath):
Dyspnea, or shortness of breath, stands as a cardinal symptom of Type 2 Respiratory Failure. As the respiratory system grapples with inadequate CO2 elimination, the body responds by increasing respiratory effort. Patients often describe a sense of breathlessness even with minimal exertion, and this symptom becomes more pronounced as the condition progresses.
Dyspnea serves as an early indicator, prompting individuals to seek medical attention, especially those with underlying chronic respiratory diseases.
1.1.4.2 Increased Respiratory Rate:
A noticeable increase in respiratory rate is a characteristic feature of Type 2 Respiratory Failure. The body attempts to compensate for the rising levels of CO2 by prompting more rapid breathing. This compensatory mechanism is a reflection of the struggle to maintain adequate oxygen levels and expel accumulating carbon dioxide.
Clinically, healthcare providers observe an elevated respiratory rate upon examination, a key parameter in assessing the severity of respiratory distress.
1.1.4.3 Use of Accessory Muscles:
In an effort to enhance ventilatory efficiency, individuals with Type 2 Respiratory Failure may engage accessory muscles during breathing. The intercostal muscles and muscles in the neck and shoulders come into play to assist the weakened primary respiratory muscles. This visible use of accessory muscles is an important clinical sign, indicative of the increased workload imposed on the respiratory system.
1.1.4.4 Cyanosis:
Cyanosis, a bluish discoloration of the skin and mucous membranes, is a consequence of inadequate oxygenation. As Type 2 Respiratory Failure progresses, the ability to oxygenate the blood diminishes, leading to this visible sign of hypoxia.
Cyanosis is particularly evident in areas with thinner skin, such as the lips, fingertips, and the perioral region. It serves as a critical indicator of compromised respiratory function and warrants prompt attention.
1.1.4.5. Altered Mental Status:
In severe cases of Type 2 Respiratory Failure, the insufficient oxygenation of the brain can result in altered mental status. Patients may exhibit confusion, lethargy, or even frank disorientation. This neurological manifestation is a red flag, indicating not only the severity of respiratory compromise but also the potential for systemic effects of inadequate oxygen delivery to vital organs.
1.1.4.6 Hypercapnic Encephalopathy:
Hypercapnic encephalopathy refers to neurological dysfunction arising from elevated levels of carbon dioxide in the blood. It can manifest as confusion, drowsiness, or in extreme cases, coma. This complication underscores the systemic impact of Type 2 Respiratory Failure beyond the respiratory system, emphasising the need for comprehensive monitoring and intervention.
1.1.4.7. Respiratory Acidosis:
The accumulation of CO2 in the bloodstream leads to respiratory acidosis: a condition characterised by a decrease in blood pH. This acidosis can contribute to a range of physiological disturbances, affecting cardiovascular function and electrolyte balance. Clinically, healthcare providers may observe signs of acidosis such as increased heart rate and disturbances in consciousness.
1.1.4.8. Systemic Effects:
Type 2 Respiratory Failure is not confined to the respiratory system; it has far-reaching effects on other organ systems. Cardiovascular changes may include an increased heart rate, elevated blood pressure, and eventually, signs of strain on the heart.
Additionally, the kidneys may respond to respiratory acidosis by retaining bicarbonate, further complicating the acid-base balance.
1.1.4.9. Exacerbation of Underlying Conditions:
Individuals with pre-existing chronic respiratory diseases, such as Chronic Obstructive Pulmonary Disease (COPD), may experience exacerbations of their underlying conditions during episodes of Type 2 Respiratory Failure.
The interplay of chronic respiratory disease and acute ventilatory insufficiency can lead to a cascade of symptoms, necessitating targeted interventions to address both acute and chronic aspects of respiratory compromise.
The clinical presentations of Type 2 Respiratory Failure are diverse and multi-faceted, encompassing respiratory distress, altered physical signs, and systemic effects. Recognizing these manifestations is essential for prompt diagnosis and timely intervention.
The comprehensive assessment of dyspnea, changes in respiratory rate, use of accessory muscles, cyanosis, alterations in mental status, and systemic effects provides clinicians with a holistic understanding of the impact of Type 2 Respiratory Failure on the individual, guiding appropriate management strategies and optimising patient outcomes.
1.1.5 Treatment for Type2 Respiratory Failure
Managing Type 2 Respiratory Failure requires a multifaceted approach, addressing both the underlying causes and the symptoms associated with inadequate carbon dioxide (CO2) elimination.
While ventilatory support and non-pharmacological interventions play crucial roles, pharmacotherapy can significantly contribute to optimizing respiratory function. Here, we explore the pharmacological agents commonly employed in the treatment of Type 2 Respiratory Failure, along with their dosages.
1.1.5.1. Pharmacological Treatment
|
Class of the Drug
|
Drug Name
|
|
Bronchodilators
|
Albuterol
|
|
Systemic Corticosteroids
|
Prednisone
|
|
Inhaled Corticosteroids
|
Fluticasone
|
|
Carbonic Anhydrase Inhibitors
|
Acetazolamide
|
|
AntiCholinergics
|
Ipratropium
|
|
Vasopressors
|
Norepinephrine
|
Table 02; Pharmacological Treatment of Type 2 Respiratory Failure
1.1.5.1.1. Bronchodilators:
- Drug Class: Beta-2 agonists (e.g., albuterol)
- Mechanism of Action: Bronchodilators help relieve airway obstruction by relaxing smooth muscle in the bronchioles, facilitating increased airflow.
- Dosage: Albuterol is commonly administered via nebulizer, and the typical dosage is 2.5 mg to 5 mg every 4-6 hours. In severe cases, continuous nebulization may be necessary.
- Drug Class: Anticholinergics (e.g., ipratropium)
- Mechanism of Action: Ipratropium blocks acetylcholine receptors, leading to bronchodilation and reduced airway resistance.
- Dosage: Ipratropium is often administered as 500 mcg to 1 mg via nebulizer every 6 hours.
1.1.5.1.2. Corticosteroids:
- Drug Class: Systemic Corticosteroids (e.g., prednisone)
- Mechanism of Action: Corticosteroids reduce inflammation in the airways, especially in the context of exacerbations in chronic respiratory diseases.
- Dosage: Prednisone is commonly prescribed at a dosage of 40-60 mg daily, with gradual tapering based on clinical response.
- Drug Class: Inhaled Corticosteroids (e.g., fluticasone)
- Mechanism of Action: Inhaled corticosteroids target airway inflammation, reducing the frequency and severity of exacerbations.
- Dosage: Fluticasone is often prescribed at doses ranging from 250 to 500 mcg twice daily, depending on the severity of the underlying respiratory condition.
1.1.5.1.3. Carbonic Anhydrase Inhibitors:
- Drug Class: Acetazolamide
- Mechanism of Action: Acetazolamide promotes bicarbonate excretion, leading to metabolic acidosis, which stimulates ventilation and can help reduce hypercapnia.
- Dosage: Acetazolamide is typically prescribed at doses ranging from 250 mg to 500 mg orally two to three times a day.
1.1.5.1.4. Opioids for Symptom Management:
- Drug Class: Opioids (e.g., morphine)
- Mechanism of Action: Opioids can help alleviate dyspnea by reducing the sensation of breathlessness and anxiety associated with respiratory distress.
- Dosage: Morphine is often administered cautiously, starting at low doses (e.g., 2-5 mg) intravenously and titrating based on the patient's response.
1.1.5.1.5. Norepinephrine for Hemodynamic Support:
- Drug Class: Vasopressors (e.g., norepinephrine)
- Mechanism of Action: In severe cases with cardiovascular compromise, vasopressors can be used to maintain blood pressure and perfusion to vital organs.
- Dosage: Norepinephrine is typically administered as a continuous intravenous infusion, with dosages ranging from 0.05 to 2 mcg/kg/min.
1.5.1.2. Non Pharmacological Treatment
Non-pharmacological treatment for Type 2 Respiratory Failure is tailored to the individual needs of each patient, often involving a combination of these interventions. Collaborative efforts between healthcare professionals, patients, and their families are essential to developing and implementing a comprehensive care plan that addresses both the physiological and psychosocial aspects of respiratory compromise.
Regular reassessment and adjustment of strategies based on the patient's response contribute to optimising outcomes and enhancing overall quality of life.
The initiation and adjustment of pharmacotherapy should be carried out under the supervision of healthcare professionals, taking into account the specific needs and conditions of each patient. Regular monitoring and reassessment are essential to tailor the treatment plan for optimal efficacy and safety.
Non-pharmacological interventions play a crucial role in the comprehensive management of Type 2 Respiratory Failure, focusing on improving respiratory function, providing support, and enhancing overall well-being. Here are key non-pharmacological treatment strategies:
1.5.1.2.1. Oxygen Therapy:
Delivery Methods:
Supplemental oxygen is a cornerstone of non-pharmacological treatment. It can be administered through nasal cannula, simple face mask, Venturi mask, or high-flow nasal cannula depending on the patient's needs and the severity of respiratory failure.
Titration:
Oxygen therapy is titrated to achieve target oxygen saturation levels, often ranging from 88% to 92%. Regular monitoring, including arterial blood gas analyses and continuous pulse oximetry, guides adjustments to maintain optimal oxygenation.
1.5.1.2.2. Non-Invasive Ventilation (NIV):
Devices:
Bi-level Positive Airway Pressure (BiPAP) or Continuous Positive Airway Pressure (CPAP) machines provide ventilatory support without the need for intubation.
Indications:
NIV is beneficial for patients with respiratory distress and hypercapnia. It helps improve ventilation, reduce the work of breathing, and enhance gas exchange.
1.5.1.2.3. Invasive Mechanical Ventilation:
Ventilator Support:
In severe cases where non-invasive measures are inadequate, invasive mechanical ventilation is initiated. Ventilator settings, including tidal volume, respiratory rate, and positive end-expiratory pressure (PEEP), are tailored to individual patient needs.
Monitoring:
Continuous monitoring of ventilator parameters, arterial blood gases, and clinical signs guides adjustments to optimise respiratory support.
1.5.1.2.4. Positioning and Chest Physiotherapy:
Positioning:
Proper positioning, such as elevating the head of the bed, can enhance lung expansion and improve respiratory mechanics. This helps alleviate dyspnea and facilitates effective ventilation.
Chest Physiotherapy:
Techniques such as percussion, vibration, and postural drainage may be employed to mobilise respiratory secretions, aiding in their clearance and preventing complications like pneumonia.
1.5.1.2.5. Respiratory Muscle Training:
Incentive Spirometry:
Encouraging deep breathing through incentive spirometry helps enhance lung expansion, maintain alveolar recruitment, and prevent atelectasis.
Inspiratory Muscle Training:
Specific exercises targeting inspiratory muscles, such as diaphragmatic breathing, can strengthen respiratory muscles and improve overall respiratory function.
1.5.1.2.6. Nutritional Support:
Caloric Intake:
Maintaining adequate nutritional intake is vital for patients with Type 2 Respiratory Failure. Malnutrition can exacerbate respiratory muscle weakness and compromise the body's ability to cope with the increased metabolic demands associated with respiratory distress.
Enteral or Parenteral Nutrition:
In cases where oral intake is insufficient, enteral or parenteral nutrition may be considered to ensure the patient receives adequate calories and nutrients.
1.5.1.2.7. Patient Education and Self-Management:
Disease Education:
Educating patients about their underlying respiratory condition, the importance of medication adherence, and recognizing early signs of exacerbations empowers them to actively manage their health.
Self-Monitoring:
Encouraging patients to monitor their symptoms, oxygen saturation levels, and weight allows for early detection of worsening respiratory function, facilitating timely intervention.
1.5.1.2.8. Psychosocial Support:
Anxiety and Stress Management:
Addressing psychological aspects of respiratory distress is crucial. Psychosocial support, including counselling and relaxation techniques, can help mitigate anxiety and stress, improving overall well-being.
Support Groups:
Connecting patients with support groups or respiratory rehabilitation programs fosters a sense of community and provides a platform for sharing experiences and coping strategies.
1.5.1.2.9. End-of-Life Care and Palliative Measures:
Advanced Care Planning:
In cases where Type 2 Respiratory Failure is part of a chronic and progressive condition, discussions about advanced care planning and end-of-life preferences should be initiated with patients and their families.
Palliative Care:
Palliative care, focused on symptom management and improving quality of life, becomes integral, especially in advanced stages of respiratory failure. In complex cases, consultation with specialists, such as pulmonologists or critical care physicians, is often warranted to ensure comprehensive and personalised care for individuals with Type 2 Respiratory Failure.
1.2 Hypothyroidism
Hypothyroidism is a medical condition characterised by an insufficient production and secretion of thyroid hormones by the thyroid gland. The thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3), play a crucial role in regulating the body's metabolism.

Image 05; Hypothyroidism
Hypothyroidism can arise from various causes, including autoimmune disorders like Hashimoto's thyroiditis, iodine deficiency, or the aftermath of thyroid surgery. This condition manifests through a spectrum of symptoms that reflect its far-reaching impact on the body's homeostasis.
1.2.1. Aetiology of Hypothyroidism
|
Aetiology of Hypothyroidism
|
|
Iatrogenic Causes
|
Medications
|
Other Causes
|
|
|
|
- Hashimoto's Thyroiditis
- Radiation Therapy
- Postpartum Thyroiditis
|
- Radioactive Iodine Therapy for Hyperthyroidism
|
|
- Iodine Deficiency
- Subacute Thyroiditis
- Pituitary or Hypothalamic Dysfunction
|
Table 03; Aetiology of Hypothyroidism
1.2.1.1. Hashimoto's Thyroiditis:
An autoimmune disorder where the immune system attacks the thyroid gland, leading to inflammation and gradual destruction of thyroid tissue.
1.2.1.2. Iatrogenic Causes:
Hypothyroidism may result from treatments such as thyroid surgery or radioactive iodine therapy for hyperthyroidism.
1.2.1.3. Medications:
Certain medications, like lithium and amiodarone, can interfere with thyroid hormone production and contribute to hypothyroidism.
1.2.1.4. Radiation Therapy:
Exposure to radiation, especially in the head and neck region, for the treatment of cancers can damage the thyroid gland and cause hypothyroidism.
1.2.1.5. Congenital Hypothyroidism:
Some individuals are born with an underactive thyroid gland due to genetic factors, leading to congenital hypothyroidism.
1.2.1.6. Iodine Deficiency:
In regions with insufficient dietary iodine, the thyroid gland may not produce enough hormones, resulting in hypothyroidism.
1.2.1.7. Subacute Thyroiditis:
Inflammation of the thyroid gland, often viral in origin, can cause a transient phase of hyperthyroidism followed by hypothyroidism.
1.2.1.8. Pituitary or Hypothalamic Dysfunction:
Disorders affecting the pituitary gland or hypothalamus can disrupt the signalling pathways that regulate thyroid hormone production.
1.2.1.9. Thyroid Surgery:
Surgical removal of part or all of the thyroid gland, often done for thyroid cancer or large goitres, can lead to hypothyroidism.
1.2.1.10. Postpartum Thyroiditis:
Some women may experience inflammation of the thyroid gland after giving birth, which can lead to temporary hypothyroidism.
1.2.2. Epidemiology of Hypothyroidism
Hypothyroidism is a prevalent endocrine disorder globally, with varying incidence rates across different regions. Worldwide, the condition affects a substantial portion of the population, particularly in iodine-deficient areas, and its prevalence increases with age. In India, where iodine deficiency has been a historical concern, the percentage of individuals with hypothyroidism is noteworthy.
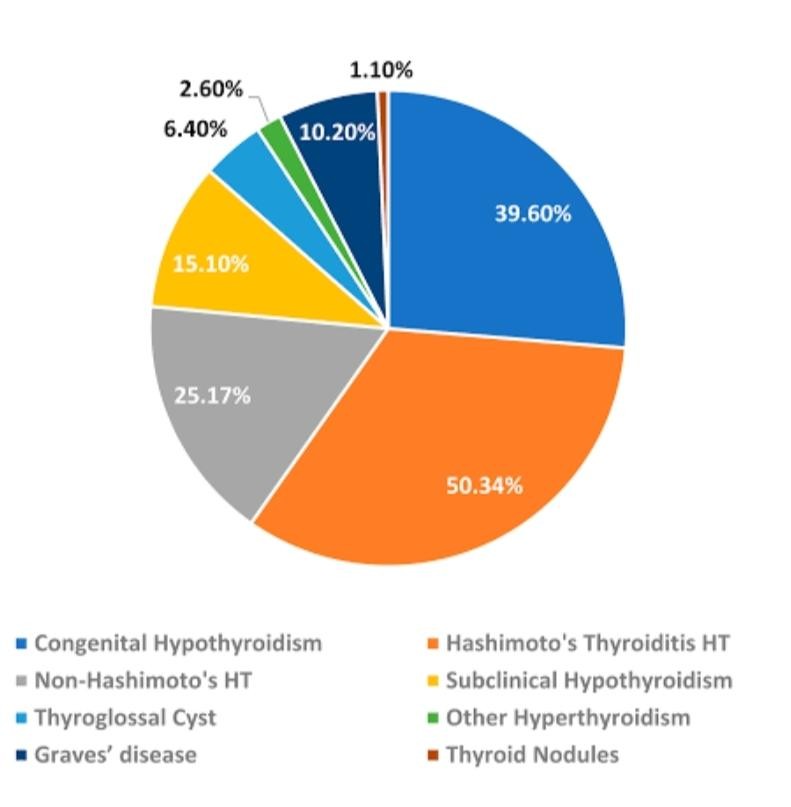
Image 06; Epidemiology of Hypothyroidism
According to estimates, approximately 10% of the Indian population may experience hypothyroidism, reflecting the country's diverse epidemiological landscape. Moreover, the global burden of hypothyroidism is accentuated by the higher susceptibility of women, especially those above 60 years of age.
- It affects around 4-5% of the general population, with a higher incidence in women and the elderly.
- The prevalence of hypothyroidism in India is 11%.
- Whereas, 2% in the UK and 4.6% in the USA.
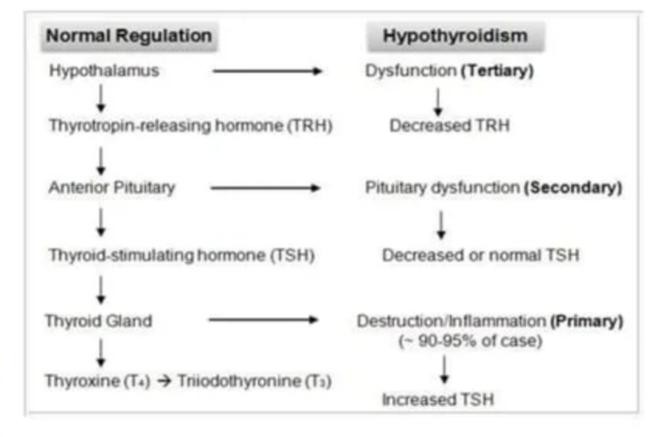
1.2.3. Pathophysiology of Hypothyroidism
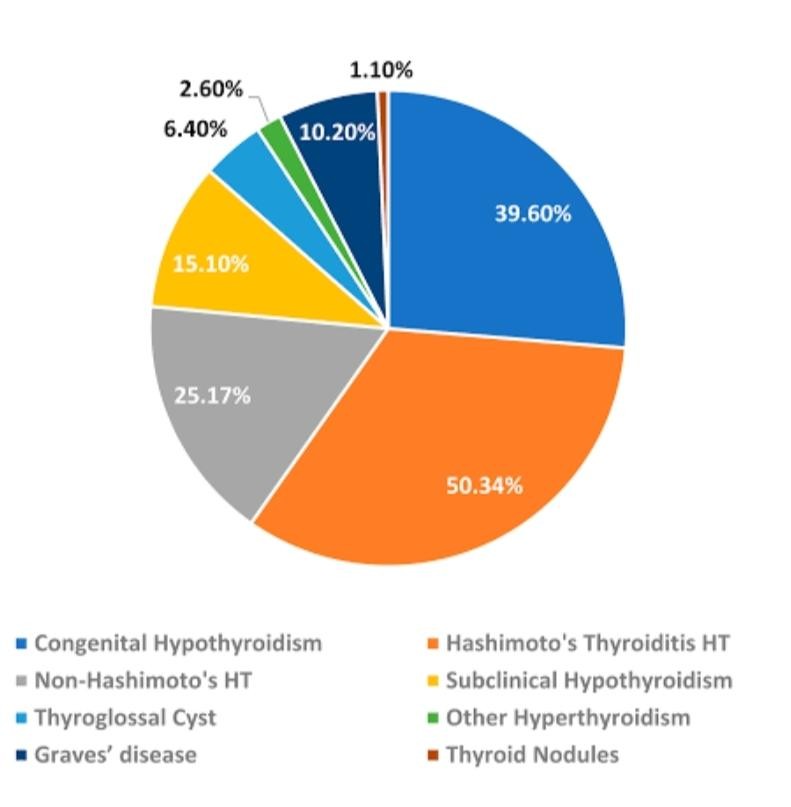
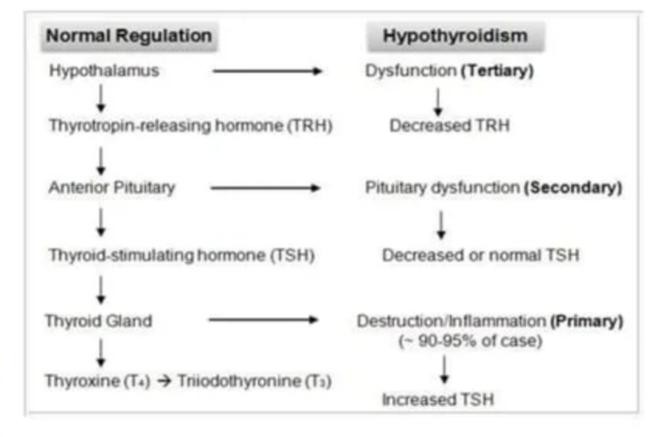
Image 07; Pathophysiology of Hypothyroidism
The pathophysiology of hypothyroidism involves an underactive thyroid gland, leading to insufficient production of thyroid hormones; thyroxine (T4) and triiodothyronine (T3). The most common cause worldwide is autoimmune thyroiditis, known as Hashimoto's disease, where the immune system attacks the thyroid tissue. In iodine-deficient regions, iodine deficiency can also contribute to hypothyroidism.
1.2.4. Clinical Presentations of Hypothyroidism
Hypothyroidism is a condition where the thyroid gland doesn't produce enough thyroid hormones, primarily thyroxine (T4) and triiodothyronine (T3). These hormones play a crucial role in regulating metabolism throughout the body.
Here's an elaboration on the clinical presentations of hypothyroidism.
|
Clinical Presentations of Hypothyroidism
|
|
|
|
|
|
|
|
|
|
|
|
- Muscle weakness and Depression
|
Table 04; Clinical Presentations of Hypothyroidism
- Fatigue: Patients often experience persistent tiredness and lethargy, even after a full night's sleep.
- Weight Gain: Unexplained weight gain may occur despite no significant changes in diet or physical activity.
- Cold Intolerance: Individuals with hypothyroidism may feel unusually sensitive to cold temperatures.
- Dry Skin: Skin may become dry, rough, and pale, with a tendency to itch.
- Constipation: Sluggish bowel movements and constipation are common symptoms of hypothyroidism.
- Menstrual Irregularities: Women may experience changes in their menstrual cycle, including heavier or irregular periods.
- Hair Loss: Thinning of hair and hair loss, including eyebrows, can occur.
- Muscle Weakness: Weakness and aching in the muscles, along with cramps, may be present.
- Depression: Hypothyroidism can contribute to feelings of depression and low mood.
1.2.5. Treatment for Hypothyroidism
1.2.5.1 Non pharmacological Treatment
It's essential to note that while these non-pharmacological approaches can complement medical treatment, they are not substitutes for thyroid hormone replacement therapy when clinically indicated. Consultation with a healthcare professional is crucial for personalised advice and proper management of hypothyroidism.
1.2.5.1.1. Dietary Changes:
- Ensure sufficient iodine intake, as iodine is essential for thyroid hormone synthesis.
- Include selenium-rich foods, as selenium supports thyroid function.
1.2.5.1.2. Nutritional Supplements:
Consider vitamin and mineral supplements, such as vitamin D and B vitamins, to support overall health.
1.2.5.1.3. Lifestyle Modifications:
- Maintain a healthy and balanced diet to support overall well-being.
- Engage in regular exercise to boost metabolism and energy levels.
1.2.5.1.4. Stress Management:
Practice stress-reducing techniques like meditation, yoga, or deep breathing, as stress can impact thyroid function.
1.2.5.1.5. Avoid Goitrogenic Foods:
Limit the intake of goitrogenic foods, such as soy, cabbage, and broccoli, which can interfere with thyroid function.
1.2.5.1.6. Adequate Sleep:
Ensure sufficient and quality sleep, as sleep plays a role in overall hormonal balance.
1.2.5.1.7. Limit Processed Foods:
Reduce the consumption of processed foods and refined sugars, which can contribute to inflammation and impact thyroid health.
1.2.5.1.8. Gluten Restriction:
Some individuals with hypothyroidism may benefit from a gluten-free diet, as gluten sensitivity can be associated with thyroid issues.
1.2.5.1.9. Regular Monitoring:
Regularly monitor thyroid function through blood tests to track progress and adjust lifestyle strategies accordingly.
1.2.5.2. Pharmacological Treatment
Pharmacological treatment for hypothyroidism typically involves thyroid hormone replacement therapy. Here are key points about this treatment:
|
Pharmacological Treatment for Hypothyroidism
|
|
Class of the Drug
|
Drug Name
|
|
Synthetic Thyroid Hormone
|
- Levothyroxine Sodium(T4)
- Liothyronine Sodium(T3)
|
|
Combination Therapy
|
- Levothyroxine/ Liothyronine combination
|
|
Natural Thyroid Hormone Extract
|
- Desiccated Thyroid Extract(DTE)
|
Table 05; Pharmacological Treatment of Hypothyroidism
1.2.5.2.1. Levothyroxine Sodium (T4) - Synthetic Thyroid Hormone:
- Drug Class: Synthetic Thyroid Hormone.
- Dosages: Individualised, starting around 25-50 micrograms, with adjustments based on response.
- Mechanism of Action: Converts to triiodothyronine (T3) in the body, regulating metabolism.
1.2.5.2.2. Liothyronine Sodium (T3) - Synthetic Thyroid Hormone:
- Drug Class: Synthetic Thyroid Hormone.
- Dosages: Lower than levothyroxine, starting around 5-25 micrograms.
- Mechanism of Action: Directly active form of thyroid hormone (T3), influencing metabolic processes.
1.2.5.2.3. Levothyroxine/Liothyronine Combination:
- Drug Class: Combination Therapy.
- Dosages: Varies; combination of both T4 and T3 for individuals who may benefit.
- Mechanism of Action: Provides both T4 and T3 hormones.
1.2.5.2.4. Desiccated Thyroid Extract (DTE):
- Drug Class: Natural Thyroid Hormone Extract.
- Dosages: Contain both T4 and T3; dosage varies based on the brand.
- Mechanism of Action: Derived from animal thyroid glands, providing a combination of thyroid hormones.
It's important to note that while levothyroxine is the standard and is effective for most patients, alternative formulations or combinations may be considered in certain situations. The choice of medication depends on individual factors, including the severity of hypothyroidism, patient preferences, and response to treatment.
Always consult with a healthcare professional for personalised advice and to determine the most appropriate medication and dosage for your specific needs. Regular monitoring through blood tests is crucial to ensure optimal thyroid function.
02. Aims & Objectives
2.1. Aim
To determine the incidence of Type2 Respiratory Failure in Hypothyroidism at tertiary care hospital.
2.2. Objectives
- To evaluate the incidence of type2 Respiratory Failure in Hypothyroidism.
- To improve the quality of life of patients.
- To improve the wellbeing of patients.
MATERIALS AND METHODS
3.1 Literature Review
- Munehisa Fukusumi et al: Respiratory failure associated with hypoventilation in a patient with severe hypothyroidism. Severe lack of thyroid hormone affects breathing in a 70 year old patient. Patient’s breathing problems are not better. It is hard to manage thyroid related breathing issues.
- Ramadan M. Nafae et al.: Thyroid function in Respiratory failure Patients. Assess how thyroid function and hormone replacement affect outcomes in respiratory failure. ESS in respiratory failure patients correlates with disease severity, prolonging mechanical ventilation.
- Hyucki kwon et al.: Respiratory Failure induced by severe Hypothyroidism in a Korean Women. Explore if severe hypothyroidism causes respiratory failure and weaning issues. Successful recovery and ventilator weaning post thyroid hormone replacement. Suggest a link between severe hypothyroidism and respiratory challenges.
- Douglas C Johnson et al.:Respiratory function in thyroid disease. Investigate how thyroid diseases affect breathing, outlining their links to specific lung issues. Identification of diverse breathing problems associated with various thyroid conditions.
- Sorensen JR et al.: Respiratory manifestations of hypothyroidism. Prevalence and mechanisms of respiratory issues in hypothyroidism. Provide a comprehensive understanding of the relationship between hypothyroidism and respiratory issues.
- Vincent S. Mirabile et al.: Respiratory Failure in Adults. Aims to review the aetiology, pathophysiology, physical exam findings, and treatment considerations for patients with respiratory failure. The goals of ventilatory support in respiratory failure, common indications for mechanical ventilation, and the epidemiology of respiratory failure. The outcome is to provide healthcare professionals with a comprehensive understanding of respiratory failure in adults to improve the evaluation and management of this condition.
- Nicola Vargas et al. 2014: Type 2 respiratory failure and falls in elderly adults: beware of the thyroid! The association between type 2 respiratory failure and falls in elderly adults with hypothyroidism. The case of an elderly patient with myxedema coma due to Hashimoto's thyroiditis and type 2 acute respiratory failure who presented with falls. Raises awareness among healthcare professionals about the potential link between respiratory failure and falls in elderly patients with hypothyroidism
- Seethalakshmi Krishna Iyer et al.: An Analysis of Dynamic Pulmonary Functions of Hypothyroid Patients. This analyze the dynamic pulmonary functions of hypothyroid patients. The study likely investigates how hypothyroidism affects respiratory function. The outcome may reveal insights into the respiratory challenges faced by individuals with hypothyroidism.
- Shahid Muhammad et al.: Physiology, Thyroid Hormone. This is likely to explore the physiological aspects of thyroid hormones. It provides insights into the roles and functions of thyroid hormones in the body, shedding light on their impact on overall physiology and health.
- Rebecca S Bahn Chair et al.: Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. This provides management guidelines for hyperthyroidism and other causes of thyrotoxicosis, as endorsed by the American Thyroid Association and American Association of Clinical Endocrinologists. It likely includes comprehensive recommendations for the diagnosis and treatment of hyperthyroid conditions, aiming to guide clinicians in effectively managing patients with thyroid disorders.
- Nikita Patil et al.: Hypothyroidism (Nursing). This is likely to address nursing considerations in the context of hypothyroidism. If include insights into the nursing care strategies, challenges, and best practices associated with patients experiencing hypothyroidism. The focus is likely on enhancing the understanding and care provided by nursing professionals for individuals with hypothyroid conditions.
- CODRUTA LENCU et al.: Respiratory manifestations in endocrine diseases. It explores respiratory manifestations in various endocrine diseases. This likely involves identifying and describing the respiratory symptoms associated with different endocrine disorders, providing valuable insights for healthcare professionals to recognize and manage respiratory complications in patients with endocrine conditions.
- Fu-Ping Guo et al.: Clinical features of respiratory failure secondary to hypothyroidism. This examines the clinical features of respiratory failure secondary to hypothyroidism. Detailing the specific respiratory complications observed in individuals with hypothyroidism, aiming to enhance understanding and facilitate better management of respiratory issues in patients with this endocrine disorder.
- Chaitanya PS et al.: Respiratory dysfunction in hypothyroidism. Journal of Clinical and Scientific Research. This is to investigate respiratory dysfunction in hypothyroidism, as published in the Journal of Clinical and Scientific Research. This includes findings on how hypothyroidism impacts respiratory function, potentially contributing valuable insights for clinicians and researchers in understanding and managing respiratory complications associated with this thyroid disorder.
- Tibullo L et al.: Type 2 respiratory failure and falls in elderly adults. This explores the association between type 2 respiratory failure and falls in elderly adults. Identifying correlations between respiratory issues and falls among the elderly, contributing valuable information for healthcare professionals in developing strategies to address both respiratory health and fall prevention in this population.
- Kim BR et al.: Respiratory failure induced by severe hypothyroidism in a Korean Woman. This presents a case study of respiratory failure induced by severe hypothyroidism in a Korean woman. Detailing the clinical manifestations, diagnostic approaches, and management strategies in addressing respiratory complications associated with severe hypothyroidism, providing insights for healthcare practitioners encountering similar cases.
- Navy EA et al.: Thyroid function in mechanically ventilated patients with acute respiratory failure: Prognostic value and its relation to high-sensitivity C-reactive protein. Investigating the thyroid function in mechanically ventilated patients with acute respiratory failure and its prognostic value. Assessing the relationship between thyroid function and high-sensitivity C-reactive protein levels, providing insights into potential markers for prognosis in critically ill patients with respiratory failure.
- Sadek SH et al.: Pulmonary consequences of hypothyroidism. To examine the pulmonary consequences of hypothyroidism. Detailing how hypothyroidism impacts the respiratory system, potentially contributing valuable insights for healthcare professionals in understanding and managing pulmonary issues associated with this endocrine disorder.
- Vrigkou E et al.: The Role of Thyroid Disorders, Obesity, Diabetes Mellitus and Oestrogen Exposure as Potential Modifiers for Pulmonary Hypertension. To investigate the role of thyroid disorders, obesity, diabetes mellitus, and oestrogen exposure as potential modifiers for pulmonary hypertension. Examining the interplay between these factors and pulmonary hypertension, offering insights into potential modifiers that could influence the development or progression of this condition.
- Scicchitano P et al.: Pulmonary hypertension in thyroid diseases. Exploring the relationship between thyroid diseases and pulmonary hypertension. This include insights into the prevalence, mechanisms, and clinical implications of pulmonary hypertension in individuals with thyroid disorders, contributing valuable information for healthcare professionals managing patients with these conditions.
- Chaker L et al.: Hypothyroidism. An overview or in-depth analysis of hypothyroidism. Discussing the causes, symptoms, and management strategies for hypothyroidism, offering comprehensive insights for healthcare practitioners and individuals seeking information about this thyroid disorder.
- Deligiorgi MV et al.: The clinical relevance of hypothyroidism in patients with solid non-thyroid cancer. Assess the clinical relevance of hypothyroidism in patients with solid non-thyroid cancer. Impact of hypothyroidism on cancer outcomes, treatment responses, and overall patient well-being, providing valuable insights for healthcare professionals managing individuals with both hypothyroidism and non-thyroid cancers.
- Palace MR et al.: Perioperative management of thyroid dysfunction. Addressing the perioperative management of thyroid dysfunction. The outcome may involve offering guidance and recommendations for healthcare professionals on how to effectively manage thyroid disorders before, during, and after surgical procedures, ensuring optimal patient care and outcomes in the perioperative period.
- Cappola AR et al.: Thyroid and cardiovascular disease. Exploring the relationship between thyroid function and cardiovascular disease. The outcome may involve discussing the impact of thyroid disorders on cardiovascular health, potential mechanisms linking the two, and implications for managing cardiovascular risk in individuals with thyroid conditions, providing valuable insights for clinicians in the field.
- Tagami T et al.: The incidence of gestational hyperthyroidism and postpartum thyroiditis in treated patients with Graves' disease. The purpose of the article is likely to investigate the incidence of gestational hyperthyroidism and postpartum thyroiditis in individuals treated for Graves' disease. The outcome may include insights into the frequency of these thyroid-related complications during pregnancy and postpartum periods in patients with a history of Graves' disease, contributing valuable information for healthcare practitioners managing thyroid disorders in pregnant individuals.
- Bonnesen B et al.: Management of COVID-19-associated acute respiratory failure with alternatives to invasive mechanical ventilation: high-flow oxygen, continuous positive airway pressure, and noninvasive ventilation. Diagnostics. The purpose of the article is likely to explore the management of COVID-19-associated acute respiratory failure using alternatives to invasive mechanical ventilation, such as high-flow oxygen, continuous positive airway pressure, and noninvasive ventilation. The outcome may involve providing recommendations and insights into the effectiveness of these alternative respiratory support strategies, aiming to guide clinicians in optimising care for COVID-19 patients experiencing acute respiratory distress.
3.2 Methodology
- Study design: Prospective observational study design.
- Study site: Pulmonology, General medicine department of Narayana Medical College and Hospital, Nellore, Andhra Pradesh.
- Study duration: Conducted over a period of six months (September to February).
- Study population: Approximately 200 patients as per inclusion criteria.
- Study criteria: Patients are considered for the study based on inclusion and exclusion criteria.
- Inclusion Criteria
- Patients with hypothyroidism.
- Patients with disease of age 30 to 80 years (both male and female).
- Patients with other comorbid conditions.
- Patients willing to provide the information.
- Exclusion Criteria
- Pregnant and lactating women.
- Patients <30>80 years.
- Lack of interest to give information.
- Whose verbal communication was poor
- Study Materials
- Patient informed consent
- A specially designed Questionnaire form on Type II Respiratory failure in hypothyroidism.
3.3 Data or statistical analysis:
- The study will be initiated after obtaining the permission from the Review Ethical Board (REB).
- The data for the present study will be collected by patient interview chart and chart review method.
- Data was entered in Microsoft Excel and analysed.
RESULTS
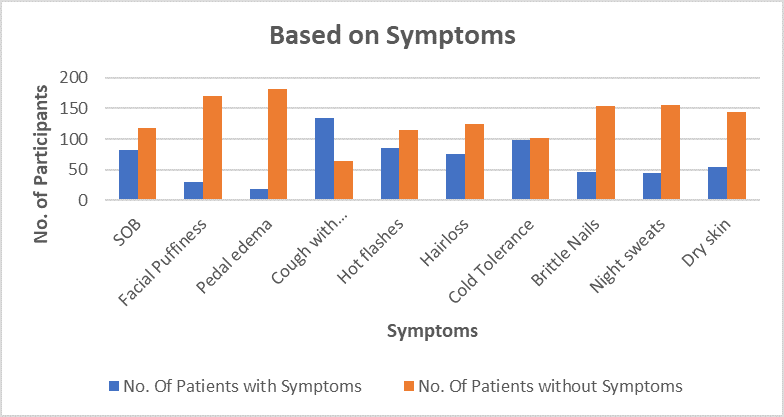
4.1 Based on Symptoms
|
Clinical Manifestations
|
No. Of Patients with Symptoms
|
No. Of Patients without Symptoms
|
|
SOB
|
82
|
118
|
|
Facial puffiness
|
30
|
170
|
|
Pedal edema
|
18
|
182
|
|
Cough with sputum
|
135
|
65
|
|
Hot flashes
|
85
|
115
|
|
Hair loss
|
76
|
124
|
|
Cold tolerance
|
98
|
102
|
|
Brittle Nails
|
46
|
154
|
|
Night sweats
|
45
|
155
|
|
Dry skin
|
55
|
145
|
Table 06; Results based on Symptoms
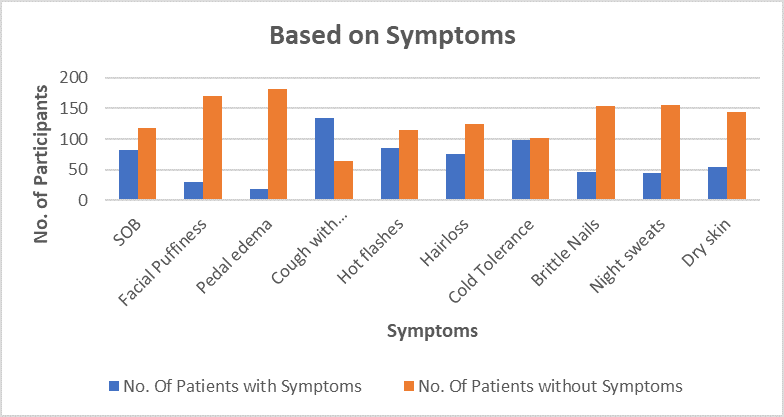
Cough with sputum is the most common symptom observed.
|
Age Group
|
No. Of Participants
|
No. Of Patients with T2RF
|
|
30-40
|
18
|
5
|
|
41-50
|
46
|
23
|
|
51-60
|
70
|
25
|
|
61-70
|
59
|
27
|
|
71-80
|
7
|
2
|
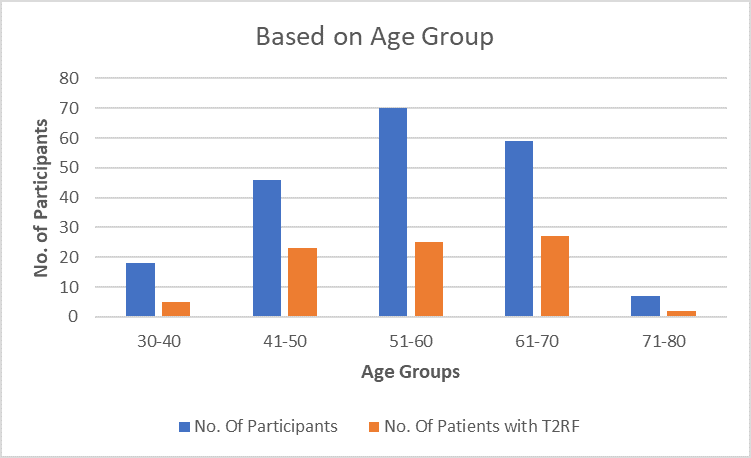
Table 07; Results based on Age groups
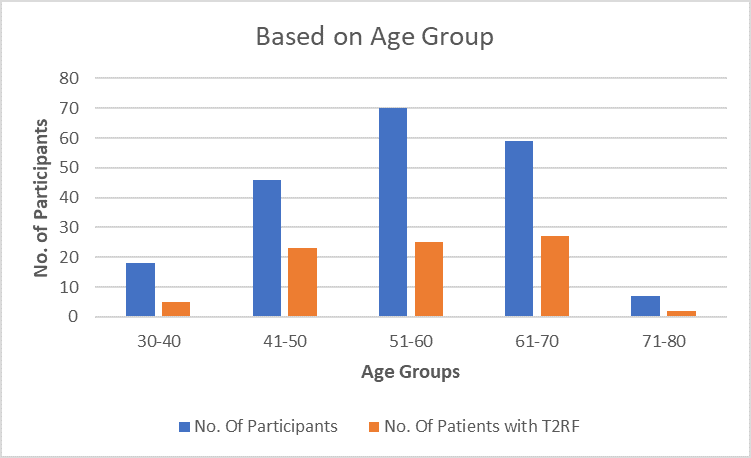
Type2 respiratory failure is observed mostly between the age groups of 51-60 and 61-70.
|
Gender
|
No.of Participants
|
No.of Participants with T2RF
|
|
Male
|
86
|
35
|
|
Female
|
114
|
47
|
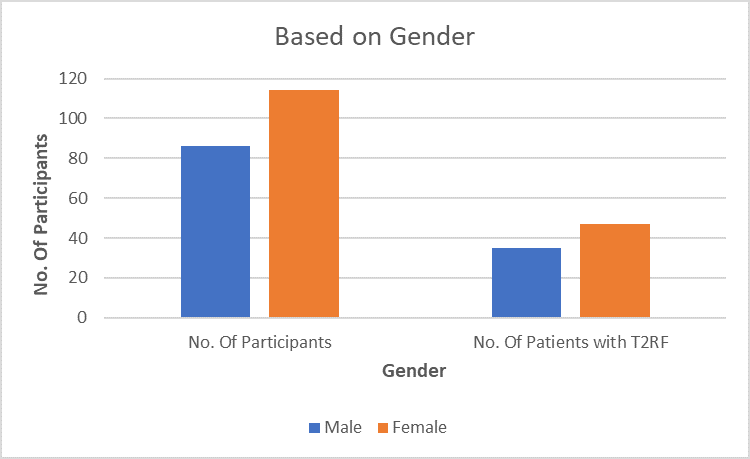
Table 08; Results based on Gender
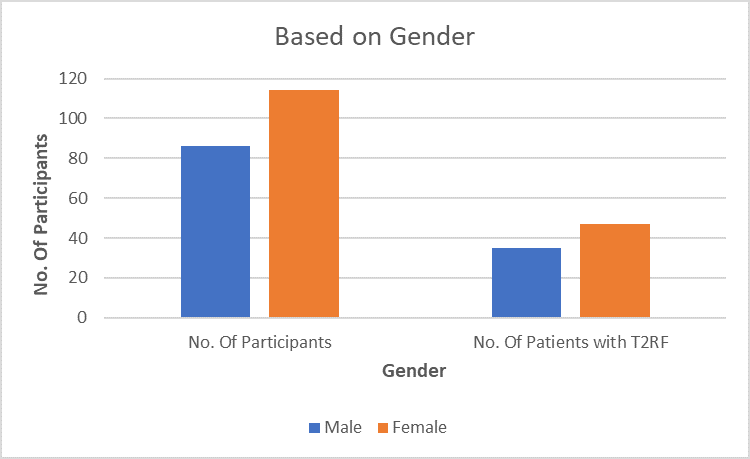
Females have high chances of getting T2RF.
4.4 Based on Risk Factors
|
Risk Factors
|
No. Of Patients
|
|
Radiation Exposure
|
33
|
|
Medication Exposure
|
24
|
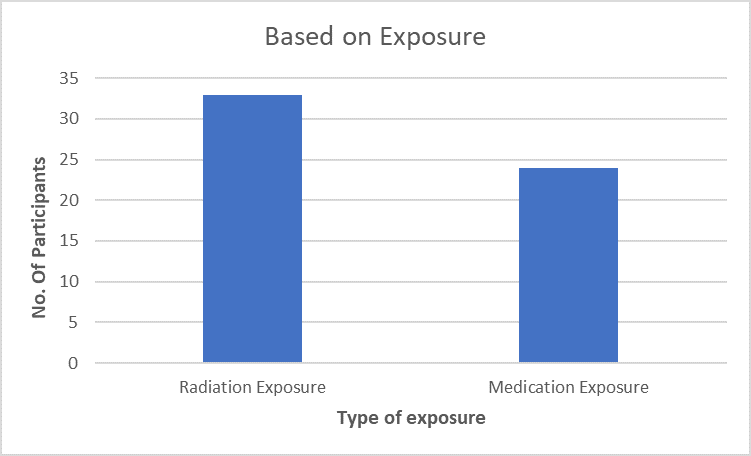
Table 09; Results based on Risk Factors
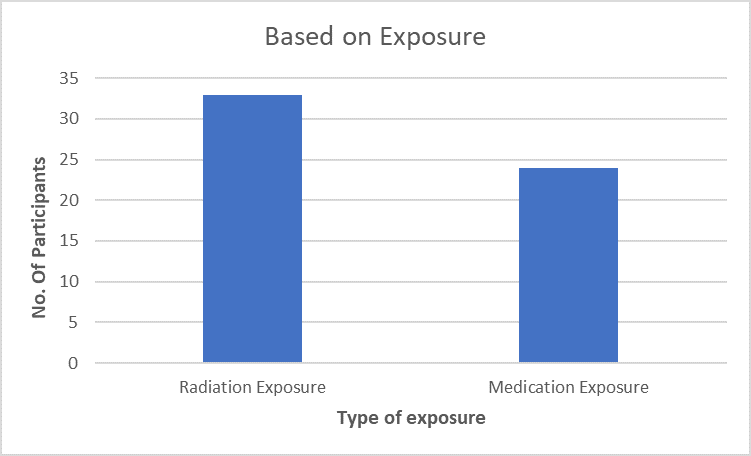
Radiation exposure is the leading cause to get T2RF.
4.5 Based on Comorbidities
|
Comorbidities
|
No.of Participants
|
No.of Participants with T2RF
|
|
DM
|
52
|
13
|
|
HTN
|
64
|
15
|
|
COPD
|
35
|
16
|
|
CAD
|
21
|
10
|
|
CKD
|
24
|
9
|
|
Pneumonia
|
4
|
2
|
|
OSA
|
6
|
5
|
|
Bronchial asthma
|
4
|
2
|
|
Others
|
20
|
14
|
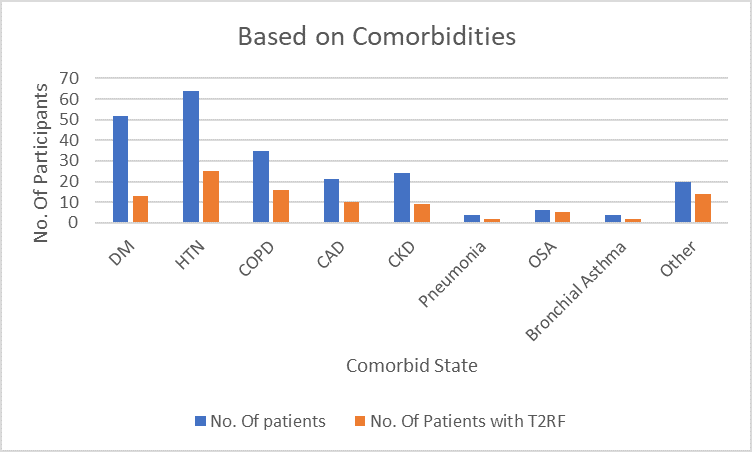
Table 10; Results based on Comorbidities
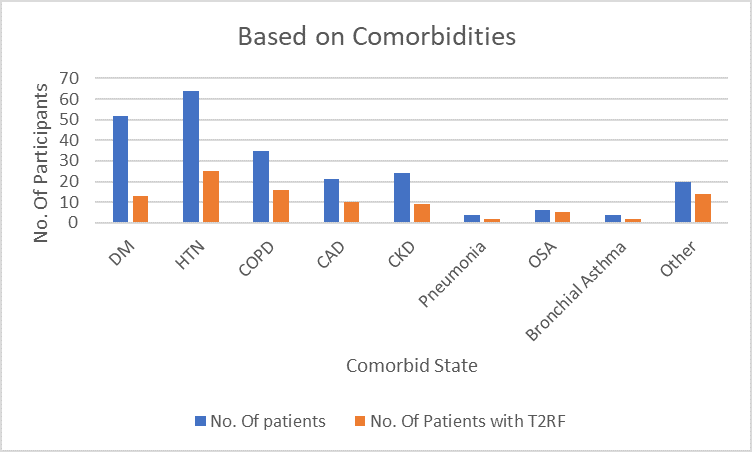
HTN, DM are the comorbidities present in most of the people causing T2RF.
DISCUSSION
A total number of 200 patients were selected for the study with various parameters. The parameters included were:
- Age of the patient
- Gender of the patient
- Symptoms experienced by the patient
- Exposure
- Comorbidities
Out of 200 participants, 82 patients have T2RF. By percentage calculation, the incidence of Type2 Respiratory failure in Hypothyroidism is 41%.
Graph1 outlines various clinical manifestations and the number of patients exhibiting each symptom. Shortness of breath affects 82 patients, while cough with sputum is prevalent in 135 patients. Facial puffiness is reported by 30 patients, pedal edema by 18, and hot flashes by 85. Hair loss affects 76 patients, cold tolerance is compromised in 98, and brittle nails are observed in 46 patients. Night sweats are reported by 45 patients, and dry skin affects 55.
Graph 2 categorises participants into age groups and reveals the incidence of Type 2 Respiratory Failure (T2RF) within each group. Among those aged 30-40, 5 out of 18 participants have T2RF. In the 41-50 age bracket, 23 out of 46 individuals have T2RF. The trend continues with 25 out of 70 participants aged 51-60, and 27 out of 59 individuals aged 61-70 experiencing T2RF. Among the smallest age group of 71-80, 2 out of 7 participants have T2RF. This data underscores the increasing incidence of T2RF with advancing age, highlighting the importance of tailored interventions and care for older populations prone to respiratory complications.
Graph 3 presents a breakdown of participants by gender and reveals the incidence of Type 2 Respiratory Failure (T2RF) within each gender category. Among the 86 male participants, 35 individuals have been diagnosed with T2RF, while among the 114 female participants, 47 individuals exhibit symptoms of T2RF. This indicates a higher incidence of T2RF among females compared to males within the sampled population.
Graph 4 outlines the incidence of specific risk factors among patients, namely radiation exposure and medication exposure. Out of the total number of patients studied, 33 individuals have been exposed to radiation, while 24 individuals have encountered medication-related exposure as potential risk factors. This information sheds light on the importance of considering various environmental and medical factors that may contribute to health conditions.
Graph 5 outlines the incidence of comorbidities among patients with Type 2 Respiratory Failure (T2RF), shedding light on the overlap of various health conditions within this population. Among the patients studied, diabetes mellitus (DM) affects 52 individuals, with 13 of them also having T2RF. Similarly, hypertension (HTN) is present in 64 patients, with 25 of them exhibiting T2RF. Chronic obstructive pulmonary disease (COPD) is observed in 35 patients, with 16 of them also having T2RF, while coronary artery disease (CAD) affects 21 patients, with 10 of them having T2RF. Additionally, chronic kidney disease (CKD) is documented in 24 individuals, with 9 of them exhibiting T2RF. A smaller number of patients present with pneumonia (4), obstructive sleep apnea (OSA) (6), and bronchial asthma (4), with 2, 5, and 2 of them respectively also having T2RF. Furthermore, 20 patients have other comorbidities not specified in the data, with 14 of them having T2RF.
CONCLUSION
The study findings underscore a significant prevalence of Type 2 Respiratory Failure (T2RF) within the sampled population, with 82 out of 200 participants experiencing T2RF, representing a notable 41% incidence rate. The manifestation of symptoms such as shortness of breath and cough with sputum emphasizes the clinical complexity of T2RF and its impact on patient well-being.
Environmental factors, including radiation exposure and medication history, emerge as potential contributors to T2RF development. Among the studied patients, 33 individuals have been exposed to radiation, while 24 participants have encountered medication-related exposure, suggesting the importance of considering various environmental and medical factors in understanding respiratory health conditions.
The analysis of comorbidities reveals an overlapping relationship between T2RF and other health conditions, such as diabetes mellitus, hypertension, chronic obstructive pulmonary disease (COPD), coronary artery disease (CAD), and chronic kidney disease (CKD). The coexistence of these conditions highlights the complexity of T2RF and underscores the need for comprehensive patient assessment and management strategies.
Gender disparities in T2RF incidence are evident, with a higher prevalence among females compared to males within the sampled population. This finding emphasizes the importance of tailoring interventions to address gender-specific risk factors and physiological differences contributing to respiratory dysfunction.
Age-wise distribution further elucidates the increasing incidence of T2RF with advancing age, emphasizing the necessity for tailored interventions and care for older populations prone to respiratory complications. The age group analysis reveals a progressive increase in T2RF incidence from 30-40 years to 71-80 years, highlighting the vulnerability of older individuals to respiratory complications.
Understanding the interplay of symptoms, demographics, environmental exposures, and comorbidities is crucial for developing comprehensive management strategies targeting T2RF in diverse patient populations. Tailored interventions addressing age-specific risks, gender disparities, and environmental factors are essential for optimizing patient outcomes and improving respiratory health in hypothyroidism.
REFERENCES
- Fukusumi M, Iidaka T, Mouri A, Hamamoto Y, Kamimura M. Respiratory failure associated with hypoventilation in a patient with severe hypothyroidism. Respirology Case Reports. 2014 Jun;2(2):79-80.
- Nafae RM, Mohammed MA, Morsi AF, Ibrahim DA. Thyroid function in respiratory failure patients. Egyptian Journal of Chest Diseases and Tuberculosis. 2014 Apr 1;63(2):513-21.
- Kwon H, Kim BR, Han SS, Hong Y. Respiratory failure induced by severe hypothyroidism in a Korean Woman. Soonchunhyang Medical Science. 2016 Jun 30;22(1):35-7.
- Shebl E, Mirabile VS, Sankari A, Burns B. Respiratory failure
- Vargas N, Tibullo L, Carifi S, Cucciniello A, Landi E, Barbella MR, Di Grezia F. Type 2 respiratory failure and falls in elderly adults: beware of the thyroid!. Journal of the American Geriatrics Society. 2014 Oct;62(10):2026-7.
- Sorensen JR, Winther KH, Bonnema SJ, Godballe C, Hegedüs L. Respiratory manifestations of hypothyroidism: a systematic review. Thyroid. 2016 Nov 1;26(11):1519-27.
- Iyer SK, Menon SK, Bahuleyan B. An analysis of dynamic pulmonary functions of hypothyroid patients. Journal of clinical and diagnostic research: JCDR. 2017 Mar;11(3):CC10.
- Shahid MA, Ashraf MA, Sharma S. Physiology, thyroid hormone.
- American Thyroid Association and American Association of Clinical Endocrinologists Taskforce on Hyperthyroidism and Other Causes of Thyrotoxicosis, Bahn RS, Burch HB, Cooper DS, Garber JR, Greenlee MC, Klein I, Laurberg P, McDougall IR, Montori VM, Rivkees SA. Hyperthyroidism and other causes of thyrotoxicosis: management guidelines of the American Thyroid Association and American Association of Clinical Endocrinologists. Thyroid. 2011 Jun 1;21(6):593-646.
- Patil N, Rehman A, Jialal I, Saathoff AD. Hypothyroidism (Nursing).
- Lencu C, Alexescu T, Petrulea M, Lencu M. Respiratory manifestations in endocrine diseases. Clujul Medical. 2016;89(4):459.
- Guo FP, Xu TD, Du TK, Wang HL. Clinical features of respiratory failure secondary to hypothyroidism. Zhongguo yi xue ke xue Yuan xue bao. Acta Academiae Medicinae Sinicae. 2008 Apr 1;30(2):153-5.
- Chaitanya PS, Suresh V, Mohan A, Sachan A. Respiratory dysfunction in hypothyroidism. Journal of Clinical and Scientific Research. 2019 Apr 1;8(2):89-94.
- Tibullo L, Carifi S, Cucciniello A, Landi E, Barbella MR, Di Grezia F. Type 2 respiratory failure and falls in elderly adults: beware of the thyroid!. Journal of the American Geriatrics Society. 2015 Oct;52(10):2026-7.
- Kim BR, Han SS, Hong Y. Respiratory failure induced by severe hypothyroidism in a Korean Woman. Soonchunhyang Medical Science. 2014 Jun 29;22(1):35-7.
- Naby EA, Selim S, Mohsen M, Helmy M. Thyroid function in mechanically ventilated patients with acute respiratory failure: Prognostic value and its relation to high-sensitivity C-reactive protein. Egyptian Journal of Chest Diseases and Tuberculosis. 2015 Jan 1;64(1):175-81.
- Sadek SH, Khalifa WA, Azoz AM. Pulmonary consequences of hypothyroidism. Annals of thoracic medicine. 2017 Jul;12(3):204.
- Vrigkou E, Vassilatou E, Dima E, Langleben D, Kotanidou A, Tzanela M. The Role of Thyroid Disorders, Obesity, Diabetes Mellitus and Estrogen Exposure as Potential Modifiers for Pulmonary Hypertension. Journal of Clinical Medicine. 2022 Feb 10;11(4):921.
- Scicchitano P, Dentamaro I, Tunzi F, Ricci G, Carbonara S, Devito F, Zito A, Ciampolillo A, Ciccone MM. Pulmonary hypertension in thyroid diseases. Endocrine. 2016 Dec;54:578-87.
- Chaker L, Razvi S, Bensenor IM, Azizi F, Pearce EN, Peeters RP. Hypothyroidism (Primer). Nature Reviews: Disease Primers. 2022;8(1).
- Deligiorgi MV, Trafalis DT. The clinical relevance of hypothyroidism in patients with solid non-thyroid cancer: a tantalizing conundrum. Journal of Clinical Medicine. 2022 Jun 14;11(12):3417.
- Palace MR. Perioperative management of thyroid dysfunction. Health services insights. 2017 Feb 17;10:1178632916689677.
- Cappola AR, Desai AS, Medici M, Cooper LS, Egan D, Sopko G, Fishman GI, Goldman S, Cooper DS, Mora S, Kudenchuk PJ. Thyroid and cardiovascular disease: research agenda for enhancing knowledge, prevention, and treatment. Circulation. 2019 Jun 18;139(25):2892-909.
- Tagami T, Hagiwara H, Kimura T, Usui T, Shimatsu A, Naruse M. The incidence of gestational hyperthyroidism and postpartum thyroiditis in treated patients with Graves' disease. Thyroid. 2007 Aug 1;17(8):767-72.
- Bonnesen B, Jensen JU, Jeschke KN, Mathioudakis AG, Corlateanu A, Hansen EF, Weinreich UM, Hilberg O, Sivapalan P. Management of COVID-19-associated acute respiratory failure with alternatives to invasive mechanical ventilation: high-flow oxygen, continuous positive airway pressure, and noninvasive ventilation. Diagnostics. 2021 Dec 2;11(12):2259


 Sayad maseera fathima *
Sayad maseera fathima *
 Arshad shaik
Arshad shaik

 10.5281/zenodo.14030809
10.5281/zenodo.14030809