Abstract
Neurological diseases (NDs) are a major global health challenge, with the WHO ranking them as a leading cause of death. Dementia cases are expected to rise from 24.3 million in 2001 to over 81 million by 2040 due to aging populations. This review focuses on Alzheimer’s disease (AD), characterized by amyloid-beta plaques, neurofibrillary tangles, and neuronal loss. Advances in genetics, biomarkers, and imaging have improved early diagnosis and understanding of its mechanisms. Treatment strategies target symptoms, lifestyle changes, and emerging therapies like nanomaterials, immunotherapy, and drugs addressing oxidative stress and inflammation. Epidemiological studies highlight potential protective roles of cholesterol-lowering agents, hormones, and antioxidants, though trial results vary. Future research prioritizes preclinical phases, cellular mechanisms, and precision medicine. Despite progress, AD remains a complex challenge requiring sustained research efforts.
Keywords
Neurological diseases, Alzheimer's Dieases, biomarkers, hormones, Despite progress.
Introduction
The primary cause of dementia, Alzheimer’s disease, is rapidly rising to the top of the list of this century’s most costly, deadly, and debilitating illnesses. Significant advancements have been made in our understanding of the underlying pathology, the identification of several protective and causative genes, the discovery of novel blood-based and imaging biomarkers, and the first tentative indications of the beneficial effects of lifestyle changes and disease-modifying therapies1. Giving the reader current information about Alzheimer’s disease is the goal of this new seminar2. An international panel of dementia specialists was assembled by Alzheimer’s Disease International to conduct an evidence-based Delphi consensus on the prevalence of dementia globally. The Delphi study2 projected that the number of dementia sufferers worldwide will increase from an estimated 24.3 million in 2001 to 42.3 million in 2020 and 81.1 million by 20403. There are regional variations in the quality of data on the prevalence of Alzheimer’s disease, and significant issues still surround whether regional variations in age-specific prevalence are genuine or the product of various research approaches4.
2. Review Of Literature: –
|
1.
|
Scheltens P, Blennow K, Breteler MM, et al.
|
Treatement of Alzheimer’s disease
|
Alzheimer disease
|
|
2.
|
Wu YT, Beiser AS, Breteler MMB, et al.
|
The changing prevalence and incidence of dementia over time current evidence.
|
Forgetful and decline memory
|
|
3.
|
Terry AV Jr, Buccafusco JJ, et al
|
The cholinergic hypothesis of age and Alzheimer’s disease-related cognitive defi cits: recent challenges and their implications for novel drug development.
|
Novel drug delivery system
|
. Scope of The Present Work: –
- Background: The article should ideally start by describing Alzheimer's Disease as a neurodegenerative disorder characterized by progressive cognitive decline, memory loss, and behavioral changes. The paper might review current statistics on AD's prevalence globally, identifying its status as a growing concern due to an aging population.
- Research Context: The article may also highlight the challenges faced by healthcare systems and researchers in diagnosing, treating, and managing AD, especially due to its complex pathology.
- Genetic and Molecular Insights: A recent focus of AD research is on genetic factors, like mutations in the APP, PSEN1, and PSEN2 genes, and their contribution to the disease. The review may mention how scientists are mapping the genetic basis of AD.
- Amyloid Plaques and Tau Tangles: One prominent area of research is the role of amyloid-beta plaques and tau protein tangles in the brain. The article may explain the significance of these structures in disease progression and how they are being targeted for treatment.
- Neuroinflammation: The paper may address the emerging role of inflammation in AD, highlighting studies on microglia (the brain's immune cells) and the potential for anti-inflammatory treatments.
Synaptic and Neurovascular Changes: The paper might describe how disruptions in neuronal connectivity and the blood-brain barrier contribute to cognitive deficits in AD.
Methodology: –
One of the main causes of dependency, disability, and death is acquired progressive cognitive impairment that is severe enough to affect day-to-day activities. According to current estimates, 44 million individuals worldwide suffer with dementia. As the population ages, this is expected to more than treble by 2050, when the yearly cost of dementia in the United States alone might surpass US$600 billion.5 Dementia accounted for 11.6% of all recorded deaths in 2015, making it the leading cause of mortality in England and Wales6.
Clinical signs and symptoms
The clinical spectrum of Alzheimer’s disease is demonstrated by three instances in panel 1 (also see figure 1). As demonstrated by the current worldwide efforts of the Dominantly Inherited Alzheimer Network and Alzheimer Prevention Initiative, as well as the related clinical studies, Case A focus on genetically determined Alzheimer’s disease. The difficulty in identifying Alzheimer’s disease in people whose memory issues are not the primary symptom is demonstrated by Case B, which is an example of a linguistic variation of the disease that typically manifests at a younger age (less than 70 years). Case C, a typical amnestic variety that is more frequently observed in patients over 70, exemplifies the growing number of people afflicted by dementia and Alzheimer’s disease: elderly people who are more reliant on others for care and frequently live alone.

Fig.1 Imaging findings of a case similar to patient B’s case in panel 1
Pathogenesis: –
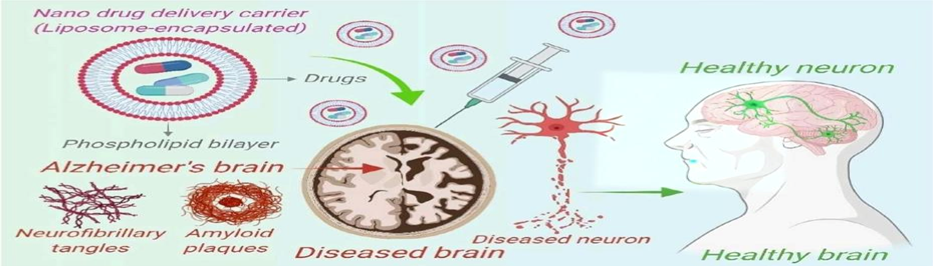
Senile or neuritic plaques and neurofibrillary tangles (figure 2) in the brain’s cortical regions and medial temporal lobe structures, along with a loss of neurones and synapses, are the hallmark microscopic lesions of Alzheimer’s disease. Numerous pathogenic mechanisms have been investigated to explain these alterations, including aberrant cell cycles, inflammatory processes, oxidative stress, mitochondrial dysfunction, tau hyperphosphorylation with tangle formation, A? aggregation and deposition with plaque development, and neurovascular dysfunction. According to the amyloid hypothesis, the most widely accepted theory of AD pathogenesis, the main pathological process is the accumulation of pathological forms of Ab caused by the brain's b- and c-secretase enzymes sequentially cleaving the APP. This imbalance between Ab production and Ab clearance is thought to be the cause of this accumulation. It is believed that the development of NFTs and the ensuing neuronal dysfunction and neurodegeneration—possibly caused by inflammation—are downstream processes.7

(Fig.2 Plaques and tangles in the cerebral cortex in Alzheimer’s disease).

fig.3 An overview of the major pathogenic events leading to Alzheimer’s disease as proposed by the amyloid hypothesis
Panel: Research diagnostic criteria for Alzheimer’s disease Probable Alzheimer’s disease
Core diagnostic criteria
A] The following characteristics of an early and severe episodic memory impairment are present:
1. Patients or informants describe a gradual and progressive decline in memory function over a period of more than six months.8
2. Test-based objective evidence of markedly impaired episodic memory: this often consists of a recall deficit that does not improve noticeably or normalise with cueing or recognition tests, even after successful information encoding has been managed.9
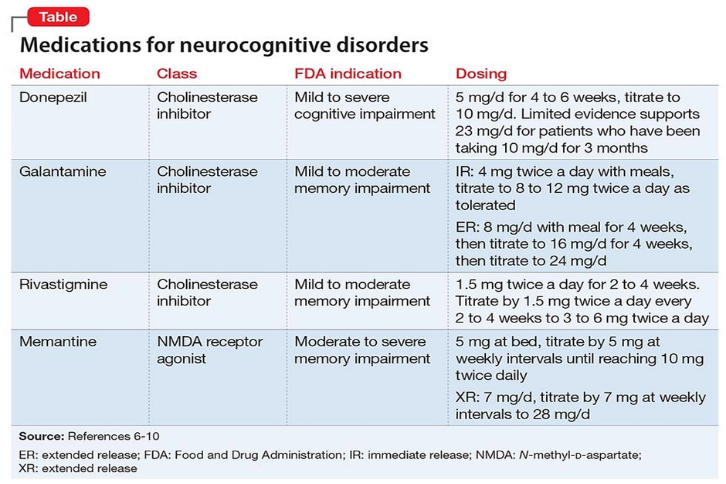
Treatment: –
As soon as Alzheimer’s is diagnosed, patients and their families should be involved in order to treat the condition effectively. In addition to providing information, services, and support to assist patients and their families live effectively with dementia, it is important to evaluate patients’ abilities to manage money, drugs, transportation, and household appliances.10 along with instances of new pharmaceutical and immunotherapy treatments. Since the middle of the 1990s, there have been numerous options for treating Alzheimer’s symptoms.11

fig.4 Progressive atrophy in presymptomatic Alzheimer’s disease
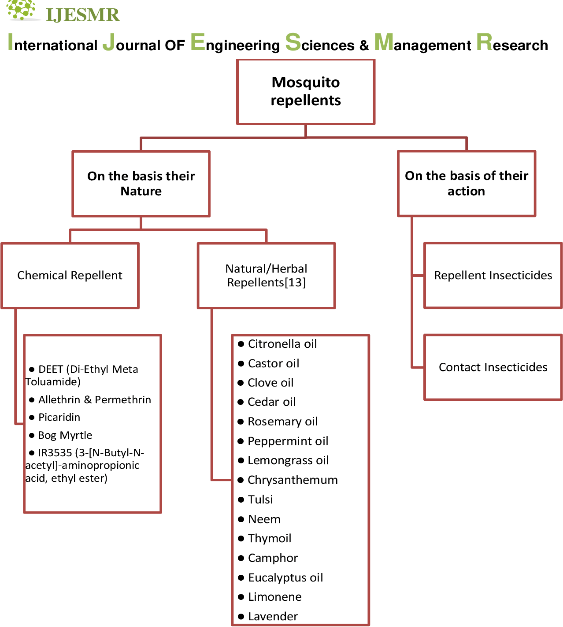
• Nanomaterials for the Treatment of Neurodegenerative Diseases
AD, or Alzheimer’s disease Alzheimer’s disease (AD), one of the most common neurodegenerative diseases in the elderly population, is responsible for more than 80% of dementia cases worldwide. It causes a progressive decline in mental, behavioural, and functional abilities as well as a loss of learning capacity.12 Lipoic acid, which is naturally present in the mitochondria and has potent anti-inflammatory and antioxidant qualities that can reduce oxidative stress, is one example of how NPS may improve the efficacy of AD therapy.13 They are safe, biodegradable, and customised to meet a particular goal thanks to their design.14
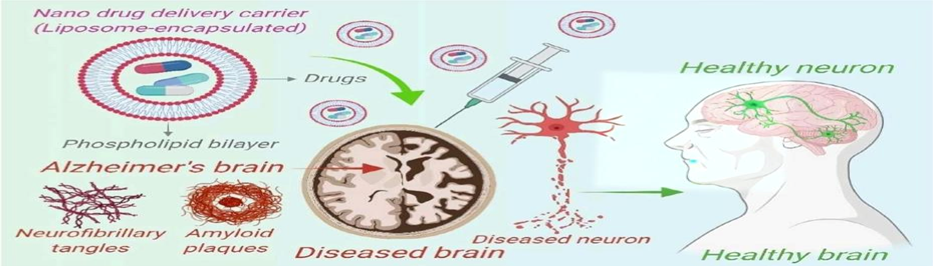
Fig.5 Nano drug delivery for the treatment of Alzheimer’s disease.
Drugs used in treatment of Alzheimer’s disease
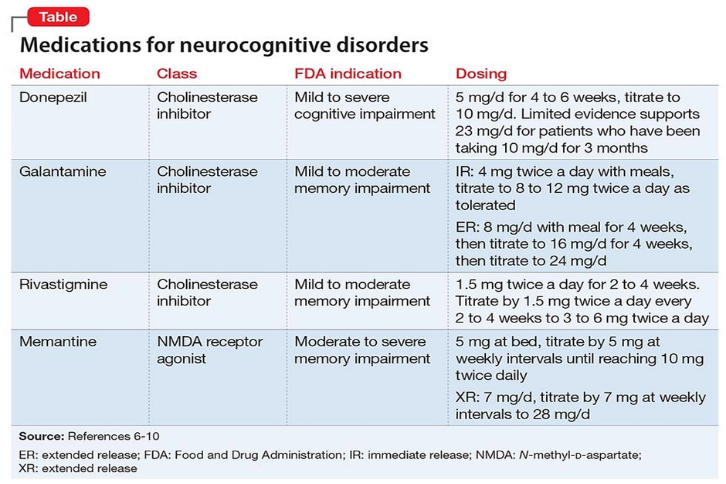
Donepezil
Class: Reversible acetylcholinesterase (AChE) inhibitor.
Mechanism: Donepezil selectively inhibits acetylcholinesterase, the enzyme responsible for breaking down acetylcholine in the synaptic cleft.
This inhibition increases acetylcholine levels in the synaptic cleft.
- Galantamine
Class: Dual-action agent (acetylcholinesterase inhibitor and allosteric modulator of nicotinic receptors).
Mechanism:
- Acetylcholinesterase inhibition: Similar to donepezil, galantamine inhibits acetylcholinesterase, increasing acetylcholine levels in the synaptic cleft.
3. Rivastigmine
Mechanism
Rivastigmine is a dual cholinesterase inhibitor that blocks both acetylcholinesterase (AChE) and butyrylcholinesterase (BuChE). This increases acetylcholine levels in the brain, improving cholinergic neurotransmission.
Drug candidates based on epidemiology: –
Epidemiology-based drug candidates Numerous therapeutic philosophies have been theoretically grounded in epidemiological research. As discussed below, observational studies have indicated that various drugs or supplements may have a protective effect. However, beneficial effects have proven difficult to determine when tested in randomised controlled clinical trials, which are intended to circumvent the numerous potential biases and inherent methodological issues in epidemiological studies.15 Medicines that reduce cholesterol In a study that found intracellular A? accumulation in rabbits on a very high-cholesterol diet, the first connection between cholesterol and Alzheimer's disease was proposed.16 However, there have been reports of both decreased.17 and increased brain A? burden in Alzheimer's disease transgenic mice fed a high-cholesterol diet. Hormones Postmenopausal oestrogen supplementation has been linked in epidemiological studies to a lower incidence of dementia.18,19 Oestrogens may potentially have a number of positive effects on brain function, according to research on animals.20 The sickness is caused by antioxidants.21,22 Numerous observational studies indicate that antioxidants like vitamin E may lower the risk of Only a slight impact on the time to institutionalisation and requirement for care was seen in one randomised controlled clinical trial of vitamin E supplementation in the illness
Future prospects: –
Despite a significant rise in recent years, our understanding of AD is still far from comprehensive. Numerous mechanisms crucial to the pathophysiology of AD have been revealed by next-generation genomic research; these are presently being investigated in cellular and animal models and are already producing new therapeutic targets. A more sophisticated approach to treatment and prevention will also result from a more nuanced concept of the preclinical phase of AD, which views inflammation, tau, and b-amyloid as components of a cellular phase of AD pathogenesis rather than as steps along a sequential pathway.23
Disease characteristics
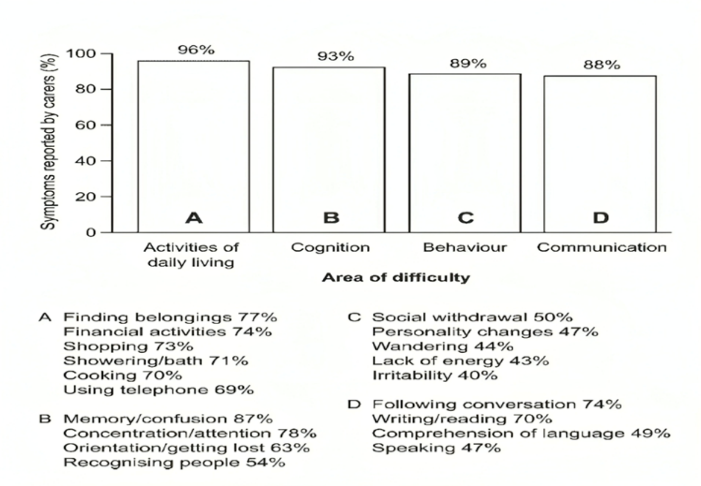
81% of respondents stated that memory loss or confusion was the most common symptom that first led the patient or carer to seek assistance. Dementia was typically diagnosed in a hospital (31%), or in a general practitioner’s office (GP/primary care) (31%). In Scotland, a psychiatrist made the diagnosis most frequently (Scottish patients, 34%; all patients, 17%), but a neurologist made the diagnosis most frequently (43%). Seventy-four percent of the dementia patients surveyed had been diagnosed with AD, while another eleven percent had vascular dementia. At the time of the survey, the majority of patients (67%) had had a dementia diagnosis for at least two years. At this point, 8% of people still had mild dementia, while more than half had moderate/middle-stage dementia (38%) or severe/late-stage dementia (26%). Eighty-seven percent of patients were older than sixty-six, and 19 percent were older than eighty-five. Although the number of patients who had received information regarding their disease varied by country, two-thirds (64%) of patients in Scotland were aware that they had dementia, whereas just 23% of patients in Spain had received this information.24.
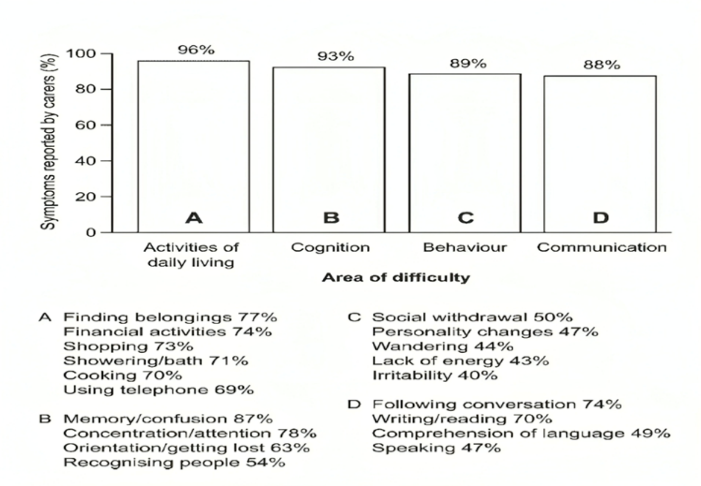
fig.no 6. Overview of current symptoms
As common as cognitive symptoms (93%) were behavioural issues and difficulties with activities of daily living (ADLs), which were reported by 89% and 96% of carers, respectively (Figure 6). The most prevalent behavioural issues were irritability (affecting 40% of patients), personality alterations (affecting 47%), and social disengagement (affecting 50% of dementia patients).
Impact of behavioural and functional problems
The fact that 32% of those surveyed reported spending at least 14 hours a day caring for the person with dementia highlights the strain that AD places on carers. An additional 12% of carers devoted 10–14 hours a day to providing care. The more severe the ailment, the more time is spent caring. Overall, over 40% of carers for patients with mild dementia and 50% of carers for those with severe dementia reported spending more than 10 hours a day on patient care (Figure 3). Nevertheless, 20% of carers for patients with moderate dementia reported spending more than ten hours a day managing the patient’s requirements (Figure 7).25
Fig-7 Time spent caring for person with dementia, according to current disease severity.
CONCLUSION: –
The conclusion of a review article on Alzheimer's disease typically summarizes the current state of knowledge, highlights gaps, and outlines potential future directions for research and treatment. Here’s an outline of key points that could form the conclusion of such a review:
Current Understanding: Alzheimer's disease (AD) is a complex neurodegenerative disorder characterized by the accumulation of amyloid plaques and tau tangles, leading to progressive cognitive decline and memory loss. While these hallmark features have been well documented, the exact cause of AD remains unclear, with genetic, environmental, and lifestyle factors likely playing significant roles.
Diagnostic Advances: Advances in diagnostic techniques, including neuroimaging and biomarkers, have made it possible to detect Alzheimer's at earlier stages, even before symptoms appear. However, challenges remain in terms of the accuracy and accessibility of these diagnostic tools, and there is a need for improved screening methods for early-stage identification.
Treatment Landscape: Currently, there are limited pharmacological treatments for Alzheimer's disease. Most treatments focus on symptomatic relief by modulating neurotransmitters like acetylcholine, but they do not stop or reverse disease progression. Recent approvals of drugs targeting amyloid plaques offer hope, but their effectiveness remains debated, and further studies are needed to assess their long-term benefits and safety.
REFERENCES
- Alzheimer Europe. Dementia in Europe Yearbook 2019: estimating the prevalence of dementia in Europe. 2020. https://www.alzheimereurope.org/content/download/195515/1457520/file/FINAL 05707 Alzheimer Europe yearbook 2019.pdf (accessed Jan 24, 2021).
- Scheltens P, Blennow K, Breteler MM, et al. Alzheimer’s disease. Lancet 2016; 388: 505–17.
- Dubois B, Feldman HH, Jacova C, et al. Research criteria for the diagnosis of Alzheimer’s disease: revising the NINCDS-ADRDA criteria. Lancet Neurol 2007; 6: 734–46.
- Ferri CP, Prince M, Brayne C, et al. Global prevalence of dementia: a Delphi consensus study. Lancet 2005; 366: 2112–17.
- Mayeux R. Epidemiology of neurodegeneration. Annu Rev Neurosci 2003; 26: 81–104.
- Mortimer JA, Snowdon DA, Markesbery WR. Head circumference, education and risk of dementia: fi ndings from the Nun Study. J Clin Exp Neuropsychol 2003; 25: 671–79.
- Masters CL, Simms G, Weinman NA, Multhaup G, McDonald BL, Beyreuther K. Amyloid plaque core protein in Alzheimer disease and Down syndrome. Proc Natl Acad Sci USA 1985; 82: 4245–49.
- Kang J, Lemaire HG, Unterbeck A, et al. The precursor of Alzheimer’s disease amyloid A4 protein resembles a cell-surface receptor. Nature 1987; 325: 733–36.
- Geddes JW, Tekirian TL, Soultanian NS, Ashford JW, Davis DG, Markesbery WR. Comparison of neuropathologic criteria for the diagnosis of Alzheimer’s disease. Neurobiol Aging 1997; 18: S99–S105.
- Hardy J, Myers A, Wavrant-De Vrieze F. Problems and solutions in the genetic analysis of late-onset Alzheimer’s disease. Neurodegener Dis 2004; 1: 213–17.
- Ertekin-Taner N. Genetics of Alzheimer disease in the pre- and post-GWAS era. Alzheimers Res Ther 2010; 2: 3.
- Kumar,A.; Singh, A. A review on Alzheimer’s disease pathophysiology and its management: An update. Pharmacol. Rep. 2015, 67, 195–203. [CrossRef]
- Furtado, D.; Björnmalm, M.; Ayton, S.; Bush, A.I.; Kempe, K.; Caruso, F. Overcoming the blood–brain barrier: The role of nanomaterials in treating neurological diseases. Adv. Mater. 2018, 30, 1801362. [CrossRef] [PubMed]
- Li, A.; Tyson, J.; Patel, S.; Patel, M.; Katakam, S.; Mao, X.; He, W. Emerging Nanotechnology for Treatment of Alzheimer’s and Parkinson’s Disease. Front. Bioeng. Biotechnol. 2021, 9, 672594. [CrossRef] [PubMed]
- Simons M, Schwarzler F, Lutjohann D, et al. Treatment with simvastatin in normocholesterolemic patients with Alzheimer’s disease: a 26-week randomized, placebo-controlled, double-blind trial. Ann Neurol 2002; 52: 346–50.
- Höglund K, Thelen KM, Syversen S, et al. The eff ect of simvastatin treatment on the amyloid precursor protein and brain cholesterol metabolism in patients with Alzheimer’s disease. Dement Geriatr Cogn Disord 2005; 19: 256–65.
- Sparks DL, Sabbagh MN, Connor DJ, et al. Atorvastatin for the treatment of mild to moderate Alzheimer disease: preliminary results. Arch Neurol 2005; 62: 753–57.
- Henderson VW, Paganini-Hill A, Emanuel CK, Dunn ME, Buckwalter JG. Estrogen replacement therapy in older women: comparisons between Alzheimer’s disease cases and nondemented control subjects. Arch Neurol 1994; 51: 896–900.
- Tang MX, Jacobs D, Stern Y, et al. Eff ect of oestrogen during menopause on risk and age at onset of Alzheimer’s disease. Lancet 1996; 348: 429–32. 141 Almeida OP, Flicker L. Association between hormone replacement therapy and dementia: is it time to forget? Int Psychogeriatr 2005; 17: 155–64.
- Mulnard RA, Cotman CW, Kawas C, et al. Estrogen replacement therapy for treatment of mild to moderate Alzheimer disease: a randomized controlled trial. Alzheimer’s Disease Cooperative Study. JAMA 2000; 283: 1007–15.
- Shumaker SA, Legault C, Kuller L, et al. Conjugated equine estrogens and incidence of probable dementia and mild cognitive impairment in postmenopausal women: Women’s Health Initiative Memory Study. JAMA 2004; 291: 2947–58.
- Engelhart MJ, Geerlings MI, Ruitenberg A, et al. Dietary intake of antioxidants and risk of Alzheimer disease. JAMA 2002; 287: 3223–29.
- Morris MC, Evans DA, Bienias JL, et al. Dietary intake of antioxidant nutrients and the risk of incident Alzheimer disease in a biracial community study. JAMA 2002; 287: 3230–3
- Wu G, Lanctot KL, Herrmann N, et al. 2003. The cost-benefit of cholinesterase inhibitors in mild to moderate dementia: a willingness-to-pay approach. CNS Drugs 17(14): 1045–1057.
- Waldemar G, Phung KTT, Burns A, etal. 2007. Accesstodiagnostic evaluation and treatment for dementia in Europe. Int J Geriatr Psychiatry 22: 47–54


 Siddhant Sawatkar*
Siddhant Sawatkar*
 Shivanee Tupkar
Shivanee Tupkar
 Dr. Gajanan Sanap
Dr. Gajanan Sanap




 10.5281/zenodo.14544288
10.5281/zenodo.14544288