Abstract
In recent years, there has been an increasing number of research on the sustained and controlled distribution of drugs through the use of natural and biocompatible ingredients. In this day and age, herbal medications made from natural or traditional herbs provide merit as alternative treatments for the majority of infectious diseases as well as non-communicable illnesses like diabetes and cancer. medication delivery problems have been solved by nanotechnology, a revolutionary approach that improves medication absorption, sustains drug release, controls drug release, lowers drug toxicity, etc. A hydrogel nanoparticle containing a network of cross-linked hydrophilic polymers is referred to as a "nanogel." Cross-linked polymer nanoparticles, or nanogels, swell in an appropriate solvent. As they are smaller in size, nanogels exhibit better penetration characteristics and a strong drug loading capacity. There are several ways to deliver them, including oral, nasal, parenteral, pulmonary, intra-ocular, etc. Nanogel is preferred for herbal remedies since it is comfortable and stable. This review article focuses on the reported activities of herbal nanogels, synthesis, its preparation, characterization and evaluation. Its degradability and biocompatibility create a multibillion dollar market for the expanding pharmaceutical sector. Herbal nanogels so increase its efficacy and serve a multipurpose purpose.
Keywords
Herbal, Sustained release, Routes, Characterization
Introduction
"The therapeutic practices that are alive for many years, before the event and spread of recent medicines" is a common definition of herbal medicine. This area of medicine, which is primarily the subject of research by numerous researchers, uses medicinal plants for therapeutic purposes and is used as herbal medicine.[1] In this day and age, herbal remedies made from natural or traditional herbs make sense as alternative treatments for the majority of infectious diseases as well as non-communicable illnesses like diabetes and cancer[2]. Herbal remedies have been helpful in providing the pharmaceutical industry's modern pharmacopoeia with much-needed inspiration. Modern medications can have more adverse effects than herbal remedies, which makes herbal remedies a healthier choice for patients. Approximately 85% of people worldwide cure skin conditions such as fungal, viral, or diabetic linked conditions, as well as hypersensitive reactions, with herbal medications. However, in fact, they are seldom employed in medicine despite having acceptable pharmacological action for a variety of reasons, including high dose requirements, problems with solubility, and problems with bioavailability[3] . By utilizing them in a novel manner, they might be included into routine medical procedures. This leads to a decrease in the dosage of the herb employed as a drug for pharmacological activity; yet, the affordability and ease of use of these ancient medicines make them more appealing as a substitute for conventional treatments [4]. Nanotechnology is a cutting-edge method with a wide range of applications in drug delivery. The development of innovative drug delivery systems affects the diagnosis, treatment, and prevention of disease. This innovative approach to problem-solving involves enhancing drug absorption, releasing pharmaceuticals over time, controlling drug release, lowering drug toxicity, etc. The development of nanoparticles, which function as carriers and can be loaded with medications or genetic material that releases in a controlled or sustainable manner to a specified target spot, is one way that nanotechnology is being applied to medicine. Nowadays, there are many different nanotechnological methods for delivering drugs, such as nanogels, nano-emulsions, nanosuspensions, and nanotubes. However, because nanogels have advantages over other formulations, they are more commonly found in the market.
"Nanogel" is the name given to a hydrogel-containing nanoparticle with a cross-linked polymer network. A nanogel is a cross-linked, nanoscale hydrogel composed of small, swelling particles and amphophilic or hydrophilic polymer networks, which may or may not be anionic. They serve as drug molecule carriers and are engineered to absorb active substances through the creation of biomolecular interactions such as salt and hydrogen bonds, among others[2]. By permitting the interaction between the matrix and the active agent, the primary biological component can be loaded into nanogels, leading to more widely distributed hydrophilic particles. Because of this, nanogels emerge as a more adaptable structure for regulated and continuous drug release at the intended location.
Advantages Of Nanogels:[5]
- A smaller amount of medicine is needed.
- Offer defense against the drug molecule's internal biodegradation within the body system.
- The nanogel's size can be changed based on the delivery molecule.
- Increase the drug molecule's bioavailability
- Lessens the toxicity of drugs.
- Nanogels can pass through both the blood-brain barrier and the skin's physiological barrier.
- Drug-loaded nanogels can be applied topically and absorbed into the body without causing any negative side effects.
Disadvantages Of Nanogels:[5]
- Surfactant particles can at times be adverse.
- Expensive procedures are needed.
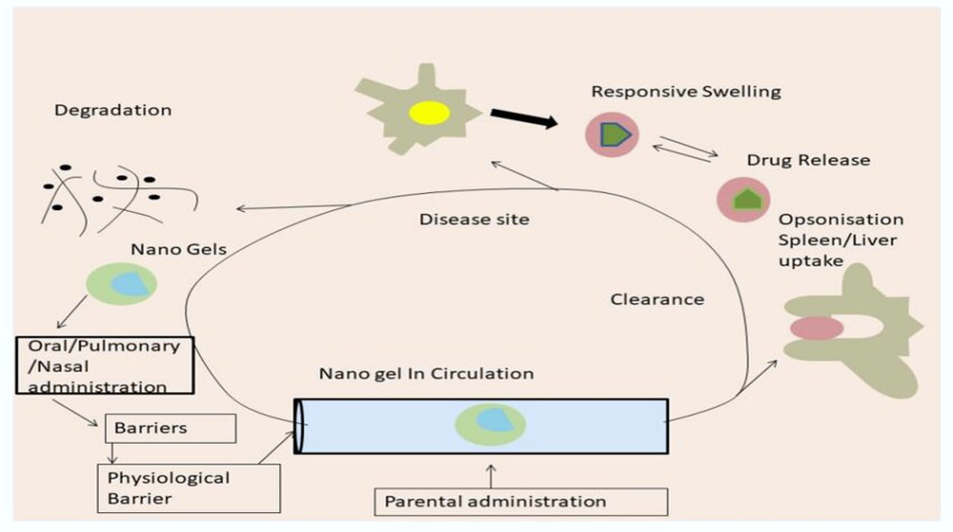
Routes Of Administration Of Nanogel:
- Topical
- Nasal
- Pulmonary
- Parenteral
- Intraocular
- Oral However, for the administration of herbal nanogel, oral and transdermal route is the most preferred one.
NANOFORMULATIONS OF HERBAL MEDICINES
Pharmaceutical companies find it difficult to develop a complete herbal medication since a variety of elements affect the plant herb's biological efficacy and repeatability of its therapeutic potential. Certain illnesses, including asthma, pain, fever, etc., require medications to have a quick start of action; conversely, chronic treatments like diabetes, cancer, and hypertension, among others, may also require longer acting times. However, because of their physiochemical characteristics, herbal treatments are severely limited in both phases. These elements have undoubtedly reduced their influence on contemporary medicine [6]. To provide herbal medicines with successful results, significant research investments have been undertaken in recent years. However, a nanotechnology approach is used to control the system's active phytoconstituents' activity in order to achieve the desired efficacy of herbal medications [7, 8]. By enhancing the potential of drug action, encouraging the prolonged release of active ingredients, lowering the necessary dosage, and enhancing biological activity, nanotechnology has demonstrated to raise the likelihood of implementing herbal-based pharmaceuticals [8,9]. To protect herbal medications from external sources of degradation and boost their bioavailability, many nanomaterials have been tested as carrier vehicles, including polymeric nanoparticles, solid lipid nanoparticles (SLN), lipid crystal (LC) systems, liposomes, and nano-emulsions [10,11]. Numerous studies show that a nano-delivery method can assist in optimizing the physiochemical properties of herbal medications in accordance with the needs. Kesarwani and Gupta stated that the characteristics of herbal compounds have been enhanced by nano-formulations [12], while Ghosh created a lipid-based approach to boost the bioavailability of active compounds derived from ginseng and green tea [13]. Significantly, the bioavailability of the active ingredients in the extract of Radix Salvia Miltiorrhiza Bunge (Lamiaceae) had improved [14].
SYNTHESIS OF NANOGELS:
Depending on the size, polymerization technique, and nano-meter scale, there are many categories for the procedures used to create nanogels. This section goes into detail on how to prepare gels and regulate their nanostructures [15].
Physical Techniques
Some popular physical methods for creating nanogels are inverse nanoprecipitation, microfluidics, and the mini-emulsion technique. The mini-emulsion process produces a water-in-oil emulsion by incorporating small particles of oil-soluble surfactants into a continuous organic phase. In the microfluidic technique, glass chambers or a capillary tube made of silica that resembles polymers are utilized to produce droplets. The most methodical approach to creating aqueous nanogels is by the final system, known as inverse nanoprecipitation, which is just mixing an aqueous polymeric solution with a miscible non-solvent [16] .
Crosslinking Method
One of the best coupling techniques for creating a gel network using monomers that have a reactive functional group at a lower molecular weight is covalent crosslinking. The highly stable nanogels produced by covalent bonding by the crosslinking of their functional groups were beneficial in the drug release and trapping process when produced in vitro. Chemical reactions including Schiff base reaction, free radical polymerization, and other photoreactions may be used in this crosslinking [17]. Through the crosslinking of preformed polymers, nanogels are created in heterogeneous colloidal environments, such as w/o microemulsions [18]. This method makes it simple to include biomacromolecules and small-molecule medications into nanogels. The amount of polymer required to obtain the necessary size depends on a number of variables, including temperature, ionization constant, pH value, and ionic strength.
This method's ability to make disc- or ellipsoid-shaped nanoparticles instead of spherical ones, which prevents phagocytosis, is one of its main advantages. Thanks to recent research and produced goods, the crosslinking procedure is combined with the microfluidic emulsification approach to produce a homogenous dispersion of nanoparticles. Given that, as figure 1 illustrates, bioavailability is closely correlated with particle size, particle size is an important factor to take into account when administering drugs.
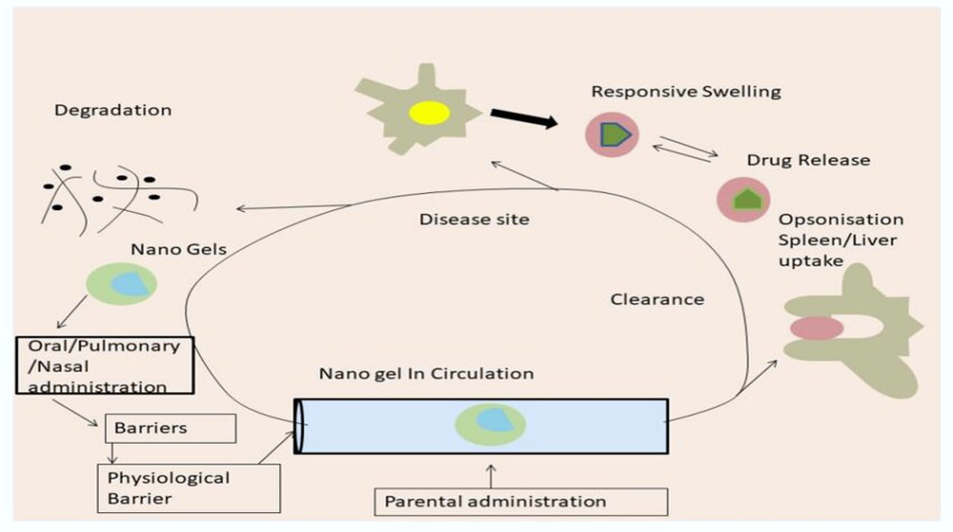
Figure 1. Mechanism of action of covalent crosslinking
Noncovalent Binding
Physical crosslinking nanogels, such as weak van der Waal forces, hydrophilic and hydrophobic contacts, and so forth, are created via non-covalent binding. These forms are less stable, and the temperature, crosslinking agent, and composition all have a significant impact on how reactive the gel is. It has been demonstrated that the use of nanogels, which produce micelles, can up to 30,000 times increase the solubility of extremely lipophilic medications [19]. For instance, polyhydroxy butyrate and polypropylene oxide are frequently used in the creation of biodegradable polymer micelles [20].
Bioconjugation Technique
One well-known and well-managed technology for creating nanogels in a variety of sizes and shapes—including core-shell nanogels—is the free radical polymerization process. Sub initiators, such as functional initiatives and micro initiators, are employed in this bioconjugation procedure to prevent functionalities from being present inside the nanogels, thereby permitting multivalent bioconjugation. Because of brittle connections between polymer chains, such as hydrogen bonding, hydrophobic contacts, or non-covalent interactions, physically crosslinked systems under moderate circumstances are more likely to be brittle than their covalently crosslinked counterparts [21].
PREPARATION OF NANOGELS
The physicochemical properties of the polymer and drug to be loaded determine which preparation process is best. The following techniques are used in the preparation of nanogels:
Emulsion-Solvent Diffusion Method [22]
The following steps are involved in the formation of nanogel using the Emulsion- Diffusion method:
-
-
- The drug's precisely weighed quantity was continuously stirred as it was dissolved in water-misciblesolvent(organicphase).
- The drug phase was sonicated for 10 minutes using an ultrabath sonicator after the aqueous phase was prepared by dissolving the polymer and gelling agent in water while stirring and heating continuously.
- To create an emulsion, the drug phase was gradually introduced drop by drop to the aqueous during high-speed homogenization for 30 minutes at 6000 rpm. O/W emulsion formed when a homogenizer transformed the emulsion into a nanodroplet.
- To create nanogel, the generated O/W emulsion was homogenized for an hour at 8000 rpm and triethanolamine was added while being constantly stirred.
Nano Precipitation Method [23]
-
-
- The polymer precipitates as a result of mixing the aqueous phase, which contains water and surfactant, with the organic phase, which contains the drug and polymer dissolved in organic solvents. Solvent evaporation was followed by the formation of polymeric nanoparticles.
- The dispersion method was employed to formulate the gel. spreading the gelling chemical over two hours to promote swelling. After the particles had inflated, the gelling agent was added with the recommended amount of nanoparticle dispersion and stirred.
- Triethanolamine was added in order to preserve the pH.
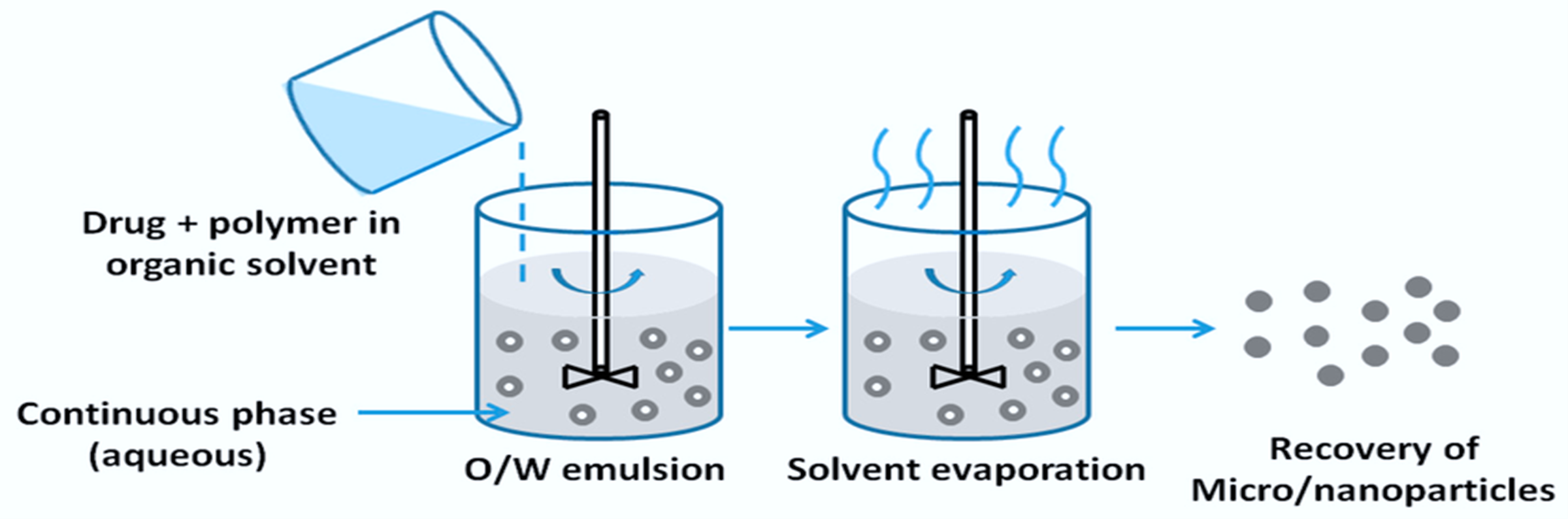
Emulsion-solvent evaporation method [24]
-
-
- Using a magnetic stirrer, the dispersion phase containing the drug and polymer in a water-impermeable solvent was gradually applied to a specific area of the aqueous phase at a speed of 1000 rpm for two hours.
- After filtering and drying the generated nano-sponges for 24 hours at 40°C in a hot air oven, they were placed into vials. In order to get a smooth dispersion, the polymer must first be soaked in water for two hours in order to facilitate the gel formation. A pH adjuster was then added to balance the pH. Agitation should be done at 6000 rpm using a magnetic stirrer. Aqueous dispersion was supplemented with the previously prepared optimized nano-sponge suspension and permeation enhancers.
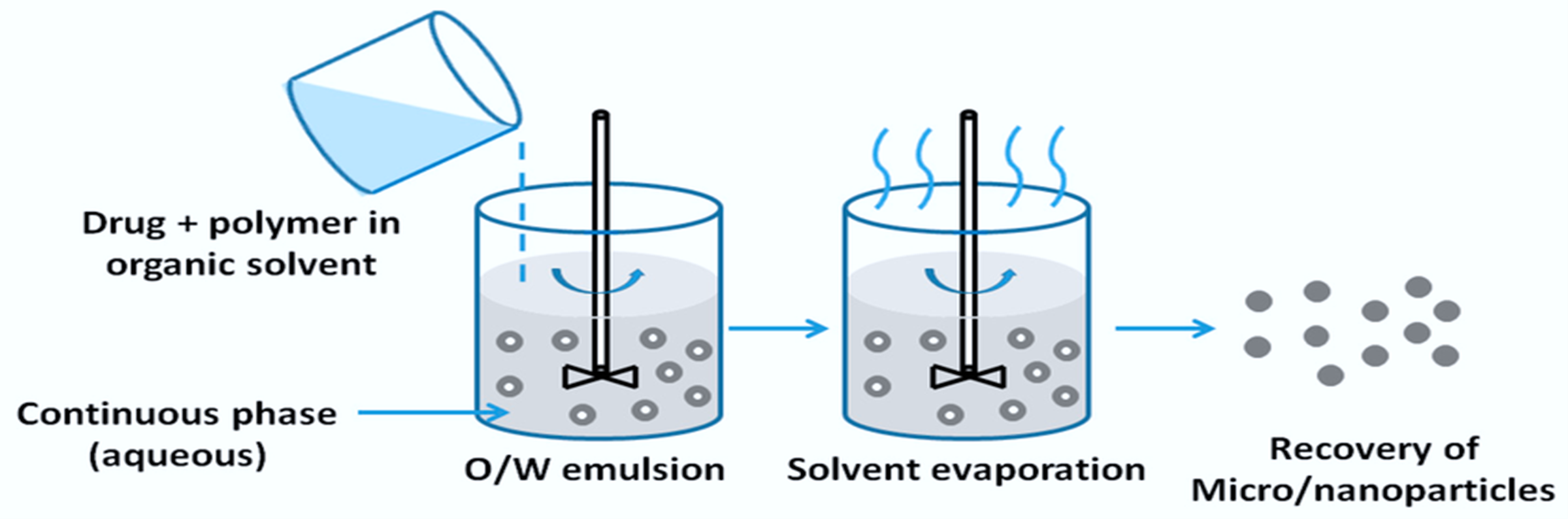
Figure 2. Emulsion Solvent Evaporation Method
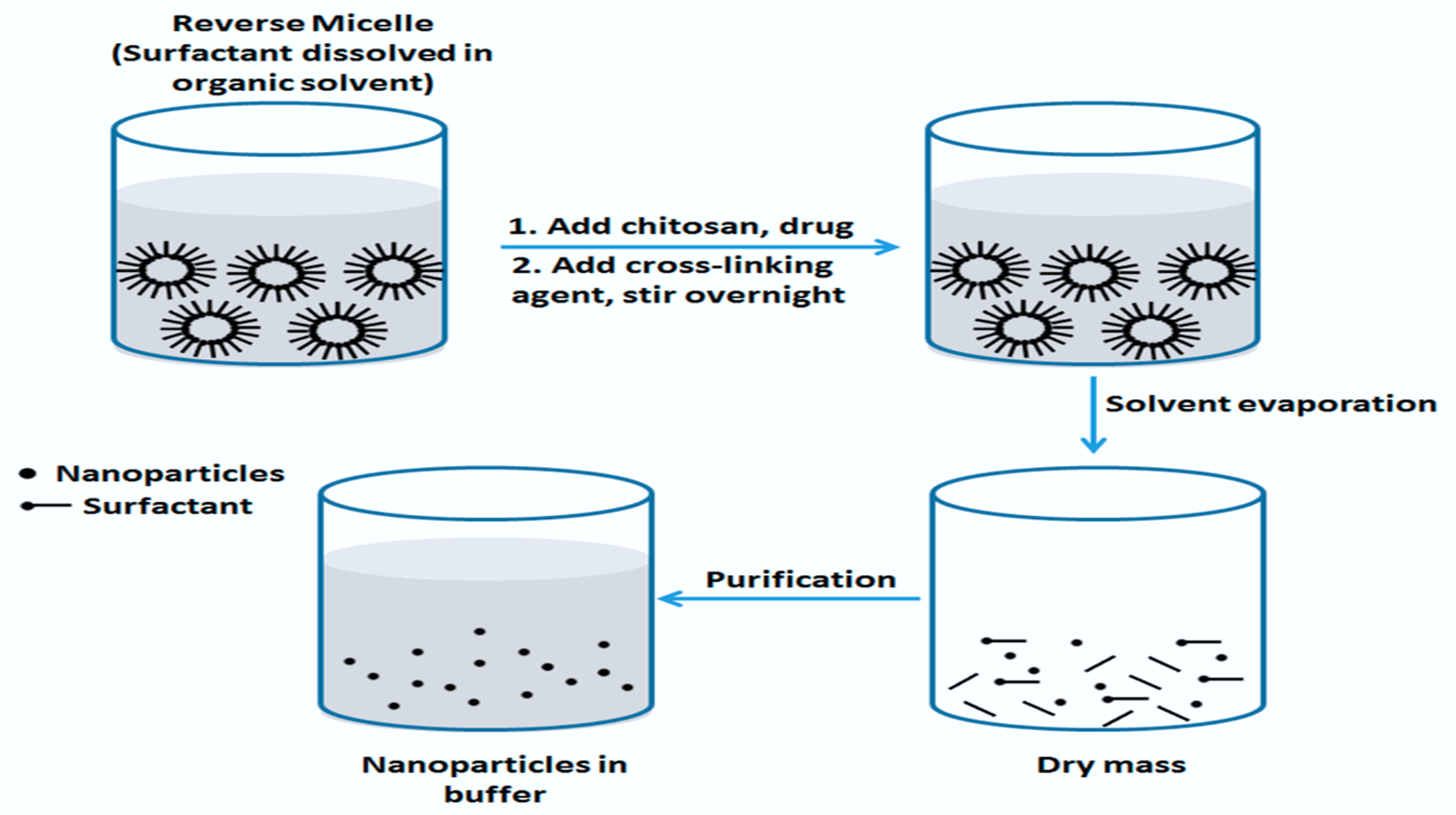
Reverse micellar method [25]
An organic solvent was used to dissolve the medication and polymer that were added to the surfactant. After adding the crosslinking agent, stir overnight.
-
-
- After the buffer's nanoparticles have been purified, the solvent evaporates and leaves behind bulk.
- Water was used to dissolve the gelling agent. To create nanogel, the produced nanoparticles were combined with an aqueous phase containing a gelling agent; a pH adjuster was then added to balance the pH.
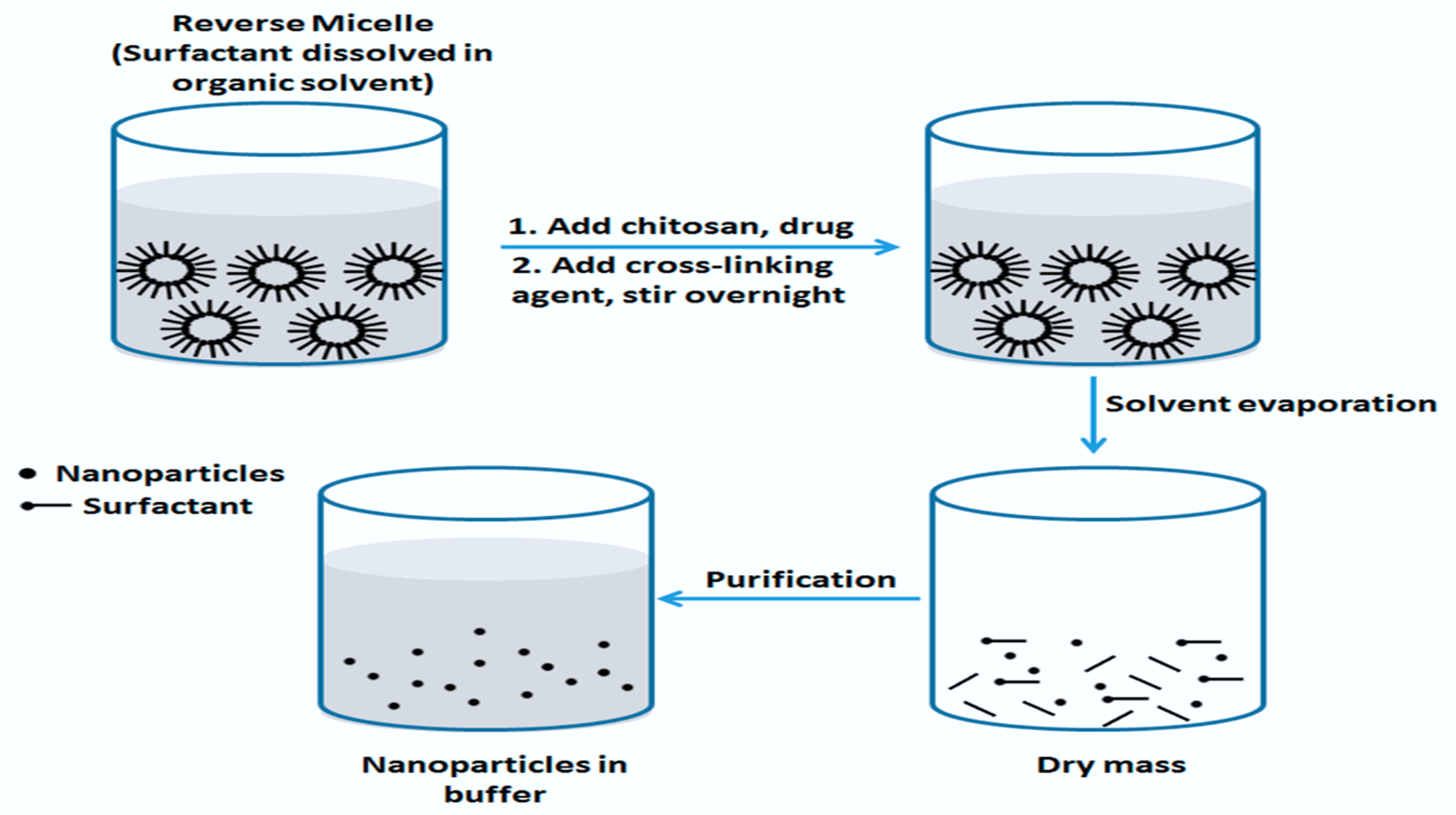
Figure 3. Reverse Micellar method
Modified emulsification - diffusion method [26]
-
-
- A certain quantity of the drug was weighed and combined with a polymer that contained solvent. The drug-polymer combination is added to the aqueous phase and continuously stirred at a speed of 5000–10,000 rpm to form the organic phase. Using a syringe fitted with a needle, the organic phase was gradually introduced drop by drop at a rate of 0.5 ml/min into an aqueous stabiliser solution.
- After 6 minutes of agitation at 10,000–25,000 rpm, the resultant dispersion was sonicated for 5–minutes.
- To encourage the diffusion of the organic solvent into a continuous phase, double-filtered water was then progressively added to the dispersion while being stirred continuously for an hour.
CHARACTERIZATION AND EVALUATION OF NANOGELS
Before using nanogels, they should be thoroughly characterized. The techniques described below are usually thought to be appropriate for the purpose.
Infrared spectroscopy
An FT-IR spectrophotometer was used to collect the infrared (IR) spectra of Nanogel between 4000-400 cm-1.5.1.
Dynamic Light Scattering
To determine the features of nanoparticle size distribution in liquids, dynamic light scattering (DLS) is employed. Light scattering is recorded on a microsecond time frame throughout different research. The impact of the cross-linker and the charges of the polymer chains on the size of the resulting nanogel can be measured using an effective hydrodynamic particle radius. Nanogel swelling in different media can also be measured using DLS. It is important to remember that the population of smaller polymer particles might not be taken into consideration by the DLS data [27]. Often, a combination of analytical approaches is needed to completely understand an object's attributes. The polydispersity index and the average particle diameter were also examined using DLS.
Scanning Electron Microscopy
One way to ascertain the size and shape of the particle surface is using electron microscopy. It can also be used to evaluate the morphological properties of nanogels and quantify particles with sizes between 50 and 80 nm. The surface morphology of the nanogel formulation was evaluated using scanning electron microscopy at X30, X500, X1000, and X3000 magnifications using a 20kV electron beam. A droplet of nanoparticulate dispersion was deposited on an aluminium metal plate and dried under vacuum to form a dry film, which allowed samples to be examined using a scanning electron microscope.
Size-Exclusion Chromatography
For the past 50 years, SEC has been recognized as the gold standard for figuring out the distributions and molar mass averages of both natural and synthetic macromolecules [28]. SEC, when combined with different kinds of detection techniques, can provide us with more insight into the physicochemical characteristics of polymers [29].
The nanogels were evaluated related on their properties:[30]
-
- Appearance
Visual inspection was done to check the clarity, color, and appearance of any particles in the nanogel bases.
-
- Homogeneity
Through visual evaluation of the nanogel formulation, the homogeneity was verified. Their appearance and the presence of any aggregates were examined.
-
- Measurement of particle size, polydisperse index, particle distribution
Using the Zeta sizer and Malvern MasterSizer 2000 MS, the mean size of the nanogels was determined, and the results were noted.
-
- Determination of pH
With the help of the Electrolab digital pH meter, the pH of the nanogel formulation was determined. A little amount of the formulation was transferred to a beaker containing a particular amount of distilled water. After dipping the electrode into the mixture, the nanogel's pH was measured.
-
- Drug content
High-performance liquid chromatography and scanning through a UV Spectrophotometer were used to determine the amount of drug present in the formulation.
-
- Spreadability
Using two slides, this nanogel parameter (5 cm2) was found. After placing 0.5g of the formulation in the center of two slides, it was left alone for a minute. We measured and compared the diameter of the nanogel's spread circle.
-
- Viscosity
The viscosity of the nanogel formulation was measured using a Brookfield Rheometer equipped with a spindle that rotates at 10 rpm. The assembly was attached to a water bath that was kept at 25°C and was thermostatically controlled. After the viscosity was calculated, it was put to the beaker that had a thermostatic jacket on. After allowing the spindle to travel through the nanogel, the values were recorded.
-
- In-vitro drug release study
The formulation's in vitro drug release was investigated using the Franz diffusion cell device. The formulation was applied to a dialysis membrane that was positioned in the center of the Franz diffusion cell's donor-receptor chamber. A constant 30°C was maintained. A magnetic field was used to continually swirl this assembly while it was subjected to magnetic stirring. The percentage of medication released from the nanogel formulation was computed.
-
- Stability study
Following ICH criteria, the nanogel's accelerated stability was achieved. The stability of topical nanogel was evaluated using a three-month study conducted in an environmental stability chamber at 25 ±2°C and 60 ±5% relative humidity. The mixture was moved into glass vials with an amber tint, sealed, and stored in the stability room. After three months, the drug content, uniformity, and in vitro drug release were assessed.
APPLICATION OF NANOGEL[31]
-
- Local Anaesthetics:
Drugs known as local anaesthetics provide analgesia and provide pain relief. By blocking Na voltage gated channels, which impede nerve impulses in nerve cell membranes, local anaesthetics provide analgesic effects.
-
- Herbal nanogels:-
Herbal nanogels can be used topically or sublingually. The oral route is the most effective way to administer many medicinal medications. However, when medications are taken orally, a number of processes are observed, including absorption, distribution, metabolism, and excretion, all of which take time for the medication to take action. In addition, oral dosing exhibits GI breakdown, low absorption, and first pass metabolism impact. However, there are a number of benefits of using herbal nanogel trans dermally over other traditional drug delivery methods, including improved patient compatibility, regulated drug release, and avoidance of the medication's first-pass metabolism effect. One type of herbal nanogel is one that is based on curcumin.
-
- CNS delivery
The delivery of hydrophilic drugs to the brain remains a difficulty in the treatment of numerous illnesses related to the central nervous system. The ionic gelatin approach was utilized to prepare methotrexate-loaded nanogel. Novel insights into the cell biology of the blood-brain barrier have emerged in the context of drug delivery to the central nervous system.
-
- Protein delivery: -
More therapeutically active proteins have been found recently and are receiving interest for treating certain illnesses such autoimmune, viral, and cancerous diseases.
-
- Anticancer therapy: -
Drugs that are therapeutically effective and have minimal adverse effects on nearby tissues are delivered specifically to treat cancer. Numerous polymeric nanogels have found application in cancer treatment. Chemotherapeutic medications that are integrated into the nanogel have higher permeability, retention, and bioavailability. Drugs are being delivered more successfully via nanogel in cancer chemotherapy. Genexol-PM is one example of a polymeric nanogel that has been approved by the FDA for use in breast cancer patients. Another illustration is the use of doxorubicin nanogels polymerized with chitin to treat cancers of the liver, lungs, prostate, and breast.
REPORTED ACTIVITIES OF HERBAL NANOGELS FORMULATION
- Eupatorium adenophorum (Asteraceae) leaves are utilized in Ayurveda as an antibacterial, analgesic, and wound therapy. The anti-inflammatory properties of the ethanolic extracts of Asteraceae were investigated by Negi et al. When used to treat rat paw oedema caused by carrageenan, the greenish translucent Carbopol 934 gel containing 1% of this extract demonstrated strong anti-inflammatory effects [32].
- Cleodendron infortunatum Linn. leaf extracts have long been used to treat epilepsy, bronchitis, asthma, fever, and skin infections. Das et al. used the artificial polymer Carbopol 940 to synthesize the leaf extract into a nanogel. There was no skin irritation and the gel containing 2.5% extract demonstrated good anti-inflammatory efficacy [33].
- The anti-inflammatory and analgesic properties of a gel comprising Albizia lebbeck's methanolic extracts were documented by Rajesh et al. Compared to Carbopol 934 and other combinations, the nanogel prepared with sodium alginate and carboxymethyl cellulose (CMC) has demonstrated superior penetration [34].
- Pongamia pinnata (Millettia pinnata) roots have the ability to stimulate angiogenesis and reduce inflammation. In addition, the roots are used as a toothbrush to treat gonorrhoea, treat skin and vaginal infections, and eradicate parasitic worms. The anti-inflammatory properties of the root extract-containing nanogel were investigated by Paul et al. After encasing the root's aqueous extract with silver nanoparticles, a paraffin wax foundation was used to create a gel. Bovine serum albumin's heat-induced denaturation was significantly reduced by the gel [35].
- According to Dwivedi and Gupta, a non-irritating nanogel comprising sodium CMC, Carbopol 934, and leaf ethyl acetate extracts of Sesbania grandiflora can be utilised to treat a variety of skin inflammations. Anti-ulcer, anti-oxidant, analgesic, antipyretic, antimicrobial, anti-cancer, anticonvulsant, anxiolytic, and hepatoprotective qualities are all present in Sesbania grandiflora leaves [36].
- Lantana camara leaves have anti-inflammatory and anti-haemorrhagic properties. Using Carbopol 934, two extract concentrations—2.5% and 5%—were formed into gels. According to Pawar and Shamkuwar's documentation, the 2.5% extract gel exhibited superior qualities compared to the 5% gel [37].
- Butea frondosa stem bark ethanolic extracts exhibit anti-inflammatory and analgesic properties. Shankar et al.'s optimised gel formulation, which included Carbopol 934 and DMSO, revealed that the diffusion and permeation percentages were 92.37 and 98.29 after eight hours [38] .
- Goyal et al. discuss the idea of creating a gel with extracts of Withania somnifera (ashwagandha) and Boswellia serrata (kunduru). Because it can inhibit 5-lipoxygenase, Boswellia serrata (pentacyclic triterpenes) possesses anti-inflammatory and anti-arthritic properties. The anti-inflammatory and anti-arthritic properties of Withania somnifera are attributed to withaferin A, a cell-permeable steroidal lactone found in the plant [39].
- Giovana et al. conducted a comparison investigation on the bactericidal activity of the glycolic extracts of pomegranate, apricot, and green tea. Because of its gallic tannins and alkaloids, pomegranate is used for its astringent and antibacterial properties. Apart from its similar function, apricot also possesses mucoprotective and remineralizing properties. Green tea has many health advantages, such as anti-inflammatory, sunscreen, chemoprotective, and anti-oxidative properties. Green tea gallic acid extract gel shown strong antibacterial activity against Escherichia coli, Pseudomonas aeruginosa, and Staphylococcus aureus. Green tea's catechin content is thought to be responsible for this action [40].
- Jadhav et al. investigated the antibacterial activity of Tridax procumbens ethanolic extracts against Staphylococcus aureus. Strong antibacterial activity was demonstrated for Carbopol 940 gel with 1% extract [41].
- Chewing Spilanthus acmella leaves and petals, also called Akkalkara, numbs the gums and tongue. It is also used as an anti-inflammatory and to alleviate toothaches. In order to treat toothache, tooth decay, and mouth ulcers, Gupta et al. investigated the advantages of incorporating ethanosomes containing plant extracts into a mucoadhesive oral gel [42] .
- Aloe vera is frequently used as an antifungal agent, to promote immunity (by activating macrophages), and to expedite the healing process of wounds (including wound contraction, wound closure, and restoration of functional barriers). In rats with skin excision wounds, the aloe vera-Carbopol 934 nanogel formulation developed by Khan et al. accelerated the pace of wound contraction. The leaf extracts' inclusion of mannose-6-phosphate is what gives rise to this capability. Collagen synthesis and fibroblast activity can be increased by mannose [43].
CHALLENGES AND OPPORTUNITIES
The pharmaceutical industry is expanding and now has access to a multibillion dollar market as a result of nanogels created with herbal drugs. Still, there are still a lot of obstacles to overcome before using herbal medications in clinical studies. The World Health Organisation (WHO) estimated that 80% of people on the planet will heavily rely on herbal-based medications to address their medical demands [44]. People still search for complementary medicine in the form of alternative medicine, even in spite of the business potential of allopathic pharmaceuticals. The substantial shifts in people's social, political, and economic values have significantly reduced the therapeutic application of herbal drugs [45]. Effective research programmes can greatly assist herbal medications in becoming much more applicable clinical practice with the use of nanogels. Because of its unique qualities, which include biocompatibility and degradability, swelling in aqueous media, increased drug loading capacity, permeability and particle size, non-immunologic reaction, and colloidal stability, nanogel is always open to new opportunities [46]. The design of the delivery system that responds to the environmental stimuli factor that regulates the medication release rate at the site of action is made easier by nanogel. This boosts the effectiveness of the herbal medications, allowing them to perform many functions [47, 48].
CONCLUSION
A versatile platform for enhancing the effects of herbal drugs is nanogel formulation. Nanogels have a number of applications as a medication carrier in herbal formulations because of their flexibility and versatility. Excellent properties allow di-sulfide cross-linked polymeric nanogels to be produced as bio-responsive delivery methods. Herbal nanogel may be able to transform the natural substance into a very effective drug for the treatment of a range of illnesses, including diabetes, cancer, and skin conditions. PLGA, PEG, chitosan, and other polymers are frequently utilised in the production of cross-linked herbal nanogels. In comparison to oral medication administration, these cross-linked nanogels show great promise for transdermal drug delivery, which affects patient compliance with herbal medications and has less adverse effects. Even though a lot of natural medicines have been developed, not all of them are safe; some have unfavourable side effects, are extremely poisonous, or interact negatively with prescription medications. An evaluation of the herbal product's quality is necessary for it to be approved by the current medical system. The contemporary pharmaceutical industry's potential lies in herbal nanogel formulations, which can yield the required synergistic effect at low medication concentrations and minimal adverse effects. For all intents and purposes, the herbal nanogel product may represent a unique medication delivery mechanism.
REFERENCES
- Viswanathan B, Salim M, Subhramani A, Sruthi. Historic review on modern herbal nanogel formulation and delivery methods. International journal of pharmacy and pharmaceutical sciences. 2018;10(10):1-10.
- Fateh AL, Magbool F, Elamin I, Shayoub M. Nanogel a pharmaceutical carrier- review article. Scholars journal of applied medical sciences.2017; 5(11F): 4730-4736.
- Iordana Neamtu, Alina Gabriela Rusu, Alina Diaconu, Loredana Elena Nita and Aurica P. Chiriac. Basic concepts and recent advances in nanogels as carriers in medical applications. Drug delivery 2017; 24(1):539-557.
- Vickers A, Zollman C. ABC of complementary medicine: herbal medicine. Br Med J 1999; 319:1050-3.
- Pallavi M. Chaudhari, Aarti V. Paithankar. Herbal Nanogel Formulation: A Novel Approach. Journal of Science and Technology 2020; 5(5):149-153.
- Brahmankar DM, Jaiswal SB. Biopharmaceutics and pharmacokinetics-a treatise. 1st ed. Delhi: Vallabh Prakashan Publishers 1995;(1):296-7.
- Rasheed A, Reddy SB, Roja. A review on the standardisation of herbal formulation. Int J Phytother 2012;12:74-88.
- Bonifacio BV, Silva PB, Ramos MAS, Negri KMS, Bauab TM, Chorilli M. Nanotechnology-based drug delivery systems and herbal medicines: a review. Int J Nanomed 2013;9:1-15.
- Ghosh V, Saranya S, Mukherjee A, Chandrasekaran N. Antibacterial microemulsion prevents sepsis and triggers healing of wound in wistar rats. Colloids Surf B 2013;105:52–7.
- Rajendran R, Radhai R, Kotresh TM, Csiszar E. Development of antimicrobial cotton fabrics using herb loaded nanoparticles. Carbohydr Polym 2013;91:613–27.
- Jain N, Jain R, Thakur N, Gupta BP, Jain DK, Banveer J, et al. Nanotechnology: a safe and effective drug delivery system. Asian J Pharm Clin Res 2010;3:159-65.
- Kesarwani K, Gupta R. Bioavailability enhancers of herbal origin: an overview. Asian Pac J Trop Biomed 2013;3:253–66.
- Bhattacharya S, Ghosh AK. Phytosomes: the emerging technology for the enhancement of bioavailability of botanicals and nutraceuticals. Int J Aesthetic Antiaging Med 2009;2:87–91.
- Su YL, Fu ZY, Zhang JY, Wang WM, Wang H, Wang YC. Preparation of radix salvia nanoparticles. Powder Technol 2008;184:114–21.
- Amamoto,Y.; Otsuka, H.; Takahara, A. Synthesis and characterization of polymeric nanogels. Nanotechnol. Life Sci. Online 2012;2(10):12-14.
- Mota, A.H.; Sousa, A.; Figueira, M.; Amaral, M.; Sousa, B.; Rocha, J.; Fattal, E.; Almeida, A.J.; Reis, C.P. Chapter 19-Natural-based consumer health nanoproducts: Medicines, cosmetics, and food supplements. In Handbook of Functionalized Nanomaterials for Industrial Applications; Mustansar Hussain, C., Ed.; Elsevier: Amsterdam, The Netherlands, 2020;527–578.
- Kishimura, A.; Koide, A.; Osada, K.; Yamasaki, Y.; Kataoka, K. Encapsulation of myoglobin in pegylated polyion complex vesicles made from a pair of oppositely charged block ionomers: A physiologically available oxygen carrier. Angew. Chem. Int. Ed. 2007, 46: 6085–6088.
- Basak, S.; Khare, H.A.; Roursgaard, M.; Kempen, P.J.; Lee, J.H.; Bazban-Shotorbani, S.; Kræmer, M.; Chernyy, S.; Andresen, T.L.; Almdal, K.; et al. Simultaneous cross-linking and cross-polymerization of enzyme responsive polyethylene glycol nanogels in confined aqueous droplets for reduction of low-density lipoprotein oxidation. Biomacromolecules 2021, 22, 386–398.
- Yallapu, M.M.; Jaggi, M.; Chauhan, S.C. Design and engineering of nanogels for cancer treatment. Drug Discov. Today 2011, 16, 457–463.
- Ezhilararasan, D.; Lakshmi, T.; Raut, B. Novel Nano-Based Drug Delivery Systems Targeting Hepatic Stellate Cells in the Fibrotic Liver. J. Nanomater. 2021, 2021, 4674046.
- Okay, O.; Lozinsky, V. Synthesis and structure-property relationships of cryogels. Adv. Polym. Sci. 2014, 263, 103.
- Swati Talele, Preetam Nikam, Braja Ghosh, Chaitali Deore, Ashwini Jaybhave et al. (2017) A Research Article on Nanogel as Topical Promising Drug Delivery for Diclofenac sodium. Indian J of Pharmaceutical Education and Research 51(4S): 580-597.
- Ayesha Siddiqua Gazi, Abbaraju Krishnasailaja (2018) Preparation & Evaluation of Paracetamol Solid Lipid Nanoparticles by Hot Homogenization Method. J Nanomedicine Research 7 (2): 152-154.
- Dr. Prathima Srinivas, K Sai Preeti (2014) Formulation & Evaluation of Gemcitabine Hydrochloride Loaded Solid Lipid Nanoparticles. J Global Trends in Pharmaceutical Sciences 5(4): 2017-2023.
- Farhana Sultana, Manirujjaman, Md. Imran-Ul-Haque, Mohammad Arafat, Sanjida Sharmin (2013) An Overview of Nanogel Drug Delivery System. J Applied Pharmaceutical Science 3(1): S95-S105.
- Chopade Swapnil, Khabade Sheeba, Patil Ajit, Powar Sayali (2018) Formulation Development and Evaluation of Anti-Inflammatory Potential of Topical Tenoxicam Nanogel on Animal Model. International J Recent Scientific Research 912(C): 29951-29957.
- McAllister, K.; Sazani, P.; Adam, M.; Cho, M.J.; Rubinstein, M.; Samulski, R.J.; DeSimone, J.M. Polymeric nanogels produced via inverse microemulsion polymerization as potential gene and antisense delivery agents. J. Am. Chem. Soc. 2002, 124, 15198–15207.
- Striegel, A.M.; Haidar Ahmad, I.A. Determining the Chemical-Heterogeneity-Corrected Molar Mass Averages and Distribution of Poly(styrene-co-t-butyl methacrylate) Using SEC/MALS/UV/DRI. Chromatographia 2018, 81, 823–827.
- Striegel, A.M. Chapter 10—Size-exclusion chromatography. In Liquid Chromatography, 2nd ed.; Fanali, S., Haddad, P.R., Poole, C.F., Riekkola, M.-L., Eds.; Elsevier: Amsterdam, The Netherlands, 2017; pp. 245–273.
- Muniraj S N, Yogananda R, Nagaraja T S, Bharathi D R. Preparation And Characterization Of Nanogel Drug Delivery System Containing Clotrimazole An Anti-Fungal Drug. Indo-American J Pharmaceutical Research 2020; 10(07): 1013-1022.
- 1 Priti Jadhao, 2 Dr. A. A. Harsulakar. A Review On: Herbal Nanogel. Indo American Journal Of Pharmaceutical Sciences 2022;09 (02): 19-27.
- Klinger D, Landfester K. Stimuli-responsive microgels for loading and release of functional compounds: fundamental concepts and applications. Polymer 2012;53:5209-31.
- Ansari SH, Islam F, Sameem M. Influence of nanotechnology on herbal drugs: a review. J Adv Pharm Technol Res 2012;3:142-6.
- Rajesh B, Das S, Dharmajit P, Pavani M. Formulation design and optimization of herbal gel containing albizia lebbeck bark extract. Int J Pharm Pharm Sci 2014;6:111-4.
- Paul S, Dhinakaran I, Mathiyazhagan K, Raja M, Sasikumar CS, Varghese JC. Preparation of nanogel incorporated with silver nanoparticles synthesized from pongamia pinnata. L root. Int J Sci Res Knowl 2015;3:314-25.
- Negi A, Sharma N, Singh MF. Formulation and evaluation of an herbal anti-inflammatory gel containing Eupatorium leaves extract. J Pharmacogn Phytochem 2012;1:112-7.
- Chacko RT, Ventura J, Zhuang J, Thayumanavan S. Polymer nanogels: a versatile nanoscopic drug delivery platform. Adv Drug Delivery Rev 2012;64:836-51.
- Shankar MU, Murthy PN, Gourishyam P, Sanjay K. Formulation development and standardization of herbal gel containing methanolic extract of Butea frondosa. Int Res J Pharm 2011;2:126-9.
- Das S, Haldar PK, Pramanik G. Formulation and evaluation of herbal gel containing clerodendron infortunatum leaves extract. Int J PharmTech Res 2011;3:140-3.
- Dwivedi S, Gupta S. Formulation and evaluation of herbal gel containing sesbania grandiflora (L.) poir. leaf extract. Acta Chim Pharm Indica 2012;2:54-9.
- Vickers A, Zollman C. ABC of complementary medicine: herbal medicine. Br Med J 1999;319:1050-3.
- Gupta N, Patel AR, Ravindra RP. Design of akkalkara (spilanthes acmella) formulations for antimicrobial and topical anti inflammatory activities. Int J Pharm Bio Sci 2012;3:161-70.
- Pawar DP, Shamkuwar PB. Formulation and evaluation of herbal gel containing lantana camara leaves extract. Asian J Pharm Clin Res 2013;6:122-4.
- Pires AM, Araujo PS. Percepcao de risco e conceitos sobre plantas medicinais, fitoterápicos e medicamentos alopáticos entre gestantes [risk perception and concepts about medicinal plants, herbal and allopathic medicines among pregnant women]. RBSP 2011;35:320–33.
- Khan AW, Kotta S, Ansari SH, Sharma RK, Kumar A, Ali J. Formulation development, optimization and evaluation of aloe vera gel for wound healing. Pharmacogn Mag 2013;9:S6-10.
- Badke MR, Budo MLD, Silva FM, Ressel LB. Plantas medicinais: o saber sustentado na prática do cotidiano popular [medicinal plants: popular knowledge in sustained daily practice]. Esc Anna Nery 2011;15:132–9.
- Shilpi Agarwal, Pradip Kumar Karar, Gaurav Agarwal. Semi-herbal nanogel of clindamycin phosphate and Aloe vera: formulation and evaluation. Mod Appl Bioequiv Availab 2017;2:5.
- Aminu N, Ming TS. Applicability of nanoparticles-hydrogel composite in treating periodontal diseases and beyond. Asian J Pharm Clin Res 2017;10:65-7.


 Akshita Deb*
Akshita Deb*
 Deeparani Urolagin
Deeparani Urolagin
 Ansari Aashif Raza Mohd Imtiyaz
Ansari Aashif Raza Mohd Imtiyaz
 Samir Panda
Samir Panda
 Arundhati Kashyap
Arundhati Kashyap
 10.5281/zenodo.11208343
10.5281/zenodo.11208343