Chronic obstructive pulmonary disease (COPD) plays a significant role in global morbidity and mortality rates, typified by progressive airflow restriction and lingering respiratory symptoms. Recent explorations in molecular biology have illuminated the complex mechanisms underpinning COPD pathogenesis, providing critical insights into disease progression, exacerbations, and potential therapeutic interventions. This review delivers a thorough examination of the latest progress in molecular research related to COPD, involving fundamental molecular pathways, biomarkers, therapeutic targets, and cutting-edge technologies. Key areas of focus include the roles of inflammation, oxidative stress, and protease–antiprotease imbalances, alongside genetic and epigenetic factors contributing to COPD susceptibility and heterogeneity. Comprehending the molecular foundation of COPD carries substantial potential for the creation of tailored treatment strategies and the enhancement of patient outcomes. By integrating molecular insights into clinical practice, there is a promising pathway towards personalized medicine approaches that can improve the diagnosis, treatment, and overall management of COPD, ultimately reducing its global burden.
Diagnostic Method, Chronic Obstructive Pulmonary Disease, Global Scenario
COPD is defined as Chronic obstructive pulmonary disease it is the airflow restriction that does not change significantly over several months. The condition consists of chronic bronchitis, small airways disease (bronchiolitis), and emphysema in varying proportions across individuals. COPD is a leading cause of illness and mortality worldwide. Tobacco exports to developing countries like India, Mexico, Cuba, Egypt, South Africa, and China are expected to significantly boost the prevalence of smoking among Western women. Asthma is a significant health risk, but there are few treatment choices available, with most drugs specifically designed for this condition. To develop effective COPD medications, it's important to study the disease's epidemiology, natural history, genetic and environmental risk factors, and pathophysiology. This review paper comprise of Epidemiology, Pathophysiology, Etiology, Diagnosis, Risk Factors, Treatment.
Fig: 1
Epidemiology:
COPD is the worldwide cause due to the expouse to the toxic substance. The world's population is aging, smoking rates are rising, and deaths from ischemic heart disease and infections are decreasing. Chronic obstructive pulmonary disease (COPD) is the world's fourth biggest cause of death, accounting for 3.5 million deaths in 2021, or almost 5% of total global deaths. Low- and middle-income countries (LMIC) account for about 90% of COPD fatalities among those under the age of 70.COPD is the eighth biggest cause of poor health worldwide, as defined by disability-adjusted life years. Tobacco use is responsible for nearly 70% of COPD cases in high-income nations. Tobacco use accounts for 30-40% of COPD cases in low- and middle-income countries, and household air pollution is a key contributor (1). Although marketed as a nicotine replacement medication, vaping has become a technique for attracting nonsmokers. Tobacco is a prominent ingredient in several vaping and e-cigarette products. Nicotine has been flavored with THC, CBD oils, Vitamin E, and other ingredients to appeal to non-smokers and young adults (2-5). COPD is a prevalent and curable illness affecting 5-22% of adults over 40. COPD is a prominent cause of hospitalization and has significant healthcare costs. 6-8 According to Gershon et al., the annual COPD incidence is 5.9 cases per 1000 people. The study found a lifetime COPD risk of 26.6%. The risk was higher for men, smokers, those over 40, and those living in rural regions. More people will be diagnosed with COPD than with heart failure, acute myocardial infarction, or some malignancies (9). There is insufficient evidence to accurately evaluate the morbidity, death, and overall burden of COPD. The majority of COPD estimations lack consistency and may be underestimated (6, 10, 11). The CDC reported that 9.0 million persons were diagnosed with chronic bronchitis in 2018. 3.6 percent of individuals were diagnosed with chronic bronchitis in the same years. Emphysema affects around 3.8 million individuals, or 1.5% of the population.
Pathophysiology:
- Tobacco use causes a chronic inflammatory reaction in the lungs. Repeated exposure can trigger a chronic inflammatory response in the lungs, resulting in emphysematous alterations, fibrosis, air trapping, and increasing airflow limitation.2 Inflammatory alterations, including tissue damage and fibrosis, are commonly observed in the airways, lung parenchyma, and pulmonary vasculature 12, and typically worsen with increased exposure. Inflammation in COPD patients persists even without exposure. Smokers who develop COPD exhibit specific patterns of inflammation, including increased CD8+ and Tc1 cells.
- These cells, along with neutrophils and macrophages, emit inflammatory mediators and enzymes that interact with structural cells in the airways, lung parenchyma, and pulmonary vascular system.
- E-cigarette usage has been associated to severe lung injuries, including eosinophilic pneumonia, alveolar hemorrhage, respiratory bronchiolitis, and other abnormalities2 .Oxidative stress and excess proteinases in the lung can alter the inflammatory response. Autoantigens and persistent bacteria contribute significantly to inflammation20 .COPD patients experience higher levels of oxidative stress in their lungs, exacerbating the condition 20 .In COPD patients, an imbalance exists between proteases that break down connective tissue components and anti-proteases that prevent breaking.
- Emphysema patients often have protease-mediated degradation of elastin, a key connective tissue component in the lung parenchyma. Inflammation and constriction of peripheral airways cause reduced FEV. Emphysema causes parenchymal damage, which can impede airflow. FEV1 and FEV1/FVC ratios associated with inflammation, fibrosis, and luminal exudates in small airways12 .The peripheral airway blockage cause hyperinflation by trapping air on expiration.
- Hyperinflation lowers inspiratory capacity during exercise, resulting in dyspnea and limited exercise capacity14.
- The peripheral airway blockage causes hyperinflation by trapping air on expiration. Hyperinflation lowers inspiratory capacity during exercise, resulting in dyspnea and limited exercise capacity14.Hypoxic vasoconstriction in tiny pulmonary arteries causes intimal hyperplasia and smooth muscle hypertrophy, resulting in pulmonary hypertension. Progressive pulmonary hypertension leads to right ventricular hypertrophy and, finally, right-sided heart failure.
Etiology:
Etiology of COPD are as follows:
- Smoking
- Environmental Exposures
- Genetic Factors
- Early Life Factors
- Smoking
The primary risk factor for COPD is tobacco use.15, 16 In high-income nations, tobacco use accounts for more than 70% of COPD cases, whereas in low- and middle-income countries, it accounts for 30% to 40% of cases. The effects of smoking include oxidative damage, cilia malfunction, and an inflammatory response.17 Additional etiologies include indoor biomass fuel combustion, air pollution, and occupational exposure to dust, chemicals, and fumes.18,19,20 Both high levels of particulate matter and large dosages of pesticides are associated with a higher risk of COPD(21,22,23,24)The pathophysiology of COPD also includes oxidative stress and an imbalance in proteases and antiproteases, particularly in those with alpha-1 antitrypsin deficiency25. Processes that impact proper lung development and, therefore, lung function can raise the chance of developing COPD.26 These processes may have their origins in childhood, adolescence, pregnancy, and delivery. Cigarette smoke contains dangerous compounds that cause lung tissue damage, oxidative stress, and chronic inflammation. The airways and alveoli undergo structural alterations as a result of this exposure, including:
- Inflammation: Smoke causes an inflammatory reaction that harms the airway and lung walls. Smoking affects the function of cilia, which are necessary for removing mucus from the airways. This results in ciliary dysfunction.
- Oxidative Injury: Elevated oxidative stress aggravates inflammation and aids in the decomposition of lung tissue
2. Genetic Factors
The best-defined causal genetic illness is alpha-1 antitrypsin deficiency, which is a major cause of emphysema in nonsmokers and significantly increases disease vulnerability in smokers. More than 30 genetic variants have been linked to COPD or deterioration in lung function in specific populations, but none have been proved to be as significant as alpha-1 antitrypsin13
3. Environmental Exposures
Other inhalational exposures that can lead to COPD include:
• Indoor air pollution is prevalent in LMICs where biomass fuels (e.g., wood or animal dung) are used for cooking and heating.
• Long-term exposure to dust, chemicals, and odours in work places can raise the risk.
• Air pollution is a major contributor, especially in cities.
4. Early Life Factors:
Several early-life circumstances, such as poor fetal growth, premature birth, and severe respiratory infections during childhood, might impede optimum lung development and raise the risk of having COPD later in life.
DIAGNOSIS:
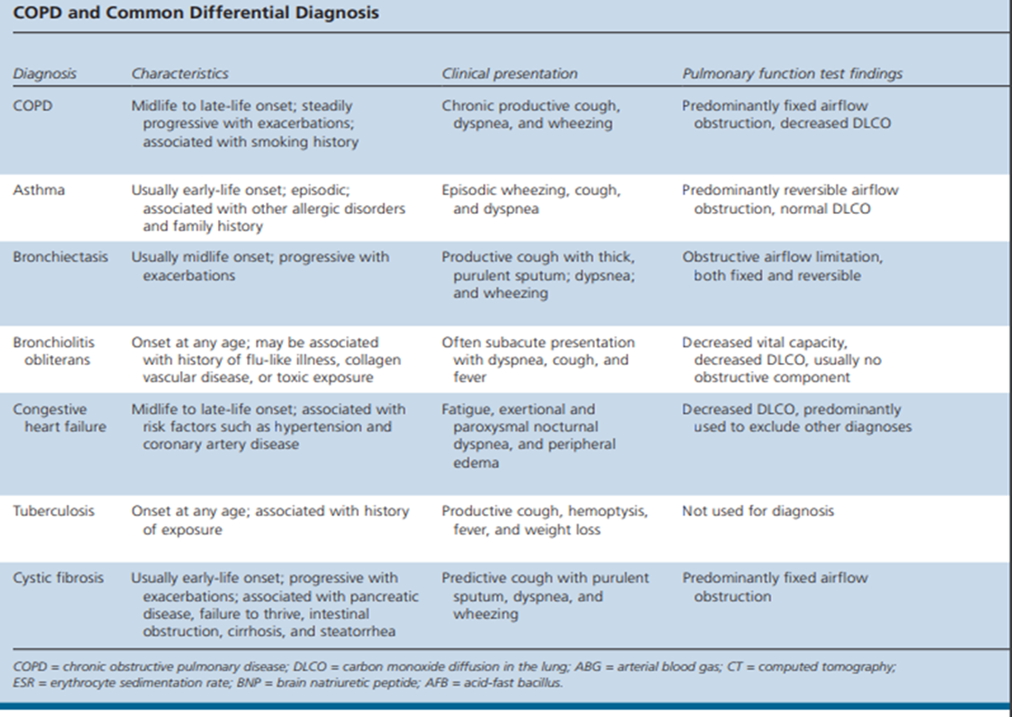
- COPD is a chronic condition that can be diagnosed clinically. However, in certain cases, spirometry is necessary for a conclusive diagnosis. COPD should be diagnosed in patients with symptoms such as dyspnea, chronic cough, or sputum production, as well as risk factors such family history, environmental history, and smoking history.2To provide a smoking history, give the age of initiation, average daily smoking amount, and current status or stop date. Tobacco smoke, home cooking and heating, occupational dusts, and chemicals are all significant risk factors for Copd development.
- COPD symptoms include a chronic cough, fluctuating sputum output, and increased dyspnea (27,28) These are the primary signs to consider while determining the necessity for antibiotics.
- Sputum production can begin years before airway restrictions, indicating the existence of COPD.28 Some people may experience airway blockages without coughing or producing sputum. The initial symptom of COPD is coughing. Coughs typically start intermittently and escalate to everyday or even all-day symptoms. Chronic coughing with COPD can be unproductive.29 Sputum output is more difficult to evaluate. Large quantities of sputum may indicate bronchiectasis. Increased sputum output and purulence may indicate a bacterial infection, exacerbating COPD symptoms.30
- Dyspnea is the primary symptom causing individuals to seek medical assistance. COPD symptoms include progressive dyspnea, characterized by greater effort to breathe, heaviness, air hunger, or gasping31. Non-specific symptoms in COPD patients include wheezing and chest discomfort. Severe COPD patients often experience fatigue, weight loss, and anorexia32. To diagnose COPD, it's necessary to acquire a detailed medical history from each patient. The history should include exposure to harmful substances like tobacco, as well as occupational and environmental influences. Prior medical history should include asthma, allergies, nasal polyps, sinusitis, and respiratory infections. Record family's history of COPD and other chronic diseases.
- Detailed information about the patient's respiratory symptoms, including seasonality, duration, and time of onset. Consider the patient's history of exacerbations and frequency of hospitalizations each year. Evaluate all comorbidities and address the impact of COPD on patients' social, economic, and sexual well-being. COPD is diagnosed when the post-bronchodilator spirometry FEV1/FVC ratio is less than 0.70 (27,33).
Spirometry is the most reliable and objective measurement of airflow limitation. Spirometry measures are compared to relevant reference values depending on age, height, gender and race.


 Indumathy . K*
Indumathy . K*
 10.5281/zenodo.14542901
10.5281/zenodo.14542901