Abstract
Renal failure is defined as the failure of excretory functions of the kidney, and it is characterized by decrease in the glomerular filtration rate (GFR).The persistent, long-lasting, and irreversible weakening of kidney functioning leads to chronic renal failure. Hemodialysis is the process used to eliminate waste products and harmful chemicals from the body and maintain the body fluids to normal,dialysis is performed via a machine called artificial kidney works based on the principle of Diffusion. The International Association for the Study of Pain (IASP) defines pain as an unpleasant sensory or emotional experience that is linked to actual or potential tissue damage. The visual analogue scale (VAS) is one of the pain rating scales used to measure the degree or frequency of pain. Electrolytes play a key role in basic life support functions.Major electrolytes involved are Sodium,potassium, calcium, and phosphate. Elevations or decreases in electrolyte levels lead to imbalance. Quality of life (QoL) refers to the state of being that a population or an individual has with respect to all of the good and bad aspects of their life at a given moment in time. A person's physical, mental, and spiritual well-being. The four primary domains of QoL, as per "engaged theory," are politics, economy, culture, and ecology. The concept of quality of life, or QoL, is becoming more widely recognized as a crucial indicator of how a disease impacts a patient's life, particularly in the case of chronic illnesses like chronic kidney disease.
Keywords
Chronic renal failure (CRF), Hemodialysis, Artificial kidney, Visual analogue scale, Quality of life (QoL).
Introduction
The major nitrogenous wastes eliminated by the animals are urea, uric acid, and ammonia. Ammonia is the most harmful type and requires a lot of water to be eliminated. Humans and other mammals mostly excrete urea, and which is referred to as ureotelic and is somewhat soluble in water. The liver transforms ammonia from metabolism into urea, which is then released into the bloodstream and filtered and eliminated by the kidneys. The excretion process removes the byproducts of numerous chemical reactions and biological processes that are no longer required by the human body. [1]
HUMAN EXCRETORY SYSTEM
The human excretory system consists of a group of organs responsible for eliminating waste from the body. There are two kidneys, a pair of ureter, a bladder, and a urethra that make up the human excretory system.[38]
NEPHRON
Metanephros, the most advanced type of nephrons, make up each adult human kidney, which has approximately one million of them. The Greek word "nephros," which means kidney, is the source of the English term "nephron." The fundamental structural and functional component of the kidney is called a nephron, and its microscopic structure is made up of renal tubules and renal corpuscles.[39]
KIDNEY FAILURE
Renal failure is defined as the failure of excretory functions of the kidney, and it is characterized by a decline in the glomerular filtration rate (GFR).[40]
The renal failure is mainly of two types,
- Acute renal failure
- Chronic renal failure
ACUTE RENAL FAILURE
Abrupt cessation of renal function is the hallmark of acute renal failure. It can be reversed in a matter of days to weeks. It is an unexpected, potentially fatal illness that needs to be treated immediately.[41]
ETIOLOGY:
- Acute nephritis - inflammation of kidneys, which usually develops by immune reaction.
- Damage of renal tissues by poisons like lead, mercury and carbon tetrachloride.
- Renal ischemia, which develops during circulatory shock.
- Acute tubular necrosis - necrosis of tubular cells in kidney, caused by burns, haemorrhage, snake bite, toxins and drugs.
- Sudden fall in blood pressure during haemorrhage, diarrhoea, severe burns and cholera.
- Blockage of ureter due to the formation of calculi.
CLINICAL MANIFESTATION:
One of the first indications of compromised renal function is oligouria, which is defined as reduced urine production, less than 400 milliliters per day or fewer than 20 milliliters per hour. [3]
reduction in the amount of urine produced, fewer than 100 milliliters daily. brought on by end-stage kidney disease, kidney stones, tumors, and severe obstructions such as renal failure in terms of function. [4]
Albumin, globulin, Bence-Jones protein, and mucoproteins are among the proteins in urine that are referred to collectively as "proteinuria."[6]
One of the most often diagnosed urological disorders is hematuria, which is defined as the abnormal presence of blood in the urine. The most helpful in terms of clinical practice is gross or micro-hematuria, which can be categorized as intermittent or constant, glomerular or non-glomerular, symptomatic or asymptomatic. Blood evident in the urine is referred to as gross hematuria. When urine seems normal on the surface but contains red blood cells (RBCs), this is known as micro-hematuria and can be detected with a dipstick or by microscopic urinalysis.
- Hypertension due to increased ECF volume.
CHRONIC KIDNEY FAILURE
The persistent, long-lasting, and irreversible weakening of kidney functioning is known as chronic renal failure. The nephrons that are not impacted can make up for it when some of them stop working. Chronic renal failure results from the compensatory mechanism failing when more and more nephrons lose their ability to function over the course of months or years. [42]
Chronic kidney disease divided into five stages,
- Stage 1: With normal or high GFR (GFR > 90ml/min)
- Stage 2: Mild CKD(GFR=60-89ml/min)
- Stage 3 (A): Moderate CKD(GFR=45-59ml/min)
- Stage 3(B): Moderate CKD (GFR=30-44ml/min)
- Stage 4: severe CKD(GFR=15-29ml/min)
- Stage 5: End stage CKD (GFR<15ml>
The stage of kidney disease is calculated by using glomerular filtration rate (GFR). A mathematical calculation based on an individual's age, gender, and serum creatinine level (creatinine is a waste product produced by muscle action and is a major sign of renal failure).
ETIOLOGY:
The kidneys' glomeruli, tubules, or interstitial tissues can become inflamed due to poisons and infections, most frequently autoimmune diseases.
- Renal calculi (kidney stones):
Hematuria, or blood in the urine, and pain in the belly, flank, or groin are frequently caused by renal calculi. Reduced urine volume or increased excretion of elements that might form stones, such as phosphate, calcium, oxalate, uric acid, cysteine, and xanthine, is linked to the development of the stones.[8]
A urethral stricture is a scarring-induced narrowing of the urethra that can impede the lower urinary tract, worsen the patient's quality of life by disrupting micturition, and harm the entire urinary tract, ultimately leading to renal failure.
Both the cause and the result of CKD are hypertension; when eGFR decreases, hypertension's incidence and severity rise. Complex interactions exist between CKD and hypertension[10,11]
Patients with chronic kidney disease are more likely to develop atherosclerosis, and they are also linked to new risk factors like abnormalities in the metabolism of calcium phosphate, anemia, malnourishment, fluid overload, variations in the volume of fluid in the body, and problems with the coagulation system[12]
- Slow poisoning by drugs or metals.
- Diabetes mellitus:
Elevated blood glucose levels have the potential to harm renal blood vessels. Blood vessels function less effectively when they are injured. Diabetes often results in excessive blood pressure, which damages the kidneys. [46]
CLINICAL MANIFESTATION:
Excess accumulation of protein metabolism end products, such as urea, nitrogen, and creatinine, in the blood is known as uremia.
Acidosis from uremia causes a coma and eventually death. One common CKD consequence is metabolic acidosis, which is more prevalent in patients with eGFR<30>
An increase in the volume of extracellular fluid due to the kidney's inability to eliminate salt and electrolytes results in the development of edema.
In cases of renal failure, the kidney does not secrete erythropoietin; instead, a decrease in red blood cell synthesis leads to normocytic normochromic anemia.
A calcitriol deficiency results in the development of secondary hyperparathyroidism (1,25-dihydroxycholecalciferol). Osteomalacia is the outcome of increased calcium loss from bones.
HAEMODIALYSIS
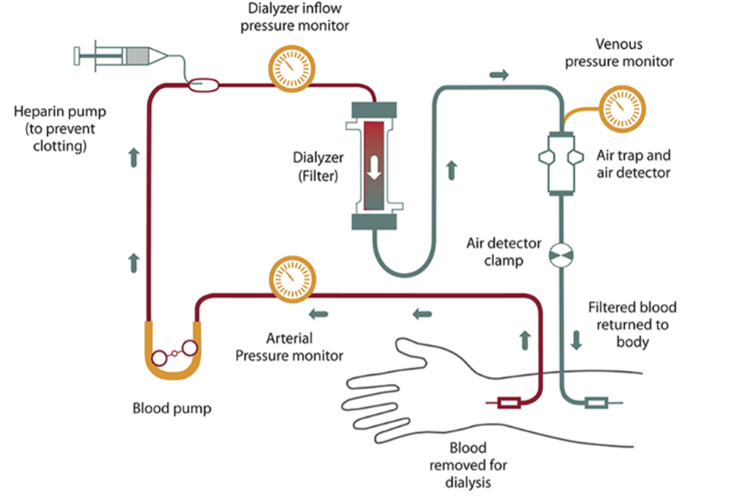
In cases of severe renal failure, hemodialysis is the process used to eliminate waste products and harmful chemicals fom the body and return the volume and composition of fluids to normal. It is commonly known as dialysis.[2]
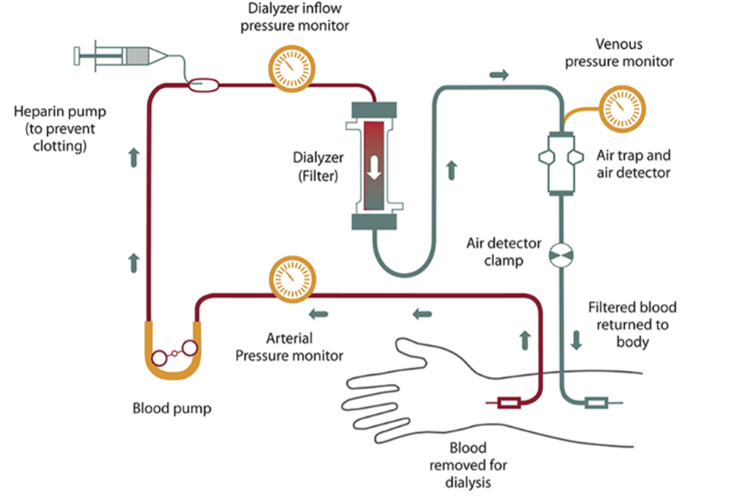
Fig.1 Procedure of Hemodialysis[28]
ARTIFICIAL KIDNEY
In cases of renal failure, dialysis is performed via a machine called an artificial kidney.It is used to treat the patients suffering from acute renal failureand Chronic or permanent renal failure.[43]
MECHANISM OF FUNCTION OF ARTIFICIAL KIDNEY
Diffusion of solutes through a semipermeable membrane from an area of higher concentration to an area of lower concentration is referred to as dialysis. This serves as the artificial kidney's basic idea. The artificial kidney filters the patient's arterial blood, which is then periodically or continuously returned to the body through the vein. When the blood is being run through the machine, heparin is utilized as an anticoagulant. Blood flows through a dialyzer inside the prosthetic kidney called a haemofilter, which has tiny channels in it. Positioned in the middle of two cellophane membranes. The membranes made of cellophane are permeable. The dialyzing fluid known as dialysate covers the exterior of these membranes. Fresh dialysate is continuously inserted into the artificial kidney to replace the used dialysate. By means of a concentration gradient, phosphate, creatinine, urea, and other undesirable chemicals from the blood enter the dialysate. Dialysate contains the essential nutrients that the body needs to diffuse into the blood. Through the cellophane membranes, nearly all substances with the exception of plasma proteins are transferred between the dialysate and blood. The dialysis equipment features many blood pumps with pressure monitors in addition to the dialyzer, making it simple for blood to flow from the patient to the machine and back again. Additionally, it features pumps for draining spent dialysate and for supplying new dialysate flow. Approximately 500 milliliters of blood can be used in the dialysis machine at once. About 200 to 300 mL of blood are passed via the dialysis machine every minute. Therate of dialysate flow is about 500 mL/minute.[2]
FREQUENCY AND DURATION OF DIALYSIS
Dialysis frequency and duration are determined by the degree of renal impairment. In severe uremia, dialysis is often performed three times a week for four to six hours.[2]
DIALYSATE
Depending on what the patient's body requires, the dialysate's concentration of different ingredients is changed. These compounds transfer from the blood to the dialysate because the fluid is devoid of urea, urate, sulphate, phosphate, and creatinine. Salt, potassium, and chloride ions are less concentrated in the fluid than they are in the uremic blood. However, the dialysate has higher concentrations of calcium ions, bicarbonate, and glucose than the uremic blood does.[44]
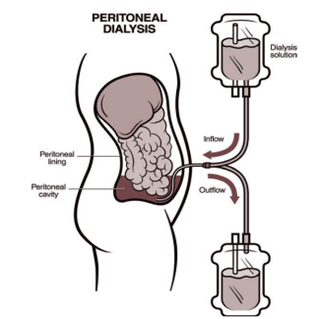
PERITONEAL DIALYSIS
The process of using the peritoneal membrane as a semipermeable membrane is called peritoneal dialysis. It is also utilized in the treatment of renal failure patients. Through the anterior abdominal wall, a catheter is introduced into the peritoneal cavity and sutured. Under gravity, the dialysate is pushed via this catheter. The necessary electrolytes from the dialysate enter the abdominal cavity's blood arteries through the peritoneum. Dialysate contains undesirable chemicals such as phosphate, creatinine, urea, and others that disperse from blood arteries. Later, gravity drawsdialysate out ofthe peritoneal cavity. [45]
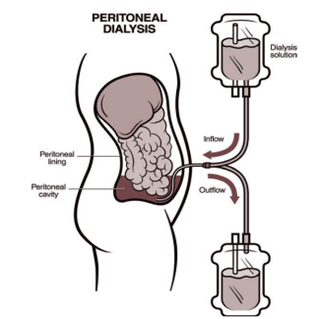
Fig.2 Procedure of Hemodialysis[28]
PAIN
A key component of signalling is pain. The pain system is made up of several components that sense an unpleasant input, transform it into a nerve impulse, and then quickly send that impulse up the spine, through the brain stem, and into the brain, where it is analysed and the best course of action is determined.[15]Margo McCaffery described pain a “whatever the experiencingperson says it is, existing whenever and wherever the person says it does” in 1968.[16]The International Association for the Study of Pain (IASP) defines pain as an unpleasant sensory or emotional experience that is linked to actual or potential tissue damage, or expressed in terms of such damage, in a more formal sense. [17]
Steps in nociception
- Transduction: A sensory neuron called a nociceptor, or pain receptor, reacts to potentially harmful stimuli.
- Transmission: the brain receives potential threat signals via the spinal cord.
- Perception: The brain views danger as real.
- Modulation: The body part can be made less dangerous by focusing attention on the painful area.
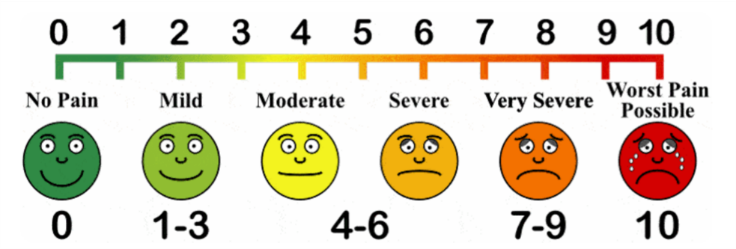
VISUAL ANALOGUE SCALE
One of the pain rating scales, the visual analogue scale (VAS), was initially employed by Hayes and Patterson in 1921.It is employed to quantify the degree or frequency of pain. A single handwritten mark is used to record scores at one location along a 10-cm line, which forms a continuum between the two extremes of the scale: "no pain" on the left end (0 cm) and "worst pain" on the right (10 cm). The five levels on the pain scale are none, mild, moderate, severe, and worst.[19]
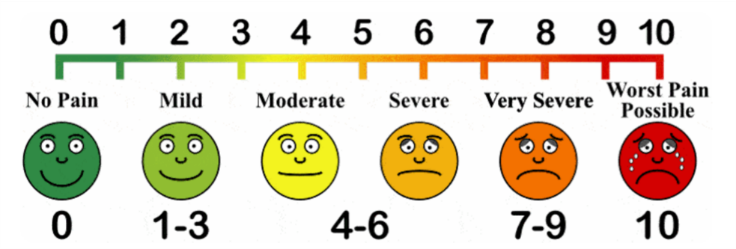
Fig.3Visual analogue scale for pain assessment[34]
IMPORTANCE OF ELECTROLYTES IN CKDThe basic life support functions including keeping cells electrically neutral and causing and conducting action potentials in the muscles and nerves, electrolytes are necessary. Sodium, potassium, chloride, calcium, phosphate, and bicarbonates are important electrolytes. We get electrolytes from our diet anddrinks. Elevations or decreases in electrolyte levels can cause serious health problems by interfering with regular bodily processes.[20]
POTASSIUM
Primarily, potassium is an intracellular ion. The sodium-potassium adenosine triphosphatase pump, which releases sodium in return for potassium, is principally in charge of maintaining the equilibrium between the two elements. The glomerulus is where potassium is filtered out of the kidneys. The thick ascending loop of Henle and the proximal convoluted tubule are the sites of potassium reabsorption. Secretion of potassium takes place at the distal convoluted tubule.
Normal range: 3.6 to 5.5 mmol/L
Hypokalemia occurs when serum potassium levels are under 3.6 mmol/L.
Hyperkalemia occurs when the serum potassium levels are above 5.5 mmol/L.
CALCIUM
Extracellular cations like calcium are crucial for blood coagulation, muscular contraction, skeletal mineralization, nerve impulse transmission, and hormone release. The major way we get calcium is through our food. The hormone-active form of vitamin D, 1,25-dihydroxy vitamin D3, is mainly responsible for controlling the absorption of calcium in the intestine. The distal tubule of the kidney is another area where parathyroid hormone controls calcium secretion. Calcium levels in the blood are lowered by calcitonin's action on bone cells.
Normal range: 8.8 to 10.7 mg/dL.
Hypocalcemia serum total calcium levels are less than 8.8 mg/dL.
Hypercalcemia serum total calcium levels exceed 10.7 mg/dL.
PHOSPHORUS
An extracellular fluid cation is phosphorus.The bones and teeth contain hydroxyapatite, which accounts for 85% of the total phosphorus in the body. The remaining 15% is found in soft tissues. It is essential to metabolic processes. PTH, calcitonin, and vitamin D3 all control phosphate at the same time as calcium. The main organ for excreting phosphorus is the kidneys. The main causes of phosphate imbalance include abnormal renal excretion, gastrointestinal problems, and reduced food intake.
Normal range: 3.4 to 4.5 mg/dL
Hypophosphatemia: less than 2.5 mg/dL
Hyperphosphatemia: greater than 4.5 mg/dL
PARAMETERS TO ASSESS RENAL FUNCTION
The kidneys play a vital role in the excretion of waste products and toxins such as urea, creatinine and uric acid, regulation of extracellular fluid volume, serum osmolality and electrolyte concentrations, as well as the production of hormones like erythropoietin and 1,25 dihydroxy vitamin D and renin.[36]
SERUM CREATININE
The body continuously produces creatinine, which is a by-product of creatine phosphate in muscle. Most of the time, the kidneys remove creatinine completely from the blood. Blood creatinine rises as a result of reduced renal clearance.[27]
Normal range:
For adult men, 0.74 to 1.35 mg/dL (65.4 to 119.3 micromoles/L)
For adult women, 0.59 to 1.04 mg/dL (52.2 to 91.9 micromoles/L)
BLOOD UREA
The by-product of protein metabolism and the urea cycle is urea, a nitrogen-containing chemical produced in the liver. Roughly 85% of urea is excreted via the kidneys, with the remaining portion going through the digestive system. In situations where renal clearance is reduced, such as acute and chronic renal failure or impairment, serum urea levels rise.[21]
Normal level: 5 to 20 mg/dl, or 1.8 to 7.1 mmol urea per liter.[33]
QUALITY OF LIFE
The term "quality of life" (QoL) refers to the state of being that a population or an individual has with respect to all of the good and bad aspects of their life at a given moment in time. A person's physical, mental, and spiritual well-being, relationships, education, employment status, social standing, money, sense of security and safety, freedom, decision-making autonomy, social belonging, and physical surroundings are a few frequent QoLfactors.[22 According to the World Health Organization, quality of life (QoL) is the subjective assessment of an individual's reality as it relates to their aspirations, as seen through the prism of their culture and value system. QoL is defined by the University of Toronto's Quality of Life Research Unit as an individual's capacity to fully appreciate the significant opportunities in their lives. The four primary domains of QoL, as per "engaged theory," are politics, economy, culture, and ecology.[23] The concept of quality of life, or QoL, is becoming more widely recognized as a crucial indicator of how a disease impacts a patient's life, particularly in the case of chronic illnesses like chronic kidney disease (CKD). Uncertainty surrounds the appropriate metrics for evaluating the quality of life (QOL) of individuals with chronic kidney disease (CKD). QOL assessments might be generic or disease-specific, functional or satisfaction-based, subjective or objective. Differential perception of quality of life (QOL) may be influenced by a number of factors, including age, ethnic or national background,and stage of CKD, type of dialytic therapy, exercise interventions, pain, erectile dysfunction, sleep disturbances, depressive affect, symptom burden, and perception of intrusiveness of illness. An essential indicator of how a condition impacts a patient's life is their health-related quality of life, or QOL.[24]
STATUS OF QUALITY OF LIFE IN CKD PATIENTS
Chronic kidney disease (CKD) patients have a lower quality of life (QoL) as a result of their high symptom burden and treatment requirements.[29]
Assessments of a patient's functional status and subjective well-being in relation to their health condition, commonly referred to as health-related quality of life (HRQoL) measurements, are important for patients with chronic kidney disease (CKD), including those with end-stage renal disease (ESRD). Patients' health-related quality of life (HRQoL) has an impact on various aspects of their lives, such as when dialysis is started, whether they continue to work despite developing renal failure, and if they continue to be involved in their community and home.The primary concern for patients with chronic kidney disease (CKD) has been low quality of life (QoL), and its onset may impede the course of CKD. Individuals diagnosed with chronic kidney disease (CKD) experience reduced quality of life (QoL), increased symptoms, and increased psychological distress. The extent of these changes is negatively correlated with GFR. Particularly for patients with advanced chronic kidney disease (CKD), health-related quality of life is a metric that is becoming more and more important for evaluating the efficacy of treatments for chronic illnesses. When making medical decisions that take into account a patient's physical, social, and emotional needs, the patient's subjective judgments of the disease are crucial. This decline in HRQoL is caused by a number of variables, including as poor nutrition, anemia, cognitive decline, depression, sleep disorders, apathy, decreased sexual and physical functioning, and co-morbidities like diabetes, hypertension, and cardiovascular diseases.[30]
ROLE OF PHARMACIST IN DIALYSIS
- Pharmacists play a significant role as members of a patient's healthcare team in a variety of settings.
- They are experts in identifying possible drug interactions, laboratory monitoring, adjusting drug dosage, creating monitoring plans, avoiding nephrotoxic drugs, and managing kidney disease complications. [31]
- Multiple pharmaceutical regimens are provided to patients with end-stage renal disease in order to treat their complex disease conditions. They are more likely to experience medication-related issues as a result. Because of their training in pharmacotherapy, pharmacists are qualified to deal with issues relating to medications.[32]
- Pharmacist plays a crucial role in patients with poor CKD related health literacy, improve their CKD awareness and self- management skills.
- Pharmacist check errors in prescription, inappropriate prescription results in adverse drug events and unwanted patient outcome.
- Pharmacist access nephrologist for the specialist services.
- Pharmacist provide information regarding health care insurance plans to reduce the burden of health care cost.
- Pharmacist provide patient counselling by supplying the patient or his or her representative with written or verbal drug information that includes usage instructions, advice on side effects, storage, precautions, and dietary and lifestyle changes. [37]
CONCLUSION
Chronic kidney failure is a significant global health concern with a steadily increasing prevalence. Dietary control is a crucial aspect of managing CKD and itsimpact on disease progression and quality of life. The population often experiences disturbances in mineral metabolism, such as hyperphosphatemia and hypocalcemia. Which contribute markedly to pain and discomfort. Effective management of these imbalances through tailored medical interventions and dietary adjustments is essential to alleviate pain and enhance the overall well-being of these patients. Additionally, comprehensive pain management strategies, including both pharmacological and non-pharmacological approaches, should be integrated into the care plan to address the multifaceted nature of pain in this patient group. By prioritizing the correction of mineral imbalances and adopting a holistic approach to pain management, healthcare providers can substantially improve the quality of life for CKD patients on hemodialysis.
CONFLICT OF INTEREST
There are no disclosed conflicts of interest for the authors. The manuscript's contents have been reviewed by all co-authors, who concur with its contents and have no financial interests to disclose. We confirm that the submission is our original work and isn't being considered for publication by another Journal
REFERENCE
- Mora J, Tarrab R, Martuscelli J, Soberón G. Characteristics of arginases from ureotelic and non-ureotelic animals. Biochem J. 1965 Sep;96(3):588-94. doi: 10.1042/bj0960588. PMID: 5862400; PMCID: PMC1207192.
- K Sembulingam, PremaSembulingam. Essentials of medical physiology. New Delhi: Jaypee Brothers Medical Publishers; 2013.
- Klahr S, Miller SB. Acute Oliguria. New England Journal of Medicine. 1998 Mar 5;338(10):671–5.
- Ingelfinger FJ. Dorlands medical dictionary. Philadelphia ; London ; Toronto: W.B. Saunders; 1980.
- Kasper DL. Harrison’s principles of internal medicine. New York: Mcgraw Hill Education Medical; 2015.
- Grauer GF. Proteinuria: Measurement and Interpretation. Topics in Companion Animal Medicine. 2011 Aug;26(3):121–7.
- Singh P, Nayak B, Sridhar Panaiyadiyan. A Guide to Management of Urological Cancers. Springer Nature; 2023.
- Leslie SW, Sajjad H, Murphy PB. Renal Calculi [Internet]. Nih.gov. StatPearls Publishing; 2019. Available from: https://www.ncbi.nlm.nih.gov/books/NBK442014/
- Brandes SB, Morey AF. Advanced male urethral and genital reconstructive surgery. New York: Humana Press; 2014.
- Bidani AK, Griffin KA, Williamson G, Wang X, Loutzenhiser R. Protective Importance of the Myogenic Response in the Renal Circulation. Hypertension. 2009 Aug;54(2):393–8.
- Hamrahian SM, Falkner B. Hypertension in chronic kidney disease. Advances in Experimental Medicine and Biology. 2017;956:307–25.
- Olechnowicz-Tietz S, Gluba A, Paradowska A, Banach M, Rysz J. The risk of atherosclerosis in patients with chronic kidney disease. International Urology and Nephrology. 2013 Mar 13;45(6):1605–12.
- Chen W, Abramowitz MK. Treatment of Metabolic Acidosis in Patients With CKD. American Journal of Kidney Diseases. 2014 Feb;63(2):311–7.
- Hamlin L, Davies M, Richardson-Tench M. Perioperative nursing : an introductory text. Australia: Taylor & Francis; 2009.
- iasppain.org [Internet]. ww12.iasppain.org. [cited 2024 May 22]. Available from: http://www.iasppain.org/Content/NavigationMenu/GeneralResourceLinks/PainDefinitions/defa
- Joshi GP, Kehlet H, Beloeil H, Bonnet F, Fischer B, Hill A, et al. Guidelines for perioperative pain management: need for re-evaluation. British Journal of Anaesthesia. 2017 Oct;119(4):720–2.
- Vadivelu N, Mitra S, Hines R, Elia M, Rosenquist RW. Acute Pain in Undergraduate Medical Education: An Unfinished Chapter! Pain Practice. 2012 Jun 20;12(8):663–71.
- Vermeire S, Audenaert K, De Meester R, Vandermeulen E, Waelbers T, De Spiegeleer B, et al. Serotonin 2A receptor, serotonin transporter and dopamine transporter alterations in dogs with compulsive behaviour as a promising model for human obsessive-compulsive disorder. Psychiatry Research: Neuroimaging. 2012 Jan;201(1):78–87.
- Delgado DA, Lambert BS, Boutris N, McCulloch PC, Robbins AB, Moreno MR, et al. Validation of Digital Visual Analog Scale Pain Scoring with a Traditional Paper-based Visual Analog Scale in Adults. JAAOS: Global Research and Reviews [Internet]. 2018 Mar;2(3):e088. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6132313/
- Shrimanker I, Bhattarai S. Electrolytes [Internet]. Nih.gov. StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK541123/
- Vanholder R, Gryp T, Glorieux G. Urea and Chronic Kidney disease: the Comeback of the century? (in Uraemia research). Nephrology Dialysis Transplantation [Internet]. 2017 Apr 12;33(1):4–12. Available from: https://academic.oup.com/ndt/article/33/1/4/3605326
- Teoli D, Bhardwaj A. Quality Of Life [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536962/
- Kefale B, Alebachew M, Tadesse Y, Engidawork E. Quality of life and its predictors among patients with chronic kidney disease: A hospital-based cross sectional study. Cheungpasitporn W, editor. PLOS ONE. 2019 Feb 27;14(2):e0212184.
- Kimmel PL. The Weather and Quality of Life in ESRD Patients: Everybody Talks About it, But Does Anybody Do Anything About it? Seminars in Dialysis. 2013 Feb 14;26(3):260–2.
- Perlman RL, Finkelstein FO, Liu L, Roys E, Kiser M, Eisele G, et al. Quality of life in Chronic Kidney Disease (CKD): A cross-sectional analysis in the Renal Research Institute-CKD study. American Journal of Kidney Diseases [Internet]. 2005 Apr 1 [cited 2021 Jan 12];45(4):658–66. Available from: https://www.sciencedirect.com/science/article/pii/S0272638605000053
- Gounden V, Jialal I. Renal Function Tests [Internet]. National Library of Medicine. StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507821/
- Creatinine Test [Internet]. Testing.com. 2021 [cited 2024 May 22]. Available from: https://labtestsonline.org/understanding/analytes/creatinine/tab/glance
- National Kidney Foundation. What is dialysis? [Internet]. National Kidney Foundation. 2018. Available from: https://www.kidney.org/atoz/content/dialysisinfo
- Health-Related Quality of Life in People Across the Spectrum of CKD. Kidney International Reports [Internet]. 2020 Dec 1;5(12):2264–74. Available from: https://www.sciencedirect.com/science/article/pii/S2468024920315448
- Sharma S, Kalra D, Rashid I, Mehta S, Maity MK, Wazir K, et al. Assessment of Health-Related Quality of Life in Chronic Kidney Disease Patients: A Hospital-Based Cross-Sectional Study. Medicina [Internet]. 2023 Oct 1 [cited 2023 Dec 3];59(10):1788. Available from: https://www.mdpi.com/1648-9144/59/10/1788
- Braund R. Renal medicine and clinical pharmacy. Cham: Springer; 2020.
- Daifi C, Feldpausch B, Roa PA, Yee J. Implementation of a Clinical Pharmacist in a Hemodialysis Facility: A Quality Improvement Report. Kidney Medicine [Internet]. 2021 Mar 1 [cited 2023 Apr 19];3(2):241-247.e1. Available from: https://www.sciencedirect.com/science/article/pii/S2590059521000170
- Hosten AO. BUN and Creatinine [Internet]. National Library of Medicine. Butterworths; 1990. Available from: https://www.ncbi.nlm.nih.gov/books/NBK305/
- Visual Analog Survey Scale -- A Pain-ful Misnamed Scale [Internet]. Great Brook Consulting. 2019. Available from: https://greatbrook.com/visual-analog-survey-scale/
- Ismail S, Al-Subhi A, Youssif E, Ahmed M, Almalki A, Seger DL, et al. Patient-centered Pharmacist Care in the Hemodialysis Unit: a quasi-experimental interrupted time series study. BMC nephrology [Internet]. 2019 Nov 13 [cited 2024 Mar 15];20(1):408. Available from: https://pubmed.ncbi.nlm.nih.gov/31722680/
- Gounden V, Jialal I. Renal Function Tests [Internet]. National Library of Medicine. StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507821/
- Thomas D, Joseph J, Francis B, P. Mohanta G. Effect of patient counseling on quality of life of hemodialysis patients in India. Pharmacy Practice (Internet). 2009 Sep;7(3).
- Excretory system [Internet]. Wikipedia. 2024 [cited 2024 May 24]. Available from: https://en.wikipedia.org/wiki/Excretory_system#References.
- Excretory system [Internet]. Wikipedia. 2024. Available from: https://en.wikipedia.org/wiki/Excretory_system#References
- Lote CJ. Principles of Renal Physiology. New York, Ny: Springer New York; 2012.
- Goyal A, Daneshpajouhnejad P, Hashmi MF, Bashir K. Acute Kidney Injury (Acute Renal Failure) [Internet]. PubMed. Treasure Island (FL): StatPearls Publishing; 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK441896/
- Vaidya SR, Aeddula NR. Chronic Kidney Disease [Internet]. Nih.gov. StatPearls Publishing; 2022. Available from: https://www.ncbi.nlm.nih.gov/books/NBK535404/
- Karageorgos FF, Stavros Neiros, Konstantina-Eleni Karakasi, Vasileiadou S, Katsanos G, Antoniadis N, et al. Artificial kidney: Challenges and opportunities. World journal of transplantation [Internet]. 2024 Mar 18 [cited 2024 Apr 18];14(1). Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10989479/#:~:text=An obvious shortcoming of the
- McGill RL, Weiner DE. Dialysate Composition for Hemodialysis: Changes and Changing Risk. Seminars in dialysis [Internet]. 2017 Mar 1 [cited 2021 Oct 2];30(2):112–20. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7645386/
- Peritoneal dialysis [Internet]. Wikipedia. 2024 [cited 2024 May 24]. Available from: https://en.wikipedia.org/wiki/Peritoneal_dialysis#cite_note-1
- States. U, States. U. Kidney Diseases: a Guide for Public Health Personnel. 1967


 V. J Dawn* 2
V. J Dawn* 2
 10.5281/zenodo.11491103
10.5281/zenodo.11491103