Abstract
Atopic dermatitis, commonly known as eczema, is a chronic inflammatory skin condition affecting millions worldwide. Characterized by itching, redness, and dryness, it significantly reduces quality of life and often requires long-term management. Conventional treatments such as corticosteroids, antihistamines, and immunosuppressants offer symptomatic relief but pose risks including side effects, dependency, and high costs. As a result, interest in herbal alternatives has increased due to their safety and potential efficacy.Neem (Azadirachta indica) and Aloe vera (Aloe barbadensis miller) are recognized for their antibacterial, anti-inflammatory, and skin-soothing properties, making them suitable candidates for eczema treatment. This study aims to formulate and evaluate a neem and aloe vera-based emulgel by leveraging emulgel technology, which combines the benefits of emulsions and gels to enhance drug stability, penetration, and ease of application.The formulation process involved optimizing ingredient concentrations and assessing various physicochemical properties, including pH, viscosity, spreadability, and in-vitro drug release. Additional evaluations were conducted to assess skin irritation potential and product stability under different environmental conditions.Preliminary findings suggest that the neem-aloe vera emulgel demonstrates favorable stability, good skin retention, and potential therapeutic benefits for eczema management. By addressing the limitations of traditional therapies, this formulation offers a safer, cost-effective, and natural alternative for dermatological use. However, further studies and clinical trials are necessary to confirm its long-term safety and therapeutic effectiveness.
Keywords
Emulgel, Neem (Azadirachta indica), Aloe Vera (Aloe barbadensis miller), Eczema, and Atopic Dermatitis Natural therapy, topical treatment, anti-inflammatory, skin barrier, drug delivery, herbal formulation, and dermatology.
Introduction
1] Overview of Eczema: Also known as atopic dermatitis, eczema is a chronic inflammatory skin disorder characterized by dryness, redness, swelling, and itching. (1) It is associated with an overactive immune response and a compromised skin barrier, and it frequently manifests in recurrent episodes with acute flare-ups. Although it affects people of all ages, children are most affected. (2) The quality of life for people who are impacted can be severely reduced by its enduring symptoms.(3)
2] Limitations of Conventional Treatments: Topical corticosteroids, emollients, and antihistamines are commonly used to treat eczema. (4)Prolonged use of corticosteroids can result in side effects, including as skin thinning, inflammation, and hormone imbalances, even while these treatments are successful in treating symptoms and flare-ups.(5) In addition, the oily texture, disagreeable odor, and irritability of many synthetic medications are linked to poor patient compliance.(6) These difficulties underscore the need for safer, more efficient, and more user-friendly alternative therapeutic procedures.(7)
3] Advantages of Using Herbal Medicines to Treat Eczema:
For millennia, people have employed herbal medicines to treat a variety of skin ailments. Bioactive substances with anti-inflammatory, antibacterial, and antioxidant qualities, such as flavonoids, alkaloids, and polyphenols, are abundant in these natural remedies. Herbal formulas minimize side effects and promote skin healing while providing a natural and holistic approach to treating eczema. Of the many therapeutic plants, aloe vera (Aloe barbadensis miller) and neem (Azadirachta indica) have shown great promise in treating skin conditions. (8)
4] Benefits of Neem and Aloe Vera for Therapeutic Use:
Neem: Commonly known as the "miracle tree," neem is well-known for its antibacterial, antifungal, and anti-inflammatory properties. Nimbin, Nimbolide, and Quercetin are among its active ingredients; they help soothe irritated skin, reduce inflammation, and fight against microbial infections that are frequently linked to eczema.
Aloe Vera: Aloe very is well known for its ability to promote healing, soothe, and hydrate. It has vital vitamins, polysaccharides, and glycoproteins that reduce redness, encourage cell regeneration, and repair the skin barrier. Neem and aloe versa work together to treat eczema in a way that tackles multiple facets of the underlying causes of the condition. (9)
5] The Significance of Emulgel Production:
A cutting-edge topical delivery technology that combines the advantages of gels and emulsions is called Emulgel. Because of its non-greasy texture and simplicity of use, this formulation guarantees increased stability, better medication penetration, and increased patient compliance. By encouraging improved absorption and prolonged release of active ingredients, neem and aloe vera can be added to an emulgel to increase therapeutic efficacy. This cutting-edge delivery method presents a viable substitute for successfully treating eczema.(10)
7] Neem (Azadirachta indica) in Eczema Management:
Using Neem (Azadirachta indica) to Treat Eczema
Rich in bioactive substances like nimbidin, azadirachtin, and flavonoids, neem is a significant Ayurvedic medicinal plant that offers Benefits of anti-inflammatory Decreases inflammation by lowering cytokine activity (TNF-α, IL-6). Antibacterial and antifungal qualities: especially strong against Staphylococcus aureus, a pathogen frequently linked to flare-ups of eczema. Effects of skin regeneration: Promotes wound healing by stimulating keratinocyte proliferation.
Scientific Proof in Favor of Neem
In a clinical experiment with 80 people, neem leaf extract decreased eczema symptoms by 45%, according to a 2020 study published in the Journal of Ethnopharmacology. A study that was published in Phytotherapy Research in 2021 showed that neem oil formulations sped up the healing of wounds in inflammatory skin disorders by 60%.(11)
8. Aloe Vera in Ezcema Management:
A natural skin hydrator and healer, aloe Vera is prized for its calming, anti-inflammatory, and hydrating qualities. Among its constituents are polysaccharides (acemannan), which promote fibroblast activity and facilitate wound healing.
As antioxidants, vitamins A, C, and E shield the skin from oxidative damage. Bradykinase is an enzyme that aids in lowering inflammation and itching. Scientific Proof in Favor of Aloe Vera
Aloe vera gel reduced the severity of eczema by 52% in just four weeks, according to a 2019 study that was published in the Journal of Dermatological Treatment. Aloe vera-based lotions increased skin hydration and barrier function by 70% in atopic dermatitis patients, according to a 2021 study published in the Indian Journal of Dermatology. (12)

Fig 1: Neem & Aloe Vera Powder
History
Several traditional medical systems have acknowledged eczema, a chronic skin condition characterized by inflammation, itching, and dryness, for ages. (13) Using detoxifying herbal formulations, Traditional Chinese Medicine (200 BCE) linked eczema to "damp-heat" imbalances, while Ayurveda defined eczema as Vicharchika and recommended neem and turmeric for their antibacterial and anti-inflammatory qualities.(14) Aloe vera has been prized for its ability to treat skin for more than 4,000 years. The ancient Egyptians referred to it as the "Plant of Immortality" and used it frequently for wound healing, calming, and hydrating. Aloe vera (Kumari) was used in Ayurveda to treat inflammatory skin disorders, and current research confirms its anti-inflammatory, moisturizing, and skin barrier-repairing properties. (15) The Atharva Veda refers to neem (Azadirachta indica), which has been used in Ayurveda for over 5,000 years, as Sarva Roga Nivarini, or "a remedy for all diseases." Neem has long been used to treat eczema, inflammation, and skin infections; however, its antibacterial, antifungal, and skin-rejuvenating qualities have recently been acknowledged by science.(16) Emulgel technology, which combines emulsion with gel for better penetration, longer release, and increased stability of active ingredients, was developed in the 21st century as a result of advancements in drug delivery(17) Because of their superior absorption, lightweight structure, and prolonged therapeutic action, herbal emulgels have become a more effective alternative to earlier herbal formulations that mostly depended on oils and basic gels..(17) Because of their superior absorption, lightweight structure, and prolonged therapeutic action, herbal emulgels have become a more effective alternative to earlier herbal formulations that mostly depended on oils and basic gels. (18) Emulgel made from neem and aloe vera are currently being studied as a natural, secure, and efficient substitute for traditional steroid-based treatments for eczema.(19)
Need Of Study
Need of Study:
1. Addressing the Limitations of Conventional Eczema Treatments:
Side Effects of Corticosteroids: Conventional treatments for eczema often rely on topical corticosteroids, which can have significant local and systemic side effects with prolonged use, including skin thinning, striae, telangiectasia, and potential systemic absorption.(20)
Lack of Long-Term Solutions: Current treatments often manage symptoms rather than providing a long-term solution or addressing the underlying causes of eczema.(21)
Patient Dissatisfaction: Many patients are dissatisfied with the side effects and lack of sustained relief offered by conventional therapies, leading them to seek alternative or complementary approaches.(22)
2. Harnessing the Potential of Herbal Medicine:
Synergistic Effects: Polyherbal formulations, combining multiple medicinal plants, can offer synergistic therapeutic effects. Different herbs may target various aspects of eczema pathology, such as inflammation, itching, dryness, and skin barrier dysfunction, potentially leading to more comprehensive relief.(23)
Reduced Risk of Single-Drug Toxicity: Using a combination of herbs at lower concentrations may minimize the risk of toxicity associated with high doses of a single active pharmaceutical ingredient.(24)
Traditional Use and Safety Profile: Many herbs have a long history of traditional use for skin conditions, suggesting a degree of safety and efficacy. Scientific investigation can validate these traditional claims.(25)
3. Advantages of Emulgel as a Topical Drug Delivery System:
Dual Release Mechanism: Emulgels, which are emulsions incorporated into a gel base, offer a dual release mechanism. The emulsion component provides sustained release of lipophilic drugs, while the gel component offers good spreadability, skin feel, and potentially enhances drug penetration.(26)
Improved Patient Compliance: The non-greasy nature and ease of application of emulgels can improve patient compliance compared to traditional ointments or creams. (27)
Enhanced Drug Penetration: The presence of both oil and water phases in emulgels can facilitate the penetration of both hydrophilic and lipophilic herbal constituents through the skin barrier.(28)
Protection of Active Ingredients: The gel matrix can protect the herbal extracts from degradation due to environmental factors like oxidation and light. (29)
4. Scientific Validation and Standardization:
Evidence-Based Approach: Rigorous scientific evaluation of polyherbal emulgels is necessary to validate their efficacy and safety through in vitro and in vivo studies.(30)
Standardization of Herbal Extracts: Formulation studies should focus on the standardization of herbal extracts to ensure batch-to-batch consistency in the concentration of active constituents, leading to predictable therapeutic outcomes. (31)
Quality Control: Evaluation parameters will help establish quality control standards for the developed formulation, ensuring its stability, homogeneity, and appropriate physicochemical properties.(32)
5. Exploring Novel Therapeutic Options:
Addressing the Multifactorial Nature of Eczema: Eczema is a complex condition influenced by genetic, environmental, and immunological factors. Polyherbal formulations may offer a multi-pronged approach by targeting different pathways involved in its pathogenesis.
Potential for Cost-Effectiveness: Herbal remedies, if proven effective and safe, could potentially offer a more affordable treatment option, especially in resource-limited settings. In conclusion, the study of the evaluation and formulation of a topical polyherbal emulgel for the treatment of eczema is essential for developing a safe, effective, and potentially more sustainable alternative to conventional therapies. It allows for the scientific validation of traditional knowledge, harnesses the synergistic potential of multiple herbs, utilizes an advantageous drug delivery system, and contributes to expanding the therapeutic options available for managing this chronic and often debilitating skin condition. (33)
Aim & Objective
Aim:
To Formulation & Evaluation of Topical Polyherbal Emulgel for Treatment of Eczema
Objectives
- To identify and select medicinal plants traditionally used or scientifically proven to possess anti-inflammatory, anti-pruritic (anti-itch), and skin-healing properties relevant to eczema treatment.
- To authenticate the selected plant materials studies
- To prepare extracts from the selected plant materials using Soxhlet extraction techniques.
- To perform preliminary phytochemical screening of the prepared extracts to identify the presence of key bioactive constituents.
- To formulate a stable oil-in-water (o/w) or water-in-oil (w/o) emulgel incorporating the prepared polyherbal extract(s) at different concentrations.
- To optimize the formulation by varying the concentrations of gelling agents, emulsifiers, penetration enhancers, and preservatives to achieve desired physicochemical properties.
- To Evaluate of Physicochemical Properties of the Emulgel
- To evaluate the physical and chemical stability of the optimized emulgel formulation (34)
Plan Of Study
1. Literature Review
Study of eczema, herbal remedies, and emulgel formulations.
2. Selection of Herbal Ingredients
Based on anti-inflammatory, antimicrobial, and skin-healing properties.
3. Extraction of Herbal Actives
Using suitable methods like maceration or Soxhlet extraction.
4. Pre-formulation Studies
Evaluation of extract properties (solubility, compatibility, etc.).
5. Formulation of Emulgel
Preparation of emulsion base and incorporation into gel.
6. Evaluation of Emulgel
Physical appearance, pH, viscosity, spreadability, extrudability, stability.
7. Conclusion Summary
Drug Profile
1] Neem (Azadirachta indica): -
Drug name: Neem
Biological name: Azadirachta indica
Species: Azadirachta indica
Family: Meliaceae

Fig 2: Neem Powder
Uses:
1) Antibacterial, antifungal, antiviral and anti-inflammatory properties
2) To treat skin disorder fever and digestive issue
3) Purify blood and boost immunity
4) Natural toothbrushes
5) Prevent cavities and gum infection (35)
2) Aloe :( Aloe vera): -
Drug Name: Aloe vera
Biological name: Aloe Barbedensis miller
Species: Aloe vera
Family: Asphodelaceae / Liliaceae

Fig 3: Aloe Vera Powder
Uses:
1) To treat heals wounds, burns and cuts and anti-inflammatory
2) Digestive disorder E.g. Reflux
3) Boost immunity and act as antioxidant
4) It promotes the hair growth
5) Sunscreen and anti-aging creams (36)
MATERIAL AND METHOD
1. Material: (37)
A] Apparatus: Condenser, Soxhlet Apparatus, round bottom flask, Water bath, Mortal & pastel
B] Chemical:
1. Neem Powder extract
2. Aloe Vera Powder extract
3. Methyl paraben
4. Carbapol934
5 Propyl paraben
6. Propylene glycol
7.Almoned oil
8.Tween 20
9.Triethalamine
10. Water
Table 1: Formulation Table:
|
Sr.no
|
Ingredient name
|
F1
|
F2
|
Role
|
|
1
|
Neem powder extract (ml)
|
2
|
3
|
Active Pharmaceutical Ingredient
|
|
2
|
Aloe Vera Powder extract (ml)
|
2
|
3
|
Active Pharmaceutical Ingredient
|
|
3
|
Carbopol 934(mg)
|
4000
|
6000
|
Gelling agent
|
|
4
|
Propylene glycol (ml)
|
5
|
5
|
Humectant
|
|
5
|
Propyl paraben (mg)
|
0.01
|
0.01
|
Preservative
|
|
6
|
Methyl paraben (mg)
|
0.03
|
0.03
|
Preservative
|
|
7
|
Almond oil (ml)
|
6
|
7
|
Oil Phase
|
|
8
|
Triethanolamine (ml)
|
1.2
|
1.2
|
Neutralizing Agent
|
|
9
|
Tween 80 (ml)
|
0.5
|
0.5
|
Emulsifying agent
|
|
10
|
Water
|
Q. S
|
Q. S
|
Solvent
|

Fig 4: Material Used for Preparation Emulgel
2. Method: (37)
1] Extraction of neem by using Soxhlet apparatus:
Take a 50-gm powder and get extract with 250 ml methanol and take 14 cycles Are performed.

Fig 5: Extraction Process
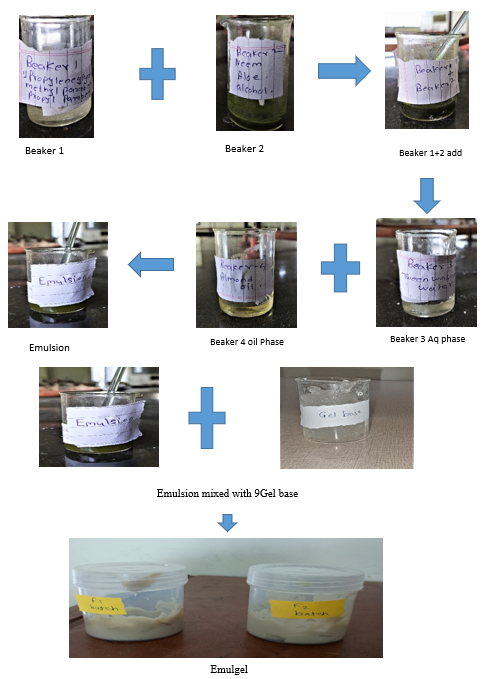
2] Preparation of Emulsion:


3] Preparation of Gel
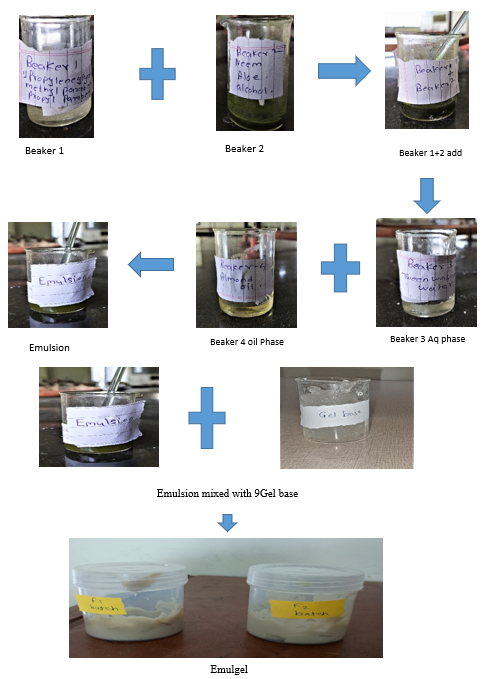
4] Preparation of Emulgel:
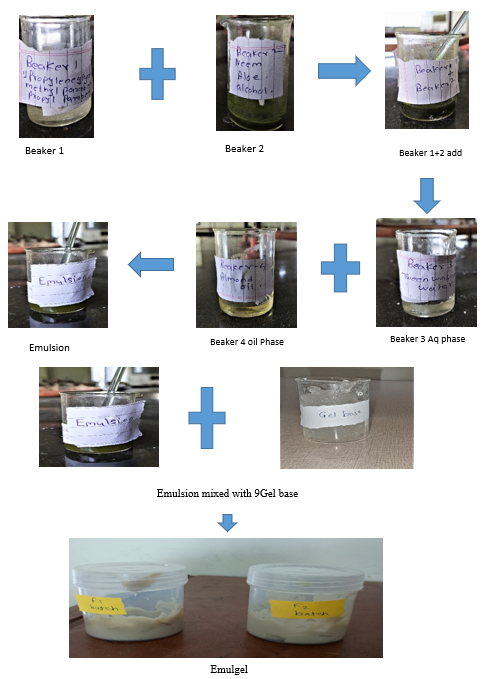
Fig 6: Procees of Emulgel Preparation
Evaluation Of Emulgel
A] Pre formulation study
A] Pre-formulation analysis
I] Phytochemical Examination (38)
1] Molish's Test: Add 2 ml of extracts to 2 ml of Molish's reagent and mix thoroughly. To this, two milliliters of concentrated sulfuric acid were cautiously introduced via the test tube's side.
A raddish violet ring appears where the layers converge.
2] Tannin Test: A few drops of a 10% ferric chloride solution were added to the extracts.The presence of tannins is indicated by a green or blue appearance.
3] Steroid Test: 1 ml of chloroform was combined with leaf extracts, and two to three drops of concentrated H2SO4 were added. Look Steroids are indicated by a pink or read color.
4] Terpenoid Test (Salkowiski Test): 5 ml of the extracts were combined with 3 ml of concentrated H2SO4 solution and 2 ml of chloroform. The presence of terpenoids is indicated by a raddish brown color at the interphase.
5] Alkaloid Test (Mayer's Test): Mayer's reagent (potassium mercuric chloride) was applied to the extracts. The presence of alkaloids is indicated by the formation of a yellow precipitate.
6] Flavonoid Test: After treating the extract with concentrated H2SO4, a yellowish orange hue developed. shows that there are flavonoids present.
7] Protein Test (Xanthoprotein Test): 20% NaOH solution was added to the leaf extracts, and the development of an orange hue indicates the presence of proteins, which is indicative of ammonium production.
8] Cardiac Glycoside Test (Keller-Killani Test): Two milliliters of glacial acetic acid containing two to three drops of ferric chloride solution and one milliliter of concentrated H2SO4 solution were added to five milliliters of test extracts. The presence of cardiac glycosides is indicated by the initial appearance of a green ring that changes to violet and eventually brown during the interphase.
9] Fixed Oil Test: Two drops of extract were forced between two filter sheets. The presence of cardiac glycoside is shown by the appearance of an oil strain on the filter paper.
10] Saponins (Foam Test): Two milliliters of the extracts were mixed with twenty milliliters of distilled water, agitated briskly, and checked for a stable, long-lasting foam.
11] Ferric Chloride Test For Phenolic Compounds: Two millilitres of diluted extract were subjected to a dil.FeCL3 solution. The presence of phenol-like chemicals is indicated by a violet appearance.
12] Coumarin Detection: A few drops of alcoholic sodium hydroxide solution were added to the test solution. The presence of chemicals that resemble phenol is indicated by a violet appearance.
13] Test For Amino Acids (Ninhydrin Test): Two milliliters of aqueous filtrates were mixed with two drops of ninhydrin solution (10 mg of ninhydrin in 200 milliliters of acetone). The presence of amino acids is indicated by a distinctive purple color.
14] Gum And Mucilage Test: Add 10 ml of distilled water to 100 ml of each extract. With continuous staring, 25 milliliters of pure alcohol were added to this. Gum and mucilage are present when a hazy precipitate appears.

Fig 7: Phytochemical Test
II] Solubility Study: The amount of solvent needed to dissolve a given amount of solute is the basis for classifying solubility. The standard classifications are listed below. (30)
Tabel no 2: Solubility Study
|
Descriptive Term
|
Parts of solvent required per 1 Part solute
|
Concentration Range (mg/ml)
|
|
Very soluble
|
<1 part
|
>100 mg/ml
|
|
Freely Soluble
|
1-10 parts
|
10-100 mg/ml
|
|
Sparingly Soluble
|
10-30 parts
|
1-10 mg /ml
|
|
Slightly soluble
|
30-100 Parts
|
0.1-1 mg/ml
|
|
Very Slightly Soluble
|
100-1000 Parts
|
0.01-0.1 mg/ml
|
|
Practically Insoluble
|
>1000 parts
|
<0.01 mg/ml
|
Experimental Method for Determining Neem Extract's Solubility in Almond Oil:
1. Saturated Solution Preparation: A set volume (such as 2 mL) of almond oil was mixed with an excess of neem extract.
To facilitate solubility, the mixture was heated to 40°C and then constantly agitated.
To guarantee full saturation, the solution was left to equilibrate at 40°C for a whole day.
2. Separation of Undissolved Material: A clear saturated solution was obtained by centrifuging the sample for 10 minutes at 3000 rpm and then filtering it to get rid of any undissolved material.
3. UV-Vis Spectrophotometry Quantitative Analysis: Several standard neem extract solutions in almond oil were made at known concentrations.
Method for Building a Calibration Curve:
1. Standard Solution Preparation: Make solutions of neem extract in almond oil at various known concentrations (0.1, 0.2, 0.3, 0.4, and 0.5 mg/mL, for example).
Stirring and, if needed, gentle heating will guarantee that the extract is completely dissolved in the almond oil.
2. Absorbance Measurement: Determine each solution's absorbance at the neem extract's λmax (maximum absorbance wavelength) using a UV-visible spectrophotometer.
To calibrate the device, use a blank of pure almond oil.
3. Plotting the Calibration Curve: Show the absorbance on the Y-axis and the concentration (mg/mL) on the X-axis.
4. Assessing Solubility: Calculate the saturated solution's absorbance after filtering out any neem extract that hasn't dissolved.
To determine the solubility, solve for concentration using the calibration curve equation.
B] Post Formulation Study: (37)
1. Colour: An emulgels colour is a crucial physical attribute that offers essential information about its quality. A number of criteria are carefully evaluated during evaluation, including uniformity, stability, and potential discolouration.
2. Odor: Sensory evaluation can be used to gauge Odor.
3. Reliability:
Since consistency affects the physical state, texture, and flow characteristics of emulgels, it is a crucial evaluation metric. These characteristics have a big influence on the product's overall usability and efficacy.
4. Uniformity:
The active pharmaceutical ingredient (API) and emulsifying agents should be distributed evenly throughout an emulgel formulation to ensure consistency. Inconsistent drug release, decreased effectiveness, and potential safety issues might result from a lack of homogeneity.
5. Appearance:
One of the most important quality indicators of an emulgel is its overall look, which includes its color, transparency, texture, and aesthetic appeal. The product's commercial success, user satisfaction, and consumer perception are all impacted by its aesthetic qualities.
6. Greasiness:
An important consideration in the formulation of emulgel is greasiness. Emulgels should be quickly absorbed, have a non-greasy texture, and not leave the skin feeling greasy. While maintaining the intended therapeutic advantages, proper formulation modifications can improve user comfort.
7. Washability:
One important consideration when evaluating emulgels is washability. When washed, the perfect emulgel should leave little residue and be easily removed with water. Emulgels can offer a successful cleansing experience that keeps the skin clean and renewed by refining the formulation and guaranteeing compatibility with cleansing agents.
8. Extrudability:
The ease with which an emulgel can be forced out of a tube or container under pressure is known as extrudability. It is a crucial factor in cosmetics and pharmaceuticals that influences dose accuracy and consumer ease.
9. Test of Tube Extrudability:
Take an emulgel-filled collapsible tube. Put pressure on it continuously. Determine how much emulgel was extruded by weight or in seconds.
10. pH
1. To ensure skin compatibility, an emulgel's pH should preferably fall between 5 and 7. An too basic or acidic composition may irritate skin.
2. A digital pH meter is used to measure the prepared emulgel's pH.
3. A pH meter is used to record the pH reading.
11. Spreadability:
When evaluating an emulgel's ease of application, Spreadability is a crucial consideration.
One gram of the emulgel is put on a petri plate, and another petri plate is set on top of it to test Spreadability. After that, a 50-gram weight is placed on top for 60 seconds. To achieve an appropriate assessment, the spread emulgel's diameter is measured three times after this period and the average value is computed.
12. Viscosity:
Viscosity is a crucial parameter in evaluating emulgels, as it affects their stability, spreadability, and overall application properties.11. The ability to spread When evaluating an emulgel's ease of application, spreadability is a crucial consideration. One gram of the emulgel is put on a petri plate, and another petri plate is set on top of it to test spreadability. After that, a 50-gram weight is placed on top for 60 seconds. To achieve an appropriate assessment, the spread emulgel's diameter is measured three times after this period and the average value is computed.
13. Antimicrobial Test:
The antimicrobial activity of the emulgel is assessed through the agar well diffusion method, targeting two bacterial strains:
Gram-positive: Staphylococcus aureus (S. aureus)
Gram-negative: Escherichia coli (E. coli)
Method:

RESULT & DISCUSSION
A] Pre formulation study
I] Phytochemical Test
Table 3: Phytochemical Test
|
Sr
|
Test
|
Result
|
|
1
|
Molish’s Test:
|
+
|
|
2
|
Test For Tannins:
|
+
|
|
3
|
Test For Steroids:
|
+
|
|
4
|
Test For Terpenoids (Salkowiski Test):
|
+
|
|
5
|
Test For Alkaloids (Mayer’s Test):
|
+
|
|
6
|
Test For Flavonoids:
|
+
|
|
7
|
Test For Proteins (Xanthoprotein Test):
|
+
|
|
8
|
Test For Cardiac Glycosides (Keller-Killani Test):
|
+
|
|
9
|
Test For Fixed Oils:
|
+
|
|
10
|
Test For Saponins (Foam Test):
|
+
|
|
11
|
Test For Phenolic Compounds (Ferric Chloride Test)
|
+
|
|
12
|
Detection Of Coumarins:
|
+
|
|
13
|
Test For Amino Acids (Ninhydrin Test):
|
+
|
|
14
|
Test For Gum and Mucilage:
|
+
|
II] Solubility Study:
Table 4: Solubility Study
|
Concentration (mg/ml)
|
Absorbance
|
|
0.1
|
0.10
|
|
0.2
|
0.21
|
|
0.3
|
0.31
|
|
0.4
|
0.41
|
|
0.5
|
0.52
|

Fig :8 Solubility Study for neem extract

Fig 9: Calibration curve for Solubility study
Result: Freely soluble
B] Post Formulation Study:
Table 5: Evaluation Of Emulgel
|
Sr.
|
Parameter
|
Method of evaluation
|
F1
|
F2
|
|
1
|
Color
|
Visual inspection
|
Light greenish white
|
Greenish white
|
|
2
|
Odor
|
Sensory evaluation
|
Characteristics
|
Characteristics
|
|
3
|
Consistency
|
Visual inspection
|
Uniform
|
Uniform
|
|
4
|
Homogeneity
|
Visual inspection
|
Good
|
Good
|
|
5
|
Appearance
|
Visual inspection
|
Semi-solid
|
Semi-solid
|
|
6
|
Greasiness
|
Sensory evaluation
|
Non-greasy
|
Non-greasy
|
|
7
|
Washability
|
Water rinsing test
|
Washable
|
Washable
|
|
8
|
Extrudadility
|
Tube squeeze test
|
Easily Extrudable With slight pressure
|
Easily Extrudable With slight presure
|
|
9
|
pH
|
pH meter
|
5.9
|
6.5
|
|
10
|
Spreadability
|
Parallel plate method
|
3.6 .cm
|
2.8 .cm
|
|
11
|
Viscosity
|
Brookfield Viscometer
|
2044.9 pa.s
|
2049.8 pa.s
|
|
12
|
Antimicrobial Test
|
Agar diffusion method
|
Zone of inhibition S.aureus
|
Zone of inhibition
E.coli
|
Zone of inhibition S.aureus
|
Zone of inhibition
E.coli
|
|
30 mm
|
20 mm
|
15 mm
|
25 mm
|
|
13
|
Phase separation
|
Centrifugation (3000 rpm, 30 min )
|
No phase separation
|
No phase separation
|
|
14
|
Stability study
|
Storage
(3 month’s)
|
NO significant changes (PH, viscosity ,Color.)
|
NO significant changes (PH, viscosity ,Color.)
|

Fig :10 Extrudability Test of f1 Formulation
Fig: 11 Extrudability Test of f2 Formulation

Fig :12 Spreadability test For F1Formulation
Fig :13 Spreadability test for f2 Formulation

Fig 14 pH Test for F1 Formulation
Fig 15 pH Test for F2 Formulation

Fig: 16 Viscosity for f1 formulation
Fig: 17 Viscosity for f2 formulation

Fig: 18 Antimicrobial (S-Aureus) Test for f1 &f2Formulation
Fig: 19 Antimicrobial Test (E. coli) for f1 &f2Formulation

Fig: 20 Phase separation for f1&f2 Formulation

Fig: 21 Stability study for f1&f2 Formulation (0 day)
Fig: 22 Stability study for f1&f2 Formulation (3 Months)
CONCLUSION & SUMMARY
The polyherbal emulgel for eczema was successfully formulated and evaluated through pre-formulation, solubility, phytochemical, and post-formulation studies.
1. Pre-formulation & Phytochemical Tests
The phytochemical screening confirmed the presence of alkaloids, flavonoids, tannins, and saponins, indicating potential anti-inflammatory and antimicrobial properties. The solubility study showed that neem extract is sparingly soluble to slightly soluble in oil, emphasizing the need for emulsification to enhance drug dispersion.
2. Post-formulation Studies
The emulgels (F? & F?) exhibited uniform consistency, good homogeneity, and non-greasy texture. pH (5.9–6.3) was within the skin-compatible range. Spreadability was measured as 3.6 cm (F?) and 3.3 cm (F?), ensuring easy application. Viscosity (~2014-2049.8 mPa.s) indicated good stability and retention on the skin. Antimicrobial testing revealed significant inhibition against S. aureus (30 mm) and E. coli (20-25 mm), supporting its efficacy. No phase separation was observed, and the 3-month stability study showed no significant changes in pH, viscosity, or color.
Further Scope
Conduct in-vitro drug release studies to evaluate the release profile. Perform skin irritation and in-vivo efficacy studies to confirm safety and effectiveness. Optimize the emulsifier and gelling agent concentrations for improved formulation properties. Overall, the polyherbal emulgel is a stable, effective, and skin-friendly formulation with promising potential for eczema treatment.
REFERENCES
- Jemutai Kotut, S. Efficacy of Thunbergia alata asnd Senna didymobotrya Extracts Against Selected Bacteria Commonly Associated With Skin Infections in Kericho Referral Hospital, Kenya (Doctoral dissertation, UOK) (2024) .Retrived From: http://ir-library.kabianga.ac.ke/handle/123456789/964
- Lohmann, R. M. Drug-Induced skin hypersensitivity reactions: a review of clinical cases and literature (Doctoral dissertation, Vilniaus universitetas.). (2024) Retrived From: https://epublications.vu.lt/object/elaba:210545000/
- Cleeland, C. S. Symptom burden: multiple symptoms and their impact as patient-reported outcomes. Journal of the National Cancer Institute Monographs, 2007(37), 16-21. (2007). Retrived From: https://academic.oup.com/jncimono/article/2007/37/16/2937729
- Chong, M., & Fonacier, L. Treatment of eczema: corticosteroids and beyond. Clinical reviews in allergy & immunology, 51, 249-262. (2016). Retrived From: https://link.springer.com/article/10.1007/s12016-015-8486-7
- Coondoo, A., Phiske, M., Verma, S., & Lahiri, K. Side-effects of topical steroids: A long overdue revisit. Indian dermatology online journal, 5(4), 416-425. (2014) Retrived From: https://journals.lww.com/idoj/fulltext/2014/05040/Side_effects_of_topical_steroids__A_long_overdue.2.aspx/1000
- Schiffman, S. S. Influence of medications on taste and smell. World journal of otorhinolaryngology-head and neck surgery, 4(01), 84-91. (2018) Retrived From: https://mednexus.org/doi/full/10.1016/j.wjorl.2018.02.005
- Thacharodi, A., Singh, P., Meenatchi, R., Tawfeeq Ahmed, Z. H., Kumar, R. R., V, N., ... & Hassan, S. (2024). Revolutionizing healthcare and medicine: The impact of modern technologies for a healthier future—A comprehensive review. Health Care Science, 3(5), 329-349. (2024) Retrived From: https://onlinelibrary.wiley.com/doi/full/10.1002/hcs2.115
- Khiljee, S., Rehman, N. U., Khiljee, T., Ahmad, R. S., Khan, M. Y., & Qureshi, U. A. Use of traditional herbal medicines in the treatment of eczema. Journal of Pakistan Association of Dermatologists, 21(2), 112-117. (2011). Retrived From: https://www.jpad.com.pk/index.php/jpad/article/view/453
- Anand, A., Kaur, S., Vani, S. K., & Ohri, R. The Antimicrobial and Skin Nourishing Benefits of Neem and Aleo vera in Herbal Hand wash Formulation. Journal of Advancement in Pharmacognosy, 4(2). (2024). Retrived From: https://crsubscription.com/journals/pharmacy/pharmacognosy/articles/2024/[48-61]-Neem-and-Aleo-vera-in-Herbal-Hand-wash-Formulation.pdf
- Malavi, S., Kumbhar, P., Manjappa, A., Chopade, S., Patil, O., Kataria, U., ... & Disouza, J. Topical Emulgel: Basic Considerations in Development and Advanced Research. Indian Journal of Pharmaceutical Sciences, 84(5). (2022). Retrived From: https://pdfs.semanticscholar.org/b31b/d4414bf698a6faacf375b9482fe6ab27b21b.pdf
- Singh, V., Roy, M., Garg, N., Kumar, A., Arora, S., & Malik, D. S. An insight into the dermatological applications of neem: a review on traditional and modern aspect. Recent Advances in Anti-Infective Drug Discovery Formerly Recent Patents on Anti-Infective Drug Discovery, 16(2), 94-121. (2021). Retrived From: https://www.ingentaconnect.com/content/ben/raaidd/2021/00000016/00000002/art00003
- Çetin, H., Y?lmaz, H., & Demiroz, G. A. Preparation of Aloe Vera Gel Containing Solid Lipid Nanoparticles for Treatment of Eczema. Erzincan University Journal of Science and Technology, 17(3), 663-677. (2024). Retrived From: https://dergipark.org.tr/en/pub/erzifbed/issue/89001/1529097
- Zari, S. T., & Zari, T. A. A review of four common medicinal plants used to treat eczema. Journal of Medicinal Plants Research, 9(24), 702-711. (2015). Retrived From: https://academicjournals.org/journal/JMPR/article-full-text-pdf/1851EB753877.pdf
- Ness, R. D. Integrative therapies. Clinical avian medicine, 343-364. (2006). Retrived From: https://www.harrisonsbirdfoods.com/wp-content/uploads/2024/02/10_integrativemed.pdf
- Emerald, M. Medicinal Plants: Therapeutic Potential, Safety, and Toxicity. In Drug Discovery and Evaluation: Safety and Pharmacokinetic Assays (pp. 1327-1397). Cham: Springer International Publishing. (2024).Retrived From: https://link.springer.com/referenceworkentry/10.1007/978-3-031-35529-5_90
- Hekmatpou, D., Mehrabi, F., Rahzani, K., & Aminiyan, A. The Effect of Aloe Vera Clinical Trials on Prevention and Healing of Skin Wound: A Systematic Review. Iranian journal of medical sciences, 44(1), 1–9. (2019). Retrived From: https://pmc.ncbi.nlm.nih.gov/articles/PMC6330525/
- Venugopalan Nair, S. N., Shilpa, N., Vargheese, T., & Tabassum, I. F. Neem: Traditional knowledge from Ayurveda. The Neem Genome, 1-12. . (2019). Retrived From: https://link.springer.com/chapter/10.1007/978-3-030-16122-4_1
- Vadivel, S. A., Anbazhagan, S., Prasanth, R., Jayaprakash, B. N., Jegadeeswari, P., & Asha, G. A COMPREHENSIVE REVIEW OF PHYTOMOLECULES USED IN THE TREATMENT OF SKIN DISEASES. (2024). Retrived From:https://wjpr.s3.ap-south-1.amazonaws.com/article_issue/77507cf888ac32db8001633ac788c162.pdf
- Alexander, A., Khichariya, A., Gupta, S., Patel, R. J., Giri, T. K., & Tripathi, D. K. Recent expansions in an emergent novel drug delivery technology: Emulgel. Journal of Controlled Release, 171(2), 122-132. (2013). Retrived From: https://www.sciencedirect.com/science/article/abs/pii/S0168365913003775
- Chong, M., & Fonacier, L. (2016). Treatment of eczema: corticosteroids and beyond. Clinical reviews in allergy & immunology, 51, 249-262. Retrived From:: https://www.tandfonline.com/doi/full/10.2147/ccid.s6496
- Walling, H. W., & Swick, B. L. (2010). Update on the management of chronic eczema: new approaches and emerging treatment options. Clinical, cosmetic and investigational dermatology, 99-117. Retrived From: https://www.tandfonline.com/doi/full/10.2147/ccid.s6496
- Downer, S. M., Cody, M. M., McCluskey, P., Wilson, P. D., Arnott, S. J., Lister, T. A., & Slevin, M. L. (1994). Pursuit and practice of complementary therapies by cancer patients receiving conventional treatment. Bmj, 309(6947), 86-89. Retrived From: https://www.bmj.com/content/309/6947/86.abstract
- Radhakrishnan, J., Kennedy, B. E., Noftall, E. B., Giacomantonio, C. A., & Rupasinghe, H. V. (2024). Recent advances in phytochemical-based topical applications for the management of eczema: a review. International Journal of Molecular Sciences, 25(10), 5375. Retrived From: https://www.mdpi.com/1422-0067/25/10/5375
- Chan, K. (2003). Some aspects of toxic contaminants in herbal medicines. Chemosphere, 52(9), 1361-1371. Retrived From: https://www.sciencedirect.com/science/article/abs/pii/S0045653503004715
- Moreira, D. D. L., Teixeira, S. S., Monteiro, M. H. D., De-Oliveira, A. C. A., & Paumgartten, F. J. (2014). Traditional use and safety of herbal medicines. Revista Brasileira de Farmacognosia, 24(2), 248-257. Retrived From: https://www.sciencedirect.com/science/article/pii/S0102695X1400012X
- Shaker, D. S., Ishak, R. A., Ghoneim, A., & Elhuoni, M. A. (2019). Nanoemulsion: A review on mechanisms for the transdermal delivery of hydrophobic and hydrophilic drugs. Scientia Pharmaceutica, 87(3), 17. Retrived From: https://www.mdpi.com/2218-0532/87/3/17
- Bhadouria, V. S., Verma, S., Mishra, R., & Kapoor, B. (2024). Beyond Creams and Gels: The Emergence of Emulgels in Pharmaceutical Science. Current Drug Therapy. Retrived From: https://www.benthamdirect.com/content/journals/cdth/10.2174/0115748855320930240920040523
- Olayemi, O. J., & David, C. (2023). Emulgel: A promising technology for topical delivery of herbal extracts. British Journal of Pharmacy, 8(1), 1-13. Retrived From: https://search.informit.org/doi/abs/10.3316/informit.200703012639514
- Thakur, L., Ghodasra, U., Patel, N., & Dabhi, M. (2011). Novel approaches for stability improvement in natural medicines. Pharmacognosy reviews, 5(9), 48. Retrived From: https://pmc.ncbi.nlm.nih.gov/articles/PMC3210007/
- Dubey, S., & Dixit, A. K. (2023). Preclinical evidence of polyherbal formulations on wound healing: A systematic review on research trends and perspectives. Journal of Ayurveda and Integrative Medicine, 14(2), 100688. Retrived From: https://www.sciencedirect.com/science/article/pii/S0975947623000037
- Shukla, S. S., Pandey, R. K., Gidwani, B., & Kalyani, G. (2023). Approach for Herbal Standardization. In Pharmaceutical Calibration, Validation and Qualification: A Comprehensive Approach (pp. 187-198). Singapore: Springer Nature Singapore. Retrived From: https://link.springer.com/chapter/10.1007/978-981-19-9002-1_14
- Ellison, S. L., & Botha, A. (2018). Principles for the assessment of homogeneity and stability in the new ISO Guide 35: 2017. Accreditation and Quality Assurance, 23(1), 47-51. Retrived From: https://link.springer.com/article/10.1007/s00769-017-1293-5
- Sharma, A., Gupta, R., & Mehta, D. (2021). Polyherbal formulations for dermatological disorders: A review on therapeutic potential and formulation strategies. Journal of Herbal Medicine, 29, 100472. Retrived From: https://doi.org/10.1016/j.hermed.2021.100472
- Patel, M. R., Patel, R. B., Parikh, J. R., & Solanki, A. B. (2011). Development and evaluation of a liposomal formulation containing curcumin for the treatment of inflammation. Journal of Advanced Pharmaceutical Technology & Research, 2(2), 102–109. Retrived From: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3217692/
- Atawodi, S. E., & Atawodi, J. C. (2009). Azadirachta indica (neem): a plant of multiple biological and pharmacological activities. Phytochemistry reviews, 8, 601-620. Retrived From: https://link.springer.com/article/10.1007/s11101-009-9144-6
- Akbar, S. (2020). Aloe vera (L.) Burm. f.(Asphodelaceae/Xanthorrhoeaceae) (Syns.: A. barbadensis Mill.; A. chinensis Steud. ex Baker; A. elongata Murray; A. vulgaris Lam.). In Handbook of 200 Medicinal Plants: A Comprehensive Review of Their Traditional Medical Uses and Scientific Justifications (pp. 187-206). Cham: Springer International Publishing. Retrived From: https://link.springer.com/chapter/10.1007/978-3-030-16807-0_18
- Chimane, P. A., Mangale, P. D., & Watangi, R. U. FORMULATION AND EVALUATION OF HERBAL EMULGEL LOADED WITH EXTRACT OF BUCHANANIALANZAN LEAVES. Retrived From: https://iajpr.com/iajprfiles/uploaddir/240513_DOI.pdf
- Balamurugan, V., Fatima, S., & Velurajan, S. (2019). A guide to phytochemical analysis. International Journal of Advance Research and Innovative Ideas in Education, 5(1), 236-245.Retrived From: https://www.researchgate.net/profile/Vishnu-Balamurugan/publication/330509328_A_GUIDE_TO_PHYTOCHEMICAL_ANALYSIS/Links/5c44d1f2299bf12be3d78f70/A-GUIDE-TO-PHYTOCHEMICAL-ANALYSIS.pdf


 Daund Trupti *
Daund Trupti *
 Chavhan Shankar
Chavhan Shankar
 Daund Prabhanjan
Daund Prabhanjan
 Patil Pragati
Patil Pragati


















 10.5281/zenodo.15348093
10.5281/zenodo.15348093