Abstract
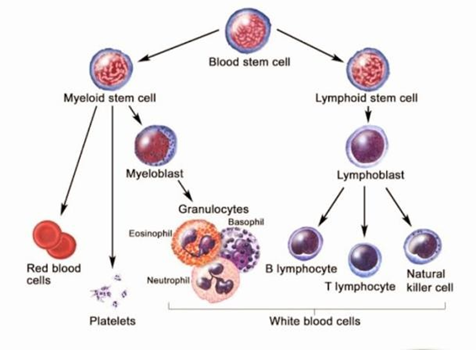
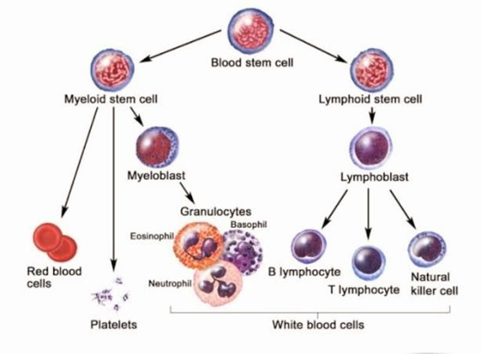
Chronic lymphocytic leukemia (CLL)/small lymphocytic lymphoma (SLL) is a common indolent B-cell malignancy characterized by the accumulation of mature B lymphocytes in the blood, bone marrow, and lymphoid tissues. The management of CLL/SLL has evolved significantly in recent years, with advances in targeted therapies and novel immunotherapies. Chronic lymphocytic leukemia (CLL) is a type of cancer that affects white blood cells called lymphocytes. Lymphocytes are part of the immune system and help fight infections. In Chronic Lymphocytic Leukemia, the lymphocytes grow and accumulate abnormally, leading to various health issues.
Keywords
Cancer, Chronic, Leukemia, Lymphocytes, Lymphoma.
Introduction
Chronic lymphocytic leukemia (CLL) is a type of cancer that affects white blood cells called lymphocytes. Lymphocytes are part of the vulnerable system and help fight infections. In Chronic Lymphocytic Leukemia, the lymphocytes grow and accumulate abnormally, leading to colorful health issues. Chronic Lymphocytic Leukemia is a type of cancer that starts in the white blood cells called B cells. These cells help fight infections. With Chronic Lymphocytic Leukemia, too numerous B cells are made, and they don’t work the way they should. This makes it harder for the body to fight off origins. Chronic lymphocytic leukemia is a malignant condition characterized by the uncontrolled proliferation of lymphocytes, a specific type of white blood cell. Unlike other leukemia, Chronic Lymphocytic Leukemia typically progresses at a relatively slow pace. This is reflected in the term “chronic” within its name.
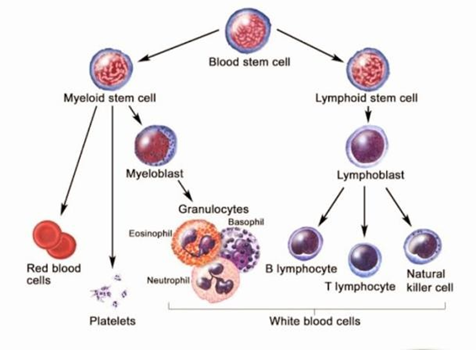
Fig 2: Basic Concept of Chronic lymphocytic leukemia
Most people with Chronic Lymphocytic Leukemia don’t have any symptoms for a long time. But as the cancer grows, you might feel tired and have swollen lymph. Nodes, or get sick often. There are treatments available for Chronic Lymphocytic Leukemia and many people with the condition can live long and healthy lives. Key treatment principles for CLL/SLL include observation for asymptomatic patients, targeted therapies for symptomatic patients, and allogeneic hematopoietic stem cell transplantation (HSCT) for select patients with high-risk disease.
Targeted therapies, such as Bruton tyrosine kinase (BTK) inhibitors and phosphatidylinositol 3-kinase (PI3K) inhibitors, have revolutionized the treatment landscape by significantly improving outcomes and reducing treatment-related toxicities.
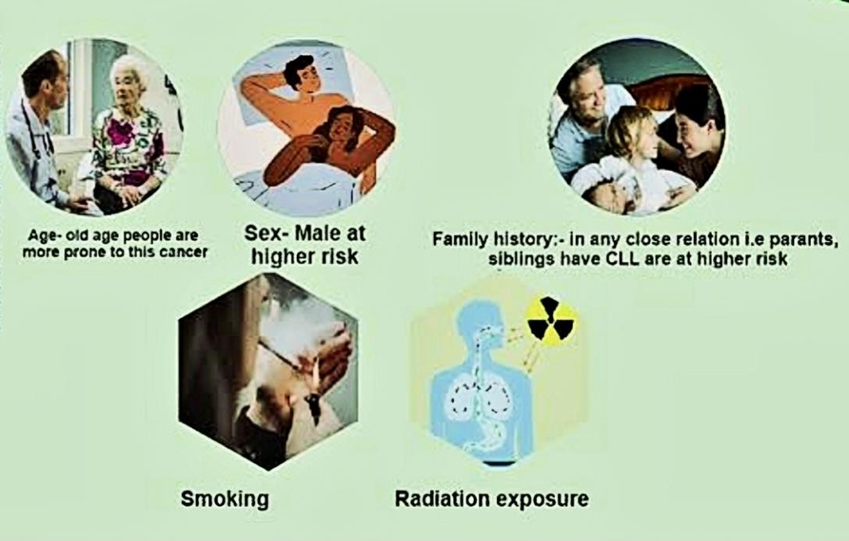
Etiology Chronic Lymphocytic Leukemia: -
Chronic lymphocytic leukemia (CLL) is a type of cancer characterized by the abnormal accumulation of mature B lymphocytes in the blood, bone marrow, and lymph nodes. While the exact cause of Chronic Lymphocytic Leukemia remains unknown, several factors have been implicated in its development.
1. Genetic Factors:
a) Inherited Genes: Certain genetic variations can increase the risk of developing Chronic Lymphocytic Leukemia. These variations may affect the function of genes involved in immune system development or cell growth and survival.
b) Chromosomal Abnormalities: Chronic Lymphocytic Leukemia is often associated with specific chromosomal abnormalities, such as deletions or additions of genetic material. These abnormalities can disrupt the normal function of genes involved in regulating B cell development and survival.
2. Environmental Factors:
a) Exposure to Chemicals and Radiation: Exposure to certain chemicals and radiation, such as benzene and ionizing radiation, has been linked to an increased risk of Chronic Lymphocytic Leukemia. However, the exact mechanisms by which these exposures contribute to Chronic Lymphocytic Leukemia development are not fully understood.
b) Infections: Some studies suggest that certain infections, such as Epstein-Barr virus (EBV) and hepatitis C virus (HCV), may be associated with an increased risk of Chronic Lymphocytic Leukemia. However, the causal relationship between these infections and Chronic Lymphocytic Leukemia is still under investigation.
c) Lifestyle Factors: While research on lifestyle factors and Chronic Lymphocytic Leukemia risk is ongoing, some studies have suggested that certain lifestyle
factors, such as smoking and obesity, may be associated with an increased risk of the disease.
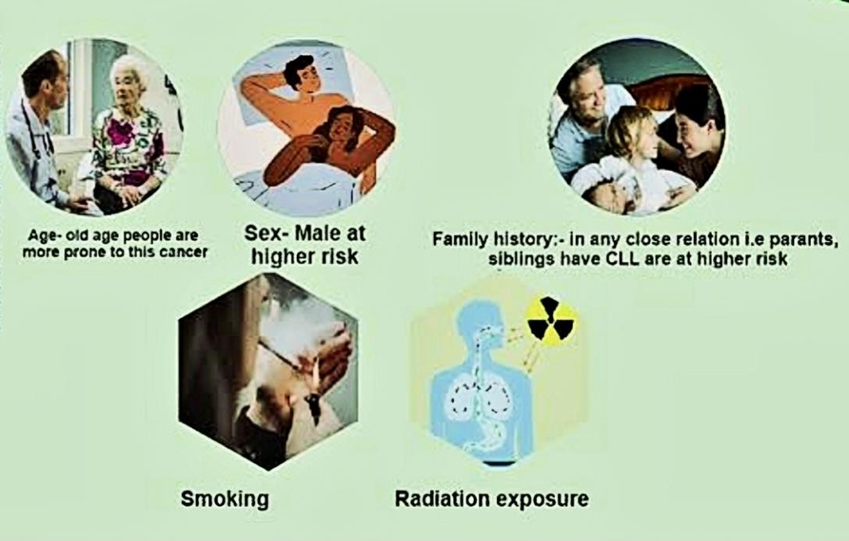
Fig 3: Etiology of Chronic lymphocytic leukemia
3. Immune System Dysfunction:
a) Autoimmune Disorders: Chronic Lymphocytic Leukemia is sometimes associated with autoimmune disorders, such as rheumatoid arthritis and
Hashimoto’s thyroiditis. This suggests that there may be a link between immune system dysfunction and the development of Chronic Lymphocytic Leukemia.
b) Defects in Immune Cell Function: Chronic Lymphocytic Leukemia is characterized by the accumulation of abnormal B cells, which can interfere with the normal function of the immune system. This may contribute to the development of Chronic Lymphocytic Leukemia and other infections.
4. Aging:
a) Age-Related Changes: Chronic Lymphocytic Leukemia is most commonly diagnosed in older adults. This suggests that age-related changes in the immune system or genetic material may play a role in the development of the disease.
Epidemiology of Chronic Lymphocytic Leukemia:-
The American Cancer Society estimates that eighteen thousand, seven hundred and forty new cases of chronic lymphocytic leukemia will be diagnosed in the United States in two thousand and twenty-three. The true incidence in the US is unknown and is likely higher, as estimates of Chronic Lymphocytic Leukemia incidence come from tumor registries, and many cases are not reported. Although the incidence of Chronic Lymphocytic Leukemia has been stable over the last two decades, mortality has been steadily declining.
While the prevalence of chronic lymphocytic leukemia (CLL) in Western nations is comparable to that of the United States, it is notably uncommon in Asian countries such as China and Japan, constituting an estimated 10% of all leukemia cases.
Nevertheless, the true incidence of Chronic Lymphocytic Leukemia in these regions may be considerably underestimated due to underreporting and incomplete registries.

Fig 4: Epidemiology according to age
The prevalence of chronic lymphocytic leukemia (CLL) is more common in men than women, with a male-to-female ratio of 1.9:1. Chronic Lymphocytic Leukemia is predominantly a disease affecting the elderly, with the average age at diagnosis being 70 years. In familial Chronic Lymphocytic Leukemia, where at least one first-degree relative is also diagnosed with CLL, the average age at diagnosis is notably lower at 57 years.
Pathophysiology of Chronic Lymphocytic Leukemia:-
The etiologic cells in a majority of Chronic Lymphocytic Leukemia cases are clonal B lymphocytes arrested in the B-cell differentiation process, situated between the pre-B and mature B cell stages. Morphologically, these cells exhibit a resemblance to mature lymphocytes when examined in peripheral blood. Chronic Lymphocytic Leukemia B lymphocytes exhibit exceptionally low levels of surface membrane immunoglobulin, predominantly immunoglobulin M (IgM) or a combination of IgM and IgD. Furthermore, they express minimal levels of a solitary immunoglobulin light chain, either kappa or lambda. A deviant karyotype is identified in a significant proportion of individuals with Chronic Lymphocytic Leukemia. The most prevalent abnormality is a deletion of chromosome 13q, occurring in more than half of patients. Individuals exhibiting 13q14 abnormalities typically present with a relatively benign disease characterized by stable or gradually progressing isolated lymphocytosis. Chronic lymphocytic leukemia (CLL) is primarily caused by a clonal proliferation of B cells that are arrested at an intermediate stage between pre-B cells and mature B cells. These abnormal B cells resemble mature lymphocytes when viewed under a microscope.
Chronic Lymphocytic Leukemia B-
Lymphocytes typically express specific B-cell surface antigens, including CD19, CD20dim, CD21, and CD23. Additionally, they express CD5, a protein more commonly found in T cells. This suggests that Chronic Lymphocytic Leukemia might originate from a subpopulation of self-reactive B cells found in the mantle zone of lymphoid follicles.
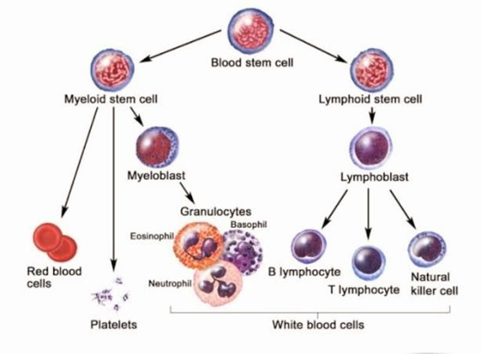
Fig 5: Pathophysiology of Chronic Lymphocytic Leukemia
Chronic Lymphocytic Leukemia B-lymphocytes produce very low levels of surface membrane immunoglobulin, primarily IgM or IgM/IgD and IgD. They also express very low levels of a single immunoglobulin light chain (kappa or lambda).
Genetic abnormalities are common in Chronic Lymphocytic Leukemia. The most frequent abnormality is a deletion of chromosome 13q, which occurs in over 50% of patients. Individuals with this deletion often have a relatively mild form of the disease. Other genetic abnormalities, such as deletions of chromosomes 11q and 17p, and trisomy 12, have also been reported. The presence of trisomy 12 is associated with atypical morphology and more aggressive disease. Deletions in chromosome 17p are linked to rapid disease progression, shorter remissions, and decreased overall survival. The proto-oncogene Bcl2 is overexpressed in B-cell CLL. Bcl2 is a protein that suppresses programmed cell death, allowing the leukemic cells to survive for a prolonged period. While Bcl2 overexpression is common in Chronic Lymphocytic Leukemia, genetic translocations that directly cause Bcl2 overexpression, such as t(14;18), are not typically found. Understanding the molecular pathophysiology of Chronic Lymphocytic Leukemia has led to the development of targeted therapies, such as venetoclax, which blocks the Bcl2 protein. Studies have indicated that an increase in the expression of Bcl2 is associated with deletions within chromosomal band 13q14. Located within this region are two genes, designated miRNA15a and miRNA16-1, which have been determined to encode not proteins, but rather regulatory RNAs termed microRNAs (miRNAs). [10, 11] These miRNA genes are members of a family of highly conserved noncoding genes dispersed throughout the genome whose transcripts suppress gene expression by inducing the degradation of mRNA or by obstructing the transcription of mRNA.
Deletions of miRNA15a and miRNA16-1 result in the overexpression of Bcl2 due to the loss of downregulating miRNAs. Genetic analyses have revealed deletions or diminished expression of these miRNA genes in approximately 70% of Chronic Lymphocytic Leukemia cases.
Investigations have also identified several high-risk genetic features and markers, including germline immunoglobulin variable heavy chain (IgV H) gene usage, specifically the IgV H V3-21 gene, increased expression of CD38 and Zap70, elevated serum levels of beta-2-microglobulin and thymidine kinase, a short lymphocyte doubling time of less than 6 months, and increased serum levels of soluble CD23.
Signs and Symptoms of Chronic Lymphocytic Leukemia:-
While many people with Chronic Lymphocytic Leukemia have no symptoms at all, especially in the early stages, some common signs and symptoms include:
a) Fatigue: Feeling tired or weak, even with minimal activity.
b) Swollen lymph nodes: These are often painless and found in the neck, underarms, or groin.
c) Frequent infections: Due to a weakened immune system.
d) Unexplained weight loss: Losing weight without making any dietary or exercise changes.
e) Night sweats: Waking up drenched in sweat during the night.
f) Shortness of breath: Difficulty breathing, even during mild exertion.
g) Pain in the upper left abdomen: This can be caused by an enlarged spleen.
h) Bruising or bleeding easily: Due to low platelet levels.
i) Fever: A persistent low-grade fever.
Complications of Chronic Lymphocytic Leukemia:-
1. Frequent infections –
Individuals with chronic lymphocytic leukemia may encounter recurrent infections of a severe nature. These infections often arise due to a deficiency in germ-fighting antibodies, known as immunoglobulins, in the bloodstream. Your healthcare provider may suggest regular infusions of immunoglobulins as a therapeutic intervention.
2. Switch to a more aggressive form of cancer -
A subset of individuals diagnosed with chronic lymphocytic leukemia may experience disease progression, manifesting as diffuse large B-cell lymphoma, a more aggressive form of cancer. This transformation is often termed Richter’s syndrome by healthcare professionals.
3. Increased risk of other cancers -
People with chronic lymphocytic leukemia have an increased risk of other types of cancer, like skin cancer, and cancers of the lung and the digestive tract.
4. Immune system problems -
A subset of individuals afflicted with chronic lymphocytic leukemia may experience an immunological aberration characterized by the aberrant targeting of erythrocytes or thrombocytes by the immune system’s defensive cells, resulting in autoimmune hemolytic anemia or autoimmune thrombocytopenia, respectively.
Diagnosis of Chronic Lymphocytic Leukemia:-
Chronic Lymphocytic Leukemia (CLL) is a type of cancer that majorly affects the white blood cells. While it often progresses slowly, it’s important to catch it early for effective treatment.
1. Blood Tests:
a) Complete Blood Count (CBC): This is the initial test to check for an abnormally high number of white blood cells, specifically lymphocytes.
b) Flow Cytometry: This test analyses the surface markers on the lymphocytes to confirm they are Chronic Lymphocytic Leukemia cells.
2. Bone Marrow Biopsy:
A small sample of bone marrow is taken to examine the presence and number of Chronic Lymphocytic Leukemia cells. This helps determine the stage of the
disease.
3. Additional Tests:
a) Cytogenetics: Examines the chromosomes of the Chronic Lymphocytic Leukemia cells to identify any genetic abnormalities that might affect the disease’s progression.
b) FISH (Fluorescence In Situ Hybridization): A more sensitive technique to detect specific genetic abnormalities in Chronic Lymphocytic Leukemia cells.
c) Imaging Studies (CT, PET scan): These may be used to assess the extent of the disease, especially if symptoms suggest the involvement of organs like the liver or spleen.
Prognosis of Chronic Lymphocytic Leukemia:-
The outcome for patients diagnosed with Chronic Lymphocytic Leukemia (CLL) can vary significantly. While some patients may experience rapid disease progression and mortality within a few years, others may initially have a milder course. However, the disease often progresses to a more aggressive stage, resistant to treatment, leading to substantial morbidity. Despite advancements in therapy, Chronic Lymphocytic Leukemia is rarely cured, and mortality rates remain elevated compared to the general population. The prognosis is influenced by the disease stage at diagnosis and the presence of high-risk markers. Due to recent therapeutic advancements, the traditional Rai and Binet staging systems are less effective in predicting prognosis. The Chronic Lymphocytic Leukemia International Prognostic Index (CLL-IPI) is currently the most accurate tool used by oncologists, considering five key prognostic factors.
1. Patient age
2. Clinical stage
3. Serum B2 microglobulin level
4. Mutational status of immunoglobulin heavy chain variable (IGVH)
5. 17p deletion and/or TP53 mutation
Based on the presence or absence of prognostic factors as assessed by the CLL-IP| calculator, patients are categorized into low-, intermediate-, high-, or very high-risk groups. Patients in the low-risk category have a greater than 90% likelihood of 5-year overall survival and, consequently, are not recommended for treatment. Intermediate-risk patients have approximately a 90% chance of 5-year overall survival and are treated only when symptoms are present. High-risk patients are managed like intermediate-risk patients, although they have a slightly lower probability of 5-year overall survival, estimated at 63%. Patients in the very high-risk category are treated with targeted therapeutic agents.
Key treatment principles for Chronic Lymphocytic Leukemia:-
Chronic lymphocytic leukemia (CLL) is a type of cancer that affects white blood cells. While there is no cure, the goal of treatment is to manage symptoms, improve quality of life, and prolong survival.
a) Targeted Therapies:
Targeted therapies are a type of treatment that generally targets cancer cells and cause minimal damage to healthy cells. These therapies have revolutionized the treatment of chronic lymphocytic leukemia (CLL), a type of blood cancer.
Common Targeted Therapies for Chronic Lymphocytic Leukemia
i) BTK Inhibitors:
Ibrutinib, acalabrutinib, zanubrutinib: These drugs block a protein called Bruton’s tyrosine kinase (BTK), which is essential for the survival of Chronic Lymphocytic Leukemia cells. They are often used as first-line treatments or in combination with other therapies.
ii) PI3K Inhibitors:
Idelalisib, and duvelisib: These drugs block the PI3K pathway, which is involved in cell survival and growth. These medications are often used in combination with other therapies.
iii) BCL-2 Inhibitors:
Venetoclax: This drug blocks BCL-2, a protein that prevents cell death. It is often used in combination with rituximab, a monoclonal antibody that targets B cells.
iv) CD20 Antibodies:
Rituximab, and obinutuzumab: These drugs target CD20, a protein found on B cells. These medications can be used alone or in combination with other therapies.
b) Chemotherapy:
Chemotherapy is a common treatment option for chronic lymphocytic leukemia (CLL). It involves the use of medications that kill the cancer cells. However, the Specific chemotherapy drugs used and the treatment plan will depend on various factors, including the stage of Chronic Lymphocytic Leukemia and overall health.
Here are some of the most common chemotherapy drugs used for Chronic Lymphocytic Leukemia:
i) Chlorambucil: This is a relatively mild chemotherapy drug that is often used as a first-line treatment for Chronic Lymphocytic Leukemia. It can be taken orally.
ii) Fludarabine: This is a more potent chemotherapy drug that is often used for patients with more advanced Chronic Lymphocytic Leukemia. It can be given intravenously.
iii) Cyclophosphamide: This is another chemotherapy drug that can be used for Chronic Lymphocytic Leukemia. These can be given orally or intravenously.
iv) Rituximab: While not technically a chemotherapy drug, Rituximab is a
monoclonal antibody that targets B cells, which are the type of white blood cells affected by Chronic Lymphocytic Leukemia. It can be given intravenously.
c) Immunotherapy:
Immunotherapy is a type of treatment that helps your immune system fight cancer cells. It's become a significant advancement in treating Chronic Lymphocytic.
Leukemia offers targeted approaches that can often be less toxic than traditional chemotherapy.
Common Immunotherapy Treatments for Chronic Lymphocytic Leukemia:
i) Monoclonal Antibodies: These are laboratory-made proteins that bind to specific targets on cancer cells. Some common monoclonal antibodies used for CLL
Include:
Rituximab: Targets CD20 proteins on B cells, which are the type of white blood cells affected by Chronic Lymphocytic Leukemia.
Ofatumumab: Targets CD20 proteins but works differently than Rituximab.
Obinutuzumab: Also targets CD20 proteins and is often used in combination with chemotherapy.
ii) Checkpoint Inhibitors: These drugs help your immune system recognize and attack cancer cells. They work by blocking certain “checkpoints” that prevent the immune system from attacking healthy cells. Examples include:
Ibrutinib: Targets Bruton’s tyrosine kinase (BTK), a protein involved in B cell signaling.
Venetoclax: Targets BCL-2, a protein that helps cancer cells survive.
iii) CAR T-Cell Therapy: This is a highly specialized treatment where your T cells are genetically engineered to recognize and attack cancer cells. It’s often used for patients with relapsed or refractory Chronic Lymphocytic Leukemia.
d) Stem Cell Transplant:
A stem cell transplant is a complex medical procedure that can be a highly effective treatment option for certain patients with chronic lymphocytic leukemia (CLL). It involves replacing damaged bone marrow with healthy stem cells, which can then produce new blood cells.
There are two main types of stem cell transplants:
i) Autologous transplant: In this type, the patient's stem cells are collected, stored, and then re-infused after the high-dose chemotherapy or radiation therapy.
ii) Allogeneic transplant: Here, stem cells are donated by another person, usually a sibling or a matched unrelated donor.
Recent Updates in the Management of Chronic Lymphocytic Leukemia:-
Chronic lymphocytic leukemia (CLL) has witnessed significant advancements in treatment strategies in recent years. These developments have led to improved outcomes for patients, particularly those with previously challenging disease characteristics.
1. Targeted Therapies:
• BTK Inhibitors: Drugs like ibrutinib, acalabrutinib, and zanubrutinib have revolutionized Chronic Lymphocytic Leukemia treatment. By inhibiting the Bruton tyrosine kinase (BTK) enzyme, these agents disrupt the signaling
pathways that promote Chronic Lymphocytic Leukemia cell survival and proliferation. They have shown impressive efficacy, especially in patients with high-risk features like del17p13 or TP53 mutations.
• BCL-2 Inhibitors: Venetoclax, a BCL-2 inhibitor, has become a cornerstone of CLL therapy. It selectively targets BCL-2, a protein that prevents cell
death. Venetoclax has demonstrated significant efficacy in both previously untreated and relapsed/refractory Chronic Lymphocytic Leukemia,
particularly in combination with other agents.
2. Combination Therapies:
• Fixed-Dose Combinations: The FDA has approved fixed-dose
combinations of ibrutinib with rituximab and venetoclax with rituximab, simplifying treatment regimens and improving patient convenience.
• Novel Combinations: Ongoing research is exploring new combinations of targeted therapies with immunotherapy agents, such as chimeric antigen receptor (CAR) T cells, to enhance treatment responses and overcome resistance.
3. Immunotherapy:
• CAR T Cell Therapy: While still under investigation, CAR T cell therapy holds promise for patients with relapsed/refractory Chronic Lymphocytic
Leukemia. This approach involves engineering a patient’s T cells to express a chimeric antigen receptor that recognizes and attacks Chronic.
Lymphocytic Leukemia cells.
• Bispecific Antibodies: Bispecific antibodies, which simultaneously bind to both Chronic Lymphocytic Leukemia cells and immune cells, are being studied as a potential new treatment option.
4. Precision Medicine:
• Genetic Testing: Advances in genetic testing are enabling the identification of specific genetic alterations in Chronic Lymphocytic Leukemia cells. This
Information can guide treatment decisions and help select the most effective therapies for individual patients.
• Minimal Residual Disease (MRD) Monitoring: MRD assessment is becoming increasingly important in Chronic Lymphocytic Leukemia management. By measuring the levels of residual leukemia cells after treatment, MRD monitoring can help predict relapse risk and guide
decisions about additional therapy
REFERENCES
- Marwick C. Link found between Agent Orange and chronic lymphocytic leukemia. BMJ. 2003 Feb 01;326(7383):242. [PMC free_article] [PubMed] 11. Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020.CA Cancer I Clin. 2020 Jan;70(1):7-30.
- Hernández JA, Land KJ, McKenna RW. Leukemias, myeloma, and other lymphoreticular neoplasms. Cancer. 1995 Jan 01;75(1 Suppl):381-94.
- Smith A, Howell D, Patmore R, Jack A, Roman E. Incidence of hematological malignancy by sub-type: a report from the Haematological Malignancy Research Network. Br J Cancer. 2011 Nov 22;105(11):1684-92.
- Yamamoto JF, Goodman MT. Patterns of leukemia incidence in the United States by subtype and demographic characteristics, 1997-2002. Cancer Causes Control. 2008 May;19(4):379-90.
- PDQ Adult Treatment Editorial Board. PDQ Cancer Information Summaries [Internet]. National Cancer Institute (US); Bethesda (MD): Dec 8, 2023. Chronic Lymphocytic Leukemia Treatment.
- Hallek M, Cheson BD, Catovsky D, Caligaris-Cappio F, Dighiero G, Döhner H, Hillmen P, Keating M, Montserrat E, Chiorazzi N, Stilgenbauer S, Rai KR, Byrd JC, Eichhorst B, O’Brien S, Robak T, Seymour JF, Kipps TJ. I will guidelines for diagnosis, indications for treatment, response assessment, and supportive management of CLL. Blood. 2018 Jun 21;131(25):2745-2760.
- Rai KR, Sawitsky A, Cronkite EP, Chanana AD, Levy RN, Pasternack BS. Clinical staging of chronic lymphocytic leukemia. Blood. 1975 Aug:46(2):219-34.
- Mauro FR, Foa R, Cerretti R, Giannarelli D, Coluzzi S, Mandelli F, Girelli G. Autoimmune hemolytic anemia in chronic lymphocytic leukemia: clinical, therapeutic, and prognostic features. Blood. 2000 May 01;95(9):2786-92.
- Visco C, Ruggeri M, Laura Evangelista M, Stasi R, Zanotti: R, Giaretta I, Ambrosetti A, Madeo Pizzolo G, Rodeghiero F. Impact of immune thrombocytopenia on the clinical course of chronic lymphocytic leukemia. Blood. 2008 Feb 01;111(3):1110-6.
- Parikh SA, Leis JF, Chaffee KG, Call TG, Hanson CA, Ding W, Chanan-Khan AA, Bowen D, Conte M, Schwager S, Slager SL, Van Dyke DL, Jelinek DF, Kay NE, Shanafelt TD. Hypogammaglobulinemia in newly diagnosed chronic lymphocytic leukemia: Natural history, clinical correlates, and outcomes. Cancer. 2015 Sep 01;121(17):2883-91.
- Agnew KI, Ruchlemer R, Catovsky D, Matutes E, Bunker CB. Cutaneous findings in chronic lymphocytic leukemia. Br J Dermatol. 2004 Jun;150(6):1129-35.
- Robak E, Robak T. Skin lesions in chronic lymphocytic leukemia. Leuk Lymphoma. 2007 May:48(5):855-65.
- Lipshutz MD, Mir R, Rai KR, Sawitsky A. Bone marrow biopsy and clinical staging in chronic lymphocytic leukemia. Cancer. 1980 Sep 15;46(6):1422-7.
- Rozman C, Montserrat E, Rodríguez-Fernández JM, Ayats R, Vallespí T, Parody R, Rios A, Prados D, Morey M, Gomis F. Bone marrow histologic pattern—the best single prognostic parameter in chronic lymphocytic leukemia: a multivariate survival analysis of 329 cases. Blood. 1984 Sep;64(3):642-8.
- Effects of chlorambucil and therapeutic decision in initial forms of chronic lymphocytic leukemia (stage A): results of a randomized clinical trial on 612 patients. The French Cooperative Group on Chronic Lymphocytic Leukemia. Blood. 1990 Apr 01;75(7):1414-21.
- Morrison WH, Hoppe RT, Weiss LM, Picozzi VJ, Horning SJ. Small lymphocytic lymphoma. J Clin Oncol. 1989 May;7(5):598-606.
- Oloo AJ, Ogada TA. Chronic lymphocytic leukemia (CLL): clinical study at Kenyatta National Hospital (KNH). East Afr Med J. 1984 Nov;61(11):797-801.
- Binet JL, Auquier A, Dighiero G, Chastang C, Piguet H, Goasguen J, Vaugier G, Potron G, Colona P, Oberling F, Thomas M, Tchernia G, Jacquillat C, Boivin P, Lesty C, Duault MT, Monconduit M, Belabbes S, Gremy F. A new prognostic classification of chronic lymphocytic leukemia derived from multivariate survival analysis. Cancer. 1981 Jul 01;48(1):198-206.
- Dearden C, Wade R, Else M, Richards S, Milligan D, Hamblin T, Catovsky D., UK National Cancer Research Institute (NCRI). Haematological Oncology Clinical Studies Group. NCRI CLL Working Group. The prognostic significance of a positive direct antiglobulin test in chronic lymphocytic leukemia: a beneficial effect of the combination of fludarabine and cyclophosphamide on the incidence of hemolytic anemia. Blood. 2008 Feb 15;111(4):1820-6.
- Morrison WH, Hoppe RT, Weiss LM, Picozzi VJ, Horning SJ. Small lymphocytic lymphoma. J Clin Oncol. 1989 May;7(5):598-606.
- Tausch E, Schneider C, Robrecht S, Zhang C, Dolnik A, Bloehdorn J, Bahlo J. Al-Sawaf O, Ritgen M, Fink AM, Eichhorst B, Kreuzer KA, Tandon M, Humphrey K, Jiang Y, Schary W, Bullinger L, Mertens D, Lurà MP, Kneba M, Döhner H, Fischer K, Hallek M, Stilgenbauer S. Prognostic and predictive impact of genetic markers in patients with CLL treated with obinutuzumab and venetoclax. Blood. 2020 Jun 25;135(26):2402-2412.


 Randhawan B. B.
Randhawan B. B.

 10.5281/zenodo.14274926
10.5281/zenodo.14274926