Abstract
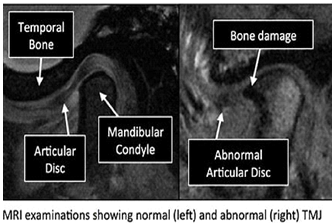
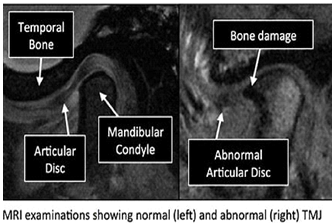
Temporomandibular joint (TMJ) disorders encompass a variety of conditions impacting the jaw's functional anatomy, leading to symptoms such as pain, restricted movement, and joint noises. Magnetic Resonance Imaging (MRI) has become a central diagnostic tool for TMJ disorders due to its ability to visualize soft tissue structures, such as the articular disc, synovial membrane, and surrounding ligaments, without exposing patients to ionizing radiation. MRI techniques, including static and dynamic imaging, provide insight into disc displacement, joint effusion, and early degenerative changes, facilitating accurate diagnoses and treatment planning. Despite its high diagnostic value, MRI has limitations, including high costs, long scan times, limited effectiveness in assessing muscle-related pain, and challenges in evaluating certain bone conditions. This review explores the applications, efficacy, and limitations of MRI in diagnosing TMJ disorders, emphasizing the need for a comprehensive clinical evaluation alongside imaging for optimal patient care.
Keywords
Temporomandibular Joint Disorders, Magnetic Resonance Imaging (MRI).
Introduction
Temporomandibular joint (TMJ) disorders represent a complex group of conditions affecting the Temporomandibular joint, which connects the jawbone to the skull. These disorders can lead to a variety of symptoms, including jaw pain, difficulty in chewing, and limited mouth opening, significantly impacting patients' quality of life. The multifactorial nature of TMJ disorders often involves both mechanical and psycho social factors, making accurate diagnosis challenging. Imaging plays a pivotal role in the evaluation of TMJ disorders, with Magnetic Resonance Imaging (MRI) emerging as a key diagnostic tool.1 MRI is particularly valuable due to its ability to provide high-resolution images of soft tissues without the use of ionizing radiation. This capability allows clinicians to visualize the complex anatomy of the TMJ, including the articular disc, ligaments, muscles, and surrounding structures, facilitating a comprehensive assessment of potential pathologies.2 Magnetic Resonance Imaging (MRI) is essential for diagnosing Temporomandibular joint disorders (TMDs), offering valuable insights into various internal derangement and degenerative conditions. Recent research underscores MRI's effectiveness in detecting disc displacements and other pathologies, achieving a Cohen's kappa value of 0.720, which reflects substantial agreement with clinical diagnoses.3 A study indicated an 87.5% concordance with clinical findings for internal derangement, showcasing its reliability in evaluating disc positions. Moreover, advancements in MRI techniques, including dynamic and quantitative approaches, enhance diagnostic capabilities by improving joint structure visualization, with emerging methods like diffusion-weighted imaging and T2 mapping being explored. However, despite its strengths, MRI faces limitations, particularly in diagnosing degenerative joint disease (DJD), where its specificity is only 43.1%.4 Additionally, its effectiveness in assessing the severity of condylar bone abnormalities is fair to moderate compared to cone-beam computed tomography (CBCT). Therefore, while MRI is a powerful tool, its limitations in specificity and severity assessment highlight the necessity of combining it with clinical evaluations and other imaging modalities for a comprehensive diagnosis of TMD5 The use of MRI in the context of TMJ disorders has evolved, enabling healthcare professionals to differentiate between various types of joint dysfunctions, such as disc displacement, arthritis, and inflammatory conditions. 6this review will explore the diagnostic applications of MRI in TMJ disorders, highlighting its advantages, common findings, limitations, and the implications for patient management. Understanding the role of MRI in this context is essential for improving diagnostic accuracy and tailoring effective treatment strategies for individuals suffering from TMJ disorders.
PRINCIPLES OF MRI
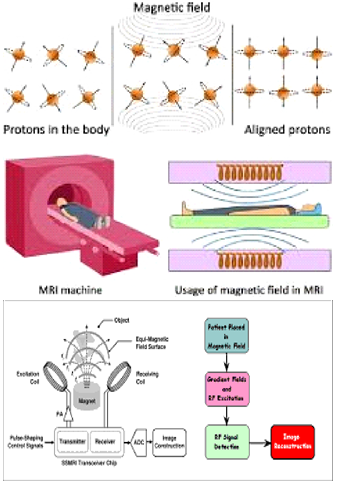
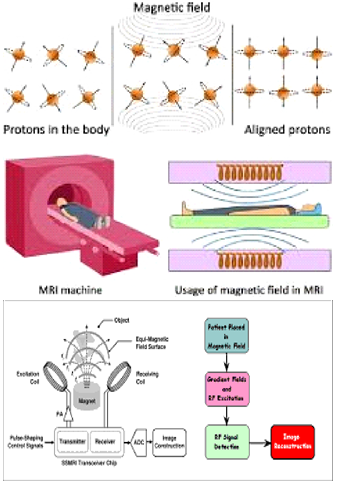
Magnetic Resonance Imaging (MRI) is a non-invasive imaging technique that leverages the electromagnetic properties of tissues to produce high-resolution images, primarily of soft tissues. MRI relies on a powerful magnetic field that aligns hydrogen protons in the body; when radio-frequency (RF) pulses are applied, these protons are displaced from equilibrium. As the RF field is turned off, protons release energy as they realign, and MRI sensors detect this energy to form images. Tissues in the body return to their equilibrium state at different rates, allowing differentiation between tissue types. Contrast in MRI images is influenced by T1 and T2 relaxation times, which vary across tissues and enhance diagnostic detail. T1-weighted images offer superior anatomical detail, while T2-weighted images highlight pathological changes. Additional techniques like fat suppression and contrast agents, such as gadolinium, further refine imaging by reducing fat signal or enhancing visibility of certain structures, respectively. Pulse sequences like Spin Echo and Gradient Echo are also used to adjust image contrast, optimizing MRI for various clinical needs.5,6
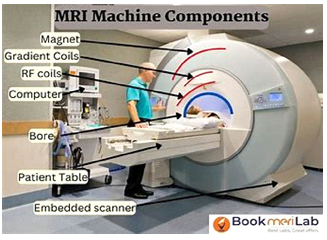
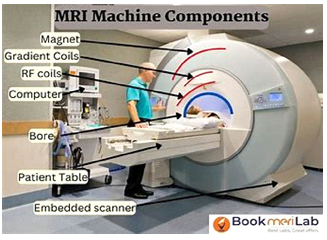
PARTS AND PROCEDURE OF MRI:
An MRI (Magnetic Resonance Imaging) machine consists of several key parts, each with a specific role in creating detailed images of the internal structures. There are main magnet, gradient coils ,radio frequency coils, gradient power amplifiers, computer system and software , cooling system , table .There are two types of magnet : main magnet and gradient coils. The main magnet is the primary and strongest magnet in the MRI machine, typically a superconducting magnet. It creates a strong magnetic field that aligns hydrogen protons in the body.4 Gradient Coils are smaller, additional magnets are used to create slight variations in the main magnetic field, allowing the machine to focus on specific areas of the body.The Radio frequency (RF) Coils has transmit coils and receive coils . Transmit Coils send radio frequency pulses into the body, which cause the aligned hydrogen protons to shift. Receive Coils detect the energy released when the hydrogen protons return to their aligned state, helping to create the image.3,4
Gradient Power Amplifiers power the gradient coils, allowing for precise control of magnetic field gradients during scanning. This is what enables different imaging slices and orientations4. In Computer System and Software , the MRI system is connected to a computer that processes signals from the RF coils and gradient amplifiers. Advanced software reconstructs the data into cross-sectional images. In the Cooling System (Cryogenics), the MRI machines use cryogen-like liquid helium to cool the superconducting magnet. This cooling maintains the magnetic field strength required for high-quality imaging. There is a motorized table in which the patient lies , which slides in and out of the machine to position the body within the magnetic field. These parts work together to generate high-resolution images of internal organs, tissues, and structures, aiding in diagnosis and treatment planning5
MRI TECHNIQUES AND EFFICACY
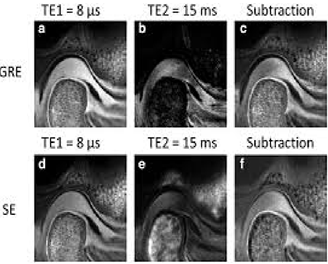
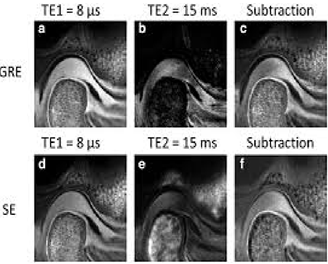
MRI techniques in evaluating Temporomandibular joint disorder (TMD) have advanced, with both static and dynamic MRI approaches offering unique insights into TMJ morphology and function. Static MRI remains the gold standard for assessing articular disc morphology and positional abnormalities, as it provides high-resolution images of both soft and osseous structures, enabling precise visualization of disc displacement, joint effusion, and degenerative changes. Static MRI is particularly useful for evaluating the joint at rest, capturing detailed images that aid in identifying abnormalities in disc structure and surrounding ligaments. However, dynamic MRI has emerged as a complementary technique, particularly useful for assessing condylar movement and disc behavior during jaw function, which provides clinicians with valuable functional insights that static imaging alone cannot offer. Dynamic MRI involves capturing real-time images as the patient performs specific jaw movements, allowing for the assessment of disc dislocation and reduction during function, though it generally has lower spatial resolution than static MRI.7 Despite its functional advantages, dynamic MRI has limitations in capturing the same level of detail as static MRI, making it less reliable for detailed anatomical assessments. Furthermore, MRI field strength plays a crucial role in image quality, with studies indicating that a 1.5T MRI provides significantly better resolution than a 0.55 T MRI, particularly for assessing intrinsic disc morphology and osseous joint structures. The higher magnetic field strength of 1.5T MRI produces clearer, sharper images that enhance diagnostic accuracy, allowing for a more precise assessment of small structural abnormalities that may be critical in TMD diagnosis. Therefore, while dynamic MRI adds valuable information on joint function and disc movement, static MRI, especially at higher field strengths like 1.5 T, remains indispensable for detailed structural assessment in TMD.8
TECHNIQUES AND CLINICAL INSIGHTS
MRI is widely regarded as the reference standard for imaging the Temporomandibular joint (TMJ) due to its superior ability to visualize soft tissue structures such as the articular disc, synovial membrane, and lateral pterygoid muscle, establishing it as the best modality for diagnosing disc displacement scan detect early TMJ dysfunction markers, including thickening of the anterior or posterior disc bands, retro disc tissue rupture, disc shape alterations, and joint effusion, providing critical insight into the onset of pathology . Images can be Sagittal, axial, and coronal planes, with most protocols involving T1-weighted, T2-weighted, and proton-density (PD) sequences. The PD sequence is particularly valuable for assessing the disc-condyle relationship, while T2-weighted images are optimal for identifying joint inflammation.9 Slice thickness often impacts image quality whereas thinner slices improve detail but require longer scan times. MRI acquisition protocols include axial plane that orient the long axis of the condyle in the closed-mouth position, followed by sagittal images perpendicular to this axis and coronal images parallel to it .10 In interpreting these images, disc position is typically lateral to the intermediate zone of the meniscus. A normal disc position is defined in the sagittal plane with the posterior band at approximately the 12 o'clock position relative to the condyle, indicating that the disc sits properly between the condyle and the temporal bone .11 Disc displacement is diagnosed when the posterior band deviates friction, shifting anteriorly, posteriorly, medially, or laterally. For accurate assessments, images should capture the closed-mouth position with teeth in contact and the open-mouth position at the widest comfortable opening, reducing the risk of misinterpreting disc positions12 .Findings suggest that alterations in articular eminence morphology, such as flattening, and changes in disc shape may predispose to disc displacement without reduction on the affected side . These studies reinforce the clinical utility of MRI in diagnosing TMJ disorders associated with disc displacement.13,14
CLINICAL CORRELATIONS IN TMJ MRI FINDINGS
Research demonstrates a significant link between joint pain and specific MRI findings, particularly joint effusion and disc displacement. These findings suggest that patients with visible joint effusion or displaced discs on MRI are more likely to experience joint-related pain. However, this correlation does not hold as strongly for muscle pain, which often shows a weaker association with MRI abnormalities.15 Muscle pain related to TMJ disorders may stem from other factors, such as muscle strain or dysfunction, that MRI is less capable of capturing, indicating that a normal MRI does not rule out muscular sources of pain. Among various disc displacement types, anterior disc displacement without reduction is associated with more pronounced symptoms, including severe pain and restricted mouth opening, compared to other disc positioning abnormalities.16 In anterior disc displacement without reduction, the disc remains displaced during both closed and open-mouth positions, preventing it from returning to its normal position over the condyle17 This persistent misalignment typically leads to mechanical interference and limits the condyle movement, resulting in significant jaw restriction and discomfort. Such cases often require more intensive therapeutic interventions, as anterior disc displacement without reduction can lead to chronic dysfunction and may progress to degenerative changes if untreated.18
APPLICATION OF MRI IN TMJ
Magnetic resonance imaging (MRI) is essential in diagnosing and evaluating Temporomandibular joint (TMJ) disorders, offering detailed anatomical and functional insights into the joint. Recent advancements, such as wireless resonator coils and detainable inserts, have improved MRI's signal-to-noise ratio (SNR), leading to clearer images and enhanced diagnostic capability, particularly at 1.5T . MRI is invaluable for identifying TMJ conditions, including disc displacement, degenerative changes, inflammatory reactions, and muscle pathology. It also plays a critical role in assessing juvenile idiopathic arthritis (JIA), detecting active synovitis even in asymptomatic patients, which enables early intervention. Additionally, MRI provides bio-mechanical insights by dynamically analyzing the articular disc’s position and movement, assisting in diagnosing internal derangement and arthritis within the TMJ. Although MRI is highly effective in visualizing TMJ structures, its use may be limited in cases focused on muscle pain, where clinical evaluation may suffice.2,4,5
IMPLICATIONS FOR DIAGNOSIS IN TMD
MRI serves as a valuable diagnostic tool, especially for patients experiencing joint pain and restricted jaw movement. In these cases, MRI can identify structural abnormalities like disc displacement and joint effusion, which are often associated with joint-specific pain and reduced mobility. However, patients whose primary symptom is muscle pain may derive less benefit from MRI, as muscle-related issues are not always clearly visible on MRI scans. In these instances, other diagnostic approaches, such as clinical examination and Electromyography (EMG), may be more effective in assessing muscle dysfunction and related pain. The development of advanced MRI techniques holds promise for enhancing diagnostic accuracy and treatment planning in TMD. Emerging methods, such as higher-resolution imaging and dynamic MRI protocols, could allow for a more detailed assessment of joint function and soft tissue interactions. Further research is essential to refine these techniques and establish more specific diagnostic criteria, ultimately improving clinical outcomes for TMD patients. Enhanced imaging protocols combined with personalized diagnostic approaches may help healthcare providers make more targeted treatment decisions for complex TMJ disorders.19,20
DISADVANTAGES
MRI, while invaluable in diagnosing TMJ disorders, does come with certain limitations. First, it is both expensive and time-consuming, which can restrict access for some patients. Additionally, MRI’s enclosed structure may be challenging for patients with claustrophobia, potentially making it difficult for them to complete the scan comfortably. Another limitation is MRI's potential to miss specific structural details, such as pseudo cysts on the condyle, which may not be captured fully depending on the imaging plane and technique used. MRI has limitations in detecting certain bone conditions and is less effective at visualizing calcifications or specific inflammatory changes in soft tissues, which are often better detected with CT imaging. In cases of inflammatory diseases, bone pathologies , or suspected tumors, CT may be preferred as it provides more detailed views of bone and calcified structures, making it the superior choice for comprehensive evaluation in these scenarios. However, MRI is not without its limitations. For one, it is less effective at pinpointing muscle-related sources of pain, as MRI findings may not correlate strongly with muscular dysfunction, which is often a significant component of TMD. Additionally, achieving high-quality images typically requires high-field strength MRI machines (1.5 T or greater), which may not be available in all clinical settings due to cost and accessibility constraints.21,22
TYPES OF IMAGES IN MRI23
|
T1-WEIGHTED/FAT IMAGES
|
T2-WEIGHTED/WATER IMAGES
|
|
T1-weighted images are useful for depicting small anatomic region[eg.the TMJ]
|
Images with T2-weighted are most commonly used for inflammatory or other pathogenic changes
|
|
Here fat appears brighter
|
Here water appears brighter
|
INTERPRETATION/APPEARANCE23
- Hyperintense structure-Appear white and bright
- Isointense-Appears grey
- Hypointense-Appears dark,black and produce a weak signal
CONCLUSION
In conclusion, MRI has established itself as a crucial imaging modality in the diagnosis and management of Tempero-mandibular joint disorders (TMD), offering unparalleled visualization of soft tissue structures, such as the articular disc, synovial membrane, and joint effusion. Its ability to reveal disc displacement, joint inflammation, and early degenerative changes makes it a valuable asset in the diagnostic toolkit, especially for patients presenting with joint pain and limited jaw mobility. A thorough clinical assessment, including patient history, physical examination, and functional testing, remains essential to differentiate joint-specific issues from muscle-related conditions. Combining MRI with clinical evaluation allows clinicians to obtain a holistic view of the patient’s symptoms and underlying pathology, leading to more accurate diagnoses and tailored treatment plans. As MRI technology continues to advance, its role in TMD diagnosis may expand; however, clinical judgment and a multidisciplinary approach should always guide the diagnostic and therapeutic process.
REFERENCES
- Y., Balel., Serkan, Yildiz., E., Gokce., MK, Tumer., Bilal, Ege. (2023). 1. Do Temporomandibular Joint Magnetic Resonance Imaging Diagnosis Support Clinical Examination Diagnosis Following Diagnostic Criteria for Temporomandibular Disorders Criteria?. Journal of Oral and Maxillofacial Surgery, doi: 10.1016/j.joms.2023.03.007
- Xin, Xiong., Zheng, Ye., Hehan, Tang., Yi, Wei., Lisha, Nie., Xiaocheng, Wei., Yang, Liu., Bin, Song. (2021). 2. MRI of Temporomandibular Joint Disorders: Recent Advances and Future Directions.. Journal of Magnetic Resonance Imaging, doi: 10.1002/JMRI.27338
- Seyed, Mohammad, H., Gharavi., Yujie, Qiao., Armaghan, Faghihimehr., Josephina, A., Vossen. (2022). 3. Imaging of the Temporomandibular Joint. Diagnostics, doi: 10.3390/diagnostics12041006
- Pragya, Surolia., Jitendra, Kumar, Kumawat., P., Sharma. (2023). 4. Role of Dynamic 3 Tesla MRI in the Evaluation of Temporomandibular Joint Dysfunction. Cureus, doi: 10.7759/cureus.36681
- Shasha, Liu., Lili, Xu., Shenji, Lu., Meng-Ying, Mao., Li-Kun, Liu., Bin, Cai. (2022). 5. Diagnostic performance of magnetic resonance imaging for degenerative temporomandibular joint disease.. Journal of Oral Rehabilitation, doi: 10.1111/joor.13386
- Ismail, Rady, Ismail., Medhat, Mohamed, Rafaat., Ahmed, Shalan. (2020). 6. Role of Magnetic Resonance Imaging in Assessment of Temporomandibular Joint Internal Derangement. doi: 10.21608/BMFJ.2020.86762
- Ahmad, Elsayed, Elnady., Mostafa, Sonble., Ahmed, Abd, El-Salam. (2024). 2. Correlation of Static and Dynamic Magnetic Resonance Imaging Sequences in Evaluation of Temporomandibular Joint Dysfunction. International Journal of Medical Arts (Print), doi: 10.21608/ijma.2023.159913.1506
- Markus, Kopp., Marco, Wiesmueller., Mayte, Buchbender., Marco, R., Kesting., Armin, M., Nagel., Matthias, May., Michael, Uder., Frank, W., Roemer., Rafael, Heiss. (2023). 3. MRI of Temporomandibular Joint Disorders: A Comparative Study of 0.55 T and 1.5 T MRI.. Investigative Radiology, doi: 10.1097/rli.0000000000001008
- Tomas X, Pomes J, Berenguer J, Quinto L, Nicolau C, Mercader JM, et al. MR imaging of temporomandibular joint dysfunction: a pictorial review. Radiographics. 2006;26(3):765–781. doi: 10.1148/rg.263055091.
- Talmaceanu D, Lenghel LM, Bolog N, Hedesiu M, Buduru S, Rotar H, Baciut M, Baciut G. Imaging modalities for temporomandibular joint disorders: an update. Clujul Med. 2018 Jul;91(3):280-287. doi: 10.15386/cjmed-970. Epub 2018 Jul 31. PMID: 30093805; PMCID: PMC6082607.
- Sano T, Widmalm SE, Yamamoto M, Sakuma K, Araki K, Matsuda Y, et al. Usefulness of proton density and T2-weighted vs. T1-weighted MRI in diagnoses of TMJ disk status. Cranio. 2003;21(4):253–258. doi: 10.1080/08869634.2003.11746259.
- Bag AK, Gaddikeri S, Singhal A, Hardin S, Tran BD, Medina JA, et al. Imaging of the temporomandibular joint: An update. World J Radiol. 2014;6(8):567–582. doi: 10.4329/wjr.v6.i8.567.
- Helms CA, Kaplan P. Diagnostic imaging of the temporomandibular joint: recommendations for use of the various techniques. AJR Am J Roentgenol. 1990;154:319–322. doi: 10.2214/ajr.154.2.2105023.
- Drace JE, Enzmann DR. Defining the normal temporomandibular joint: closed-, partially open-, and open-mouth MR imaging of asymptomatic subjects. Radiology. 1990;177:67–71. doi: 10.1148/radiology.177.1.2399340.
- Gibbs SJ, Simmons HC., 3rd A protocol for magnetic resonance imaging of the temporomandibular joints. Cranio. 1998;16(4):236–241. doi: 10.1080/08869634.1998.11746063.
- Hirata FH, Guimarães AS, Oliveira JX, Moreira CR, Ferreira ET, Cavalcanti MG. Evaluation of TMJ articular eminence morphology and disc patterns in patients with disc displacement in MRI. Braz Oral Res. 2007;21(3):265–271. doi: 10.1590/s1806-83242007000300013.
- Alm??an OC, Hede?iu M, B?ciu? G, Leucu?a DC, B?ciu? M. Disk and joint morphology variations on coronal and sagittal MRI in temporomandibular joint disorders. Clin Oral Investig. 2013;17(4):1243–1250. doi: 10.1007/s00784-012-0803-4.
- Sinha VP, Pradhan H, Gupta H, Mohammad S, Singh RK, Mehrotra D, et al. Efficacy of plain radiographs, CT scan, MRI and ultra sonography in temporomandibular joint disorders. Natl J Maxillofac Surg. 2012;3(1):2–9. doi: 10.4103/0975-5950.102138.
- Larheim TA. Current trends in temporomandibular joint imaging. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1995;80(5):555–576. doi: 10.1016/s1079-2104(05)80154-4.
- Goknur, Topaloglu, Yasan., S., Adiloglu., Hakan, Hifzi, Tuz., Dilek, Sahar. (2023). 5. Evaluation of clinical signs and magnetic resonance imaging findings in patients with temporomandibular disorders.. doi: 10.1016/j.jcms.2023.08.013
- Jaqueline, Moreira, Silva., Marly, Barbosa, Maia, Souza., Regina, Paula, Soares, Diego. (2023). 6. Diagnosis of Temporomandibular Disorders by Magnetic Resonance: a narrative review. doi: 10.52600/2965-0968.bjcmr.2023.1.1.30-36
- Sara, Sang., Nazila, Ameli., Fabiana, Tolentino, Almeida., Reid, Friesen. (2024). 1. Association between clinical symptoms and MRI image findings in symptomatic temporomandibular joint (TMJ) disease: A systematic review.. doi: 10.1016/j.jcms.2024.04.006
- Sanjay M.Mallya,Ernest W.N.Lam White and pharoah's oral radiology principals and intrepretaion 2nd south asia edition interpretation amd apperance.


 Dr. T. Vaishnavi*
Dr. T. Vaishnavi*
 Dr. K. Pazhanivel
Dr. K. Pazhanivel
 10.5281/zenodo.14211054
10.5281/zenodo.14211054