Abstract
BACKGROUND: Drug utilization evaluation studies are critical in understanding patient prescription patterns, which help to improve the suitable and efficient use of antibiotics. Studies that evaluate drug use are crucial in determining patient prescription patterns, which aid in improving suitable and efficient use of antibiotics and creating the right guidelines for their use in hospitals. METHODOLOGY: A Prospective observational Study is planned to be conducted on 83 patients admitted to general medicine ward. The study individuals were selected using inclusion and exclusion criteria. Data was collected by evaluating treatment charts of the patients. At the conclusion of the investigation, the acquired data were meticulously compiled and statistically analyses. RESULTS: The study results show the prescribing pattern of antibiotics, where the class of antibiotics were found as 28% of Tetracycline, 18% of Fluroquinolone, 15% of Nitroimidazole, 49% of Cephalosporins, 24% of penicillin’s, 13% of Macrolide. The therapeutic outcomes were recorded in which 67% were cured, 26% was controlled and 6% patients show no improvement. CONCLUSION: The current investigation could evaluate antibiotic prescribing patterns, antibiotic therapeutic outcomes, and culture sensitivity patterns. In the study population, cephalosporins were most often administered antibiotics, followed by tetracyclines. According to the culture sensitivity pattern, streptococcus pneumonia, mycobacterium tuberculosis, and hepatitis A virus were the next most common bacteria found. According to statistical analysis, a patient's age will have an impact on their recovery. In these investigations, the vast majority of patients were healed.
Keywords
Antibiotics; Drug Utilization; Antibiotic Audit; Prescription; General Medicine
Introduction
For decades, antibiotics have been widely used around the world to treat a wide range of bacterial infections because they are strong and efficient medications that combat infectious diseases brought on by bacteria. Since they first came on the scene over fifty years ago, antibiotics have saved millions of lives(1).Antibiotics are drugs that treat bacterial illnesses. Viral infections are unaffected by antibiotics. In the beginning, an antibiotic was a chemical that one microbe created that specifically stopped another from growing. Since then, synthetic antibiotics that perform similar functions have been developed; these are typically chemically related to natural antibiotics.(2) The primary objective is to study the prescribing pattern of antibiotics. The secondary objective is to study the therapeutic outcomes of antibiotics(3).
Classification Of Antibacterial Agents:
Antibiotics can be classified based on chemical structure, bacterial spectrum and mode of action. Antibiotics within the same structural class typically have equal toxicity, effectiveness, and allergy potential. The most often used antibiotic classes include aminoglycosides, penicillins, fluoroquinolones, cephalosporins, macrolides, and tetracyclines. Each pharmaceutical class has unique characteristics, even if it includes multiple drugs(3)
Classification by Chemical Structure:
- Beta-Lactams
- Tetracyclines
- Fluoroquinolones
- Macrolides
- Sulfonamides
- Aminoglycosides
Classification by Mode of Action:
- Bactericidal
- Bacteriostatic
Classification by Spectrum of Activity:
- Narrow-spectrum
- Broad-spectrum
Drug Utilization Evaluation
The regulated, systematic, continuous review of patient medication use, pharmacist dispensing, and healthcare provider prescriptions is known as Drug Utilization Evaluation (DUE)(4). Drug use evaluations examine a patient's prescription and medication data before, throughout, and after treatment to ensure appropriate medication selection and positive patient outcomesand after dispensing(2). Drug therapy is regarded as a key element of patient care in primary healthcare and other healthcare settings. Even while patients benefit much from pharmaceutical therapies, it is impossible to ignore the dangers of medications and the repercussions of improper usage(5). The introduction of powerful medications with a higher risk of adverse drug reactions, the high cost of medication, and a focus on drug use outcomes and clinical misuse of drugs can all result in preventable patient morbidity and mortality, expensive remedial care, additional costs for the diagnosis and treatment of iatrogenic diseases, and unnecessary waste of health resources. Inadequate comprehension of treatment plans and diagnostic proficiency have resulted in poor medication selection, dosage, adverse drug reactions, drug interactions, and overuse of expensive medications when less expensive alternatives might be equally or more effective(2).Drug Utilization Evaluation, or DUE, has been suggested as a way to monitor, assess, and encourage sensible drug therapy in order to detect improper or needless drug use. Increased morbidity, mortality, and medical costs have been linked to a number of issues, including irrational drug usage, polypharmacy, improper drug selection, dosage, and interactions, as well as the use of medications without evidence of efficacy(6). Antibiotic abuse or inappropriate use results in major adverse drug responses, medication resistance, and higher healthcare costs(7). Drug utilization evaluation studies are crucial in determining patient prescription patterns, which aid in the development of appropriate hospital antibiotic usage protocols and the provision of valuable information for bettering the appropriate and efficient use of antibiotics(3). The goal of drug utilization evaluation is to determine the rationale of pharmacological treatment.Methods for auditing pharmacological therapy towards rationality are required to achieve this goal. Descriptive and analytical studies are the two categories of drug utilization evaluation. The former has focused on characterizing drug use patterns and identifying issues that warrant more thorough research(8).Analytical studies link medication use data to statistics on morbidity, treatment outcomes, and service quality to assess the effectiveness of pharmacological therapy(9).
2. MATERIALS AND METHOD:
A Prospective observational Study is planned to be conducted at MVJ Medical College and Research Hospital, Bangalore, South India.After receiving approval from the Institutional Ethical Committee, the study was carried out. Every patient who satisfied the requirements for inclusion was added to the trialto participate in the trial, patients must be at least 18 years old, male or female, admitted to the study site during the study period, and administered antibiotics.& exclusion criteria (those who refuse to participate in the trial and those for whom antibiotics are not provided are excluded). Information on the patient was gathered by looking up lab results, past medication histories, and other pertinent information. Data was gathered by looking at the patients' treatment records. When the study is over, the information gathered will be compiled systematically and will be subjected to statistical analysis. In this study statistical tools like ANOVA and Chi Square were used for the prescribing pattern of antibiotics and MX-excel was performed.
3. RESULTS:
Table 1: Classification By Gender
|
Sl No
|
Gender
|
No. Of Cases (N=83)
|
|
1.
|
Male
|
47
|
|
2.
|
Female
|
36
|
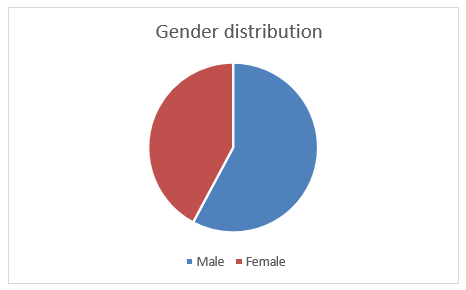
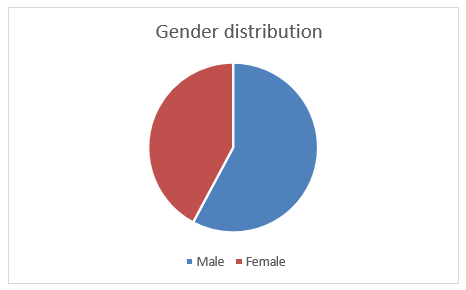
Fig 1: Gender Distribution
According to the study's findings, 43% of the patients were female and 57% of the patients were male.
Table 2: Distribution By Age
|
SL NO
|
Age
|
No. of people prescribed (N=83)
|
|
1.
|
< 20
|
3
|
|
2.
|
20-40
|
29
|
|
3.
|
41-60
|
38
|
|
4.
|
61-80
|
12
|
|
5.
|
>80
|
1
|
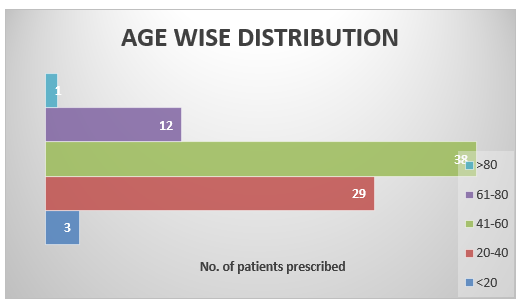
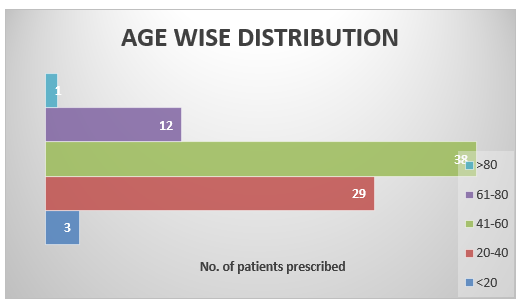
Fig 2: Age Wise Distribution
A review of the patients' age distribution found that 4% of prescriptions were written for patients under the age of 20, 35% for those aged 20 to 40, and 46% forpeople aged 41 to 60, 14% for people aged 61 to 80, and 1% for people above 80.
Table 3: Study Population of Comorbid Conditions
|
Disease Condition
|
No. of patients (N=83)
|
|
Gastro intestinal disorders
|
7
|
|
Diabetes mellitus
|
9
|
|
Viral Fevers
|
23
|
|
Respiratory disorders
|
16
|
|
Renal disorders
|
7
|
|
Liver disorders
|
5
|
|
Cardiovascular diseases
|
3
|
|
CNS disorders
|
2
|
|
Tuberculosis
|
2
|
|
Anemia
|
2
|
|
Hypertension
|
2
|
|
Urinary tract infection
|
5
|
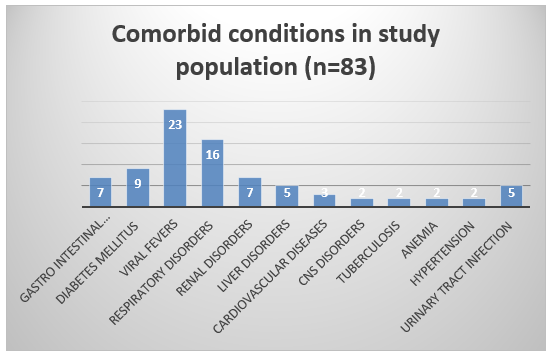
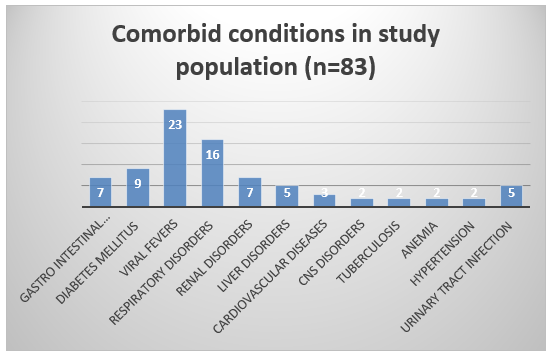
Fig 3: Study population of co morbid conditions
9% of patients had GID, followed by 11% with diabetes, 28% with viral fever, 20% with respiratory disorders, 9% with renal disorders, 6% with liver disorders, 3% with cardiovascular disorders, 2% with central nervous system disorders, 2% with tuberculosis, 2% with anemia, 2% with hypertension, and 6% with urinary tract infections, according to the study on the analysis of co-morbidities of the study population.
Table 4: Classes Of Prescription Antibiotics
|
SL NO
|
Antibiotics
|
No. of prescription (N=83)
|
|
1.
|
Fluroquinolone
|
15
|
|
2.
|
Tetracycline
|
24
|
|
3.
|
Nitroimidazole
|
13
|
|
4.
|
Cephalosporins
|
41
|
|
5.
|
Glycopeptides
|
1
|
|
6.
|
Macrolide
|
11
|
|
7.
|
pencillins
|
20
|
|
8.
|
Sulfonamides
|
1
|
|
9.
|
Lincosamide
|
2
|
|
10.
|
Glycylcyline
|
1
|
|
11.
|
Aminoglycoside
|
1
|
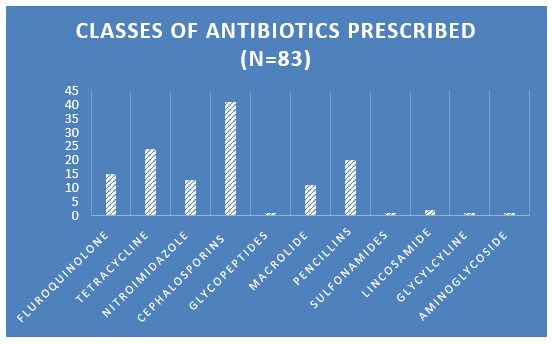
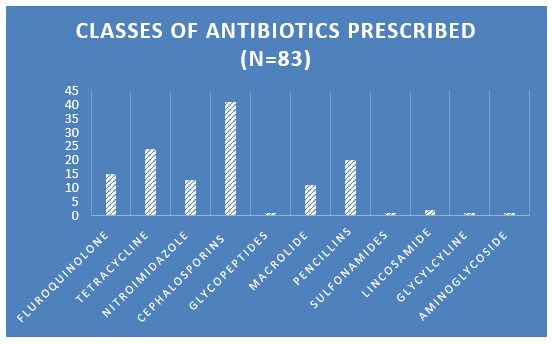
Fig 4: Classes of Antibiotics prescribed
According to the study, cephalosporins accounted for approximately 49% of the antibiotics prescribed to patients, with pencillins (24%), nitroimidazole (15%), fluoroquinolones (18%), and macrolide (13%) coming in second and third, respectively. Lincosamide (2%), sulfonamides (1%), aminoglycosides (1%), Glycylcyline (1%), Tetracyclins (28%), and glycopeptides antibiotics (1%).
Table 5: Total Number of Prescribed Antibiotics (N=83)
|
SL NO
|
No. of Antibiotics
|
No. of patients prescribed (N=83)
|
|
1.
|
1
|
41
|
|
2.
|
2
|
32
|
|
3.
|
3
|
7
|
|
4.
|
4
|
2
|
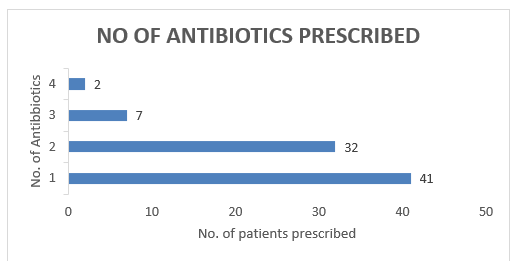
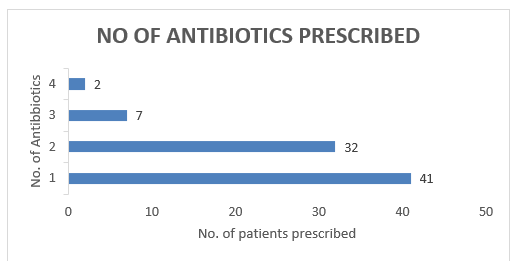
Fig 5: Number of antibiotics prescribed
Most patients were prescribed only one antibiotic throughout their hospital stay, with 41 receiving two, 32 receiving three, and two receiving four.
Table 6: Reason For Antibiotic Prescription (N=83)
|
SI. No.
|
Antibiotics
|
No. of patients prescribed
|
|
1.
|
Prophylaxis
|
13
|
|
2.
|
BPI
|
40
|
|
3.
|
Non- BPI
|
30
|
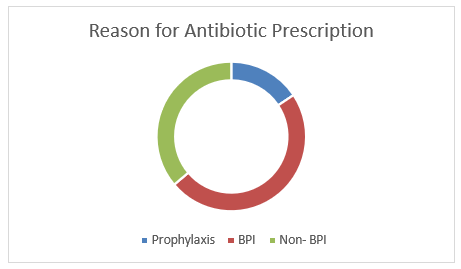
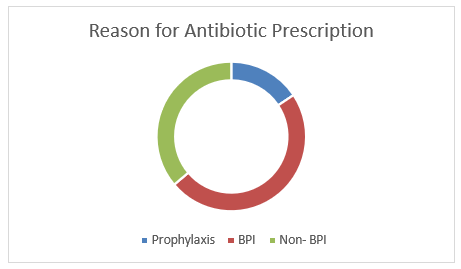
Fig 6: Reason for Antibiotic Prescription
The study found that 48% of patients received antibiotics for Bacteriologically Proven Infection (BPI), 36% for Non-BPI, and 16% for prophylaxis.
Table 7: Antibiotics Therapy Results
|
SI No.
|
Therapy outcomes
|
No. of patients prescribed
|
|
1.
|
Cured
|
56
|
|
2.
|
Controlled
|
22
|
|
3.
|
No improvement
|
5
|
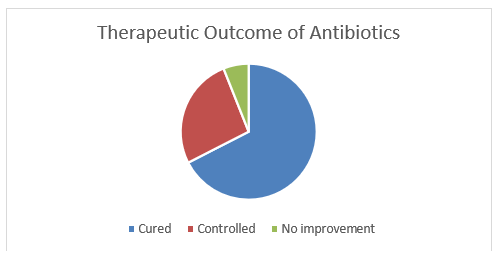
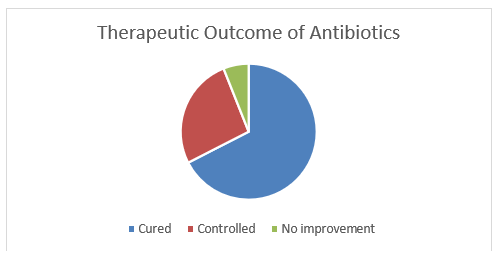
Fig 7: Antibiotic Therapy Results
According to patient reports on the therapeutic effects of antibiotics, around 67% of patients experienced a full recovery from the treatment, 26% demonstrated a controlled response, and 7% exhibited no improvement at all.
Table 8: Therapeutic Outcomes According to The Age (N= 83)
|
Age
|
Therapeutic outcome
|
Therapeutic outcome
|
|
56
|
2
|
Controlled
|
|
45
|
1
|
Cured
|
|
71
|
2
|
Controlled
|
|
58
|
2
|
Controlled
|
|
35
|
2
|
Controlled
|
|
45
|
1
|
Cured
|
|
30
|
1
|
Cured
|
|
35
|
2
|
Controlled
|
|
48
|
1
|
Cured
|
|
54
|
2
|
Controlled
|
|
27
|
2
|
Controlled
|
|
23
|
1
|
Cured
|
|
30
|
2
|
Controlled
|
|
19
|
1
|
Cured
|
|
43
|
3
|
No improvement
|
|
45
|
1
|
Cured
|
|
65
|
1
|
Cured
|
|
50
|
1
|
Cured
|
|
42
|
3
|
No improvement
|
|
48
|
1
|
Cured
|
|
49
|
1
|
Cured
|
|
45
|
1
|
Cured
|
|
59
|
2
|
Controlled
|
|
65
|
1
|
Cured
|
|
66
|
3
|
No improvement
|
|
42
|
1
|
Cured
|
|
44
|
1
|
Cured
|
|
29
|
1
|
Cured
|
|
35
|
1
|
Cured
|
|
40
|
1
|
Cured
|
|
64
|
2
|
Controlled
|
|
50
|
1
|
Cured
|
|
23
|
1
|
Cured
|
|
69
|
2
|
Controlled
|
|
56
|
3
|
No improvement
|
|
31
|
1
|
Cured
|
|
48
|
1
|
Cured
|
|
19
|
1
|
Cured
|
|
49
|
1
|
Cured
|
|
56
|
2
|
Controlled
|
|
23
|
1
|
Cured
|
|
58
|
1
|
Cured
|
|
66
|
2
|
Controlled
|
|
35
|
1
|
Cured
|
|
31
|
1
|
Cured
|
|
38
|
1
|
Cured
|
|
21
|
1
|
Cured
|
|
54
|
2
|
Controlled
|
|
34
|
1
|
Cured
|
|
55
|
2
|
Controlled
|
|
35
|
1
|
Cured
|
|
19
|
1
|
Cured
|
|
39
|
1
|
Cured
|
|
65
|
2
|
Controlled
|
|
64
|
3
|
No improvement
|
|
31
|
1
|
Cured
|
|
54
|
1
|
Cured
|
|
70
|
2
|
Controlled
|
|
56
|
1
|
Cured
|
|
47
|
2
|
Controlled
|
|
29
|
1
|
Cured
|
|
46
|
1
|
Cured
|
|
83
|
1
|
Cured
|
|
42
|
2
|
Controlled
|
|
31
|
1
|
Cured
|
|
35
|
1
|
Cured
|
|
34
|
1
|
Cured
|
|
34
|
2
|
Controlled
|
|
59
|
1
|
Cured
|
|
48
|
1
|
Cured
|
|
38
|
1
|
Cured
|
|
61
|
1
|
Cured
|
|
47
|
1
|
Cured
|
|
48
|
2
|
Controlled
|
|
31
|
1
|
Cured
|
|
58
|
1
|
Cured
|
|
53
|
1
|
Cured
|
|
72
|
1
|
Cured
|
|
38
|
1
|
Cured
|
|
28
|
1
|
Cured
|
|
56
|
1
|
Cured
|
|
43
|
1
|
Cured
|
|
46
|
2
|
Controlled
|
Table 8A: Therapeutics Outcomes According to The Age
|
Anova: Single Factor
|
|
|
|
|
|
|
|
SUMMARY
|
|
|
|
|
|
|
|
Groups
|
Count
|
Sum
|
Average
|
Variance
|
|
|
|
Age
|
83
|
3763
|
45.33735
|
206.9092
|
|
|
|
Therapeutic outcome no
|
83
|
115
|
1.385542
|
0.36174
|
|
|
|
ANOVA
|
|
|
|
|
|
|
|
Source of Variation
|
SS
|
df
|
MS
|
F
|
P-value
|
Significance F
|
|
Between Groups
|
80168.1
|
1
|
80168.1
|
773.5585
|
5.6
|
3.89
|
|
Within Groups
|
16996.22
|
164
|
103.6355
|
|
|
|
| |
|
|
|
|
|
|
|
Total
|
97164.31
|
165
|
|
|
|
|
After the statistical study was completed, the following findings were observed: Every group shares the same continuous variable mean. H1: At least one group has a different continuous variable mean. Therefore, age has an impact on patients' ability to recuperate.
Table 9: Factors Affecting Number of Antibiotics Prescribed (N=83)
|
|
N
|
1
Antibiotic
|
2
Antibiotics
|
3
Antibiotics
|
|
Gender
Male
Female
|
47
36
|
24
18
|
19
14
|
4
4
|
|
Age
<20
21-40
41-60
61-80
>80
|
3
29
38
12
1
|
2
12
18
6
1
|
1
14
16
4
|
3
4
2
|
|
Stay Period
<5 days
5 days
>5 days
|
36
27
17
|
25
11
10
|
15
10
5
|
6
6
2
|
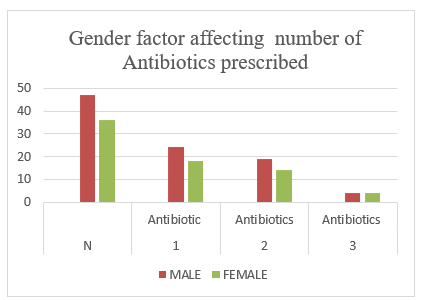
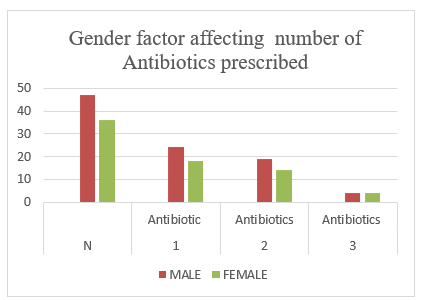
Fig 9A: Gender factor affecting the number of antibiotics prescribed
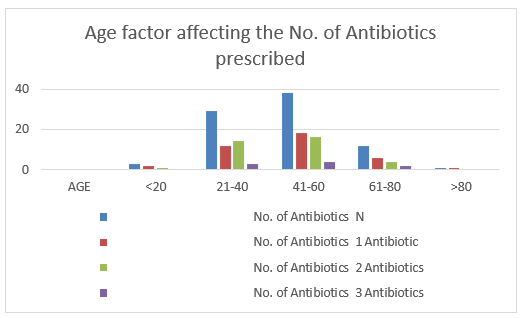
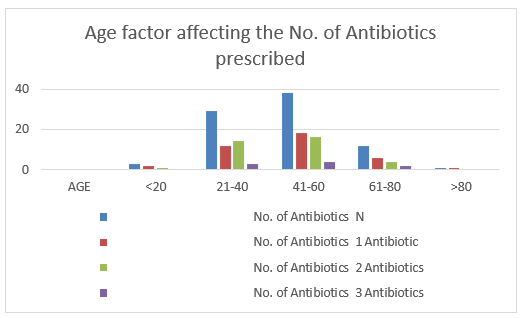
Fig 9B: Age factor affecting the No. of Antibiotics prescribed
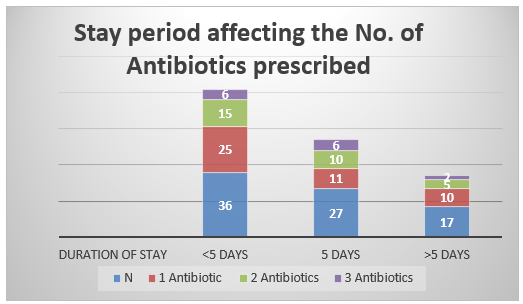
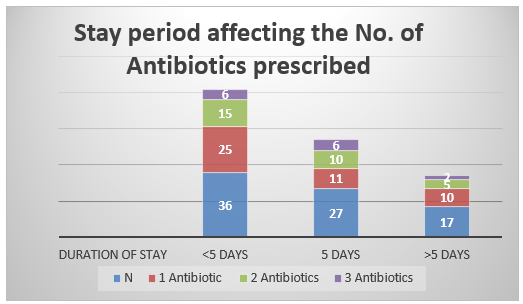
Fig 9C: Stay period affecting the No. of Antibiotics prescribed
The study linked the amount of antibiotics prescribed to gender, age, and duration of therapy, and it was shown that the majority of patients were prescribed only one antibiotic. In terms of gender, 24 males and just 18 females were administered single antibiotics. Compared to other age groups, the majority of patients aged 21-40 and 41-60 were prescribed a single antibiotic during the research.
Table 10: Organisms Isolated
|
SL NO
|
Organisms
|
No. of patients
|
|
1.
|
Streptococcus pneumonia
|
5
|
|
2.
|
E. coli
|
6
|
|
3.
|
Hepatitis A virus
|
1
|
|
4.
|
Mycobacterium tuberculosis
|
2
|
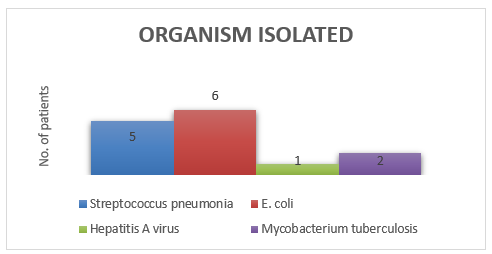
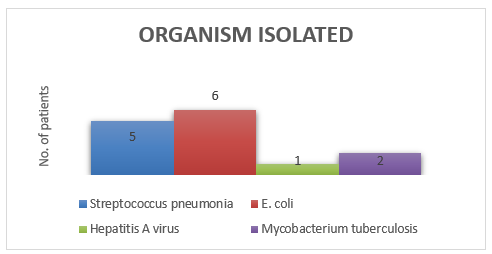
Fig 10: Organism Isolated
The study presents many strains of organisms identified from the patient's culture test. Streptococcus pneumoniae was the most prevalent isolated organism, accounting for 35%, followed by E.coli 42%, Hepatitis A virus 7%, and Mycobacterium tuberculosis 14%.
Table 11: Culture Sensitivity Specimen
|
SL NO
|
Specimen
|
No. of patients
|
|
1.
|
Sputum
|
7
|
|
2.
|
Urine
|
6
|
|
3.
|
Blood
|
1
|
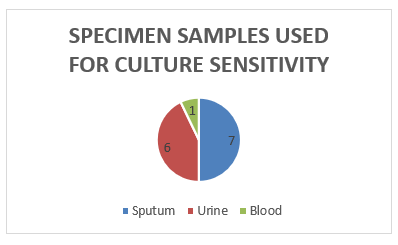
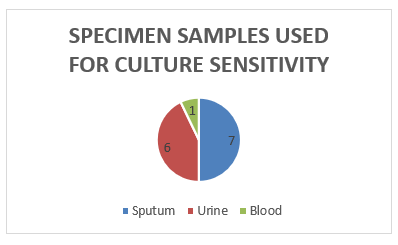
Fig 11: Culture Sensitivity Specimen
The specimens used in the culture sensitivity test were sputum (43%), urine (7%), and blood (50%).
4. DICUSSION:
The current study on gender categorization found that men made up the majority of the study population.A comparable study by Ravi Pathiyil Shankar et al. (2003) discovered that the majority of patients were men. An examination of the age distribution found that the bulk of prescriptions were written for those between the ages of 21 and 40, followed by those aged 41 to 60.Mujtaba Hussain et al. (2014) observed that the majority of prescriptions were for people aged 46 to 60. In the current study, categorization based on co morbid illnesses was examined, and it was discovered that the majority of patients had viral fever, which was consistent with a study conducted by Mohanraj Rathinavelu et al (2015), who stated that the majority of patients had urinary tract infection(3). Cephalosporins and tetracyclines were the two most commonly prescribed antibiotics to patients, according to the current study. This study was similar to one conducted by Venu Gopal D et al. (2014), who discovered that cephalosporins were predominantly prescribed to inpatients and penicillin usage was highest in outpatients. Ceftriaxone (24.6%) and piperacillin/tazobactum (40.6%) were the most often provided antibiotics during hospitalization, according to a comparable study by Meher B. R. et al. (2014). In line with a study by R Selvaraj et al. (2015), the majority of prescriptions (48.6%) contained only one antibiotic.(10) The current study, like a study conducted by Ravi Pathiyil Shankar et al. (2003), found that the majority of patients were recommended antibiotics for BPI(3). 67% of patients were fully healed by the therapy, 26% of patients showed a controlled response to the therapy, and 7% of patients showed no improvement, according to reports on therapeutic outcomes throughout the hospital stay. Shalem Lakkepogu et al. (2014) conducted a similar study and found that the majority of patients were cured, with only a few individuals failing to respond(3). Streptococcus pneumoniae was the most frequently observed organism in the study, followed by E. coli, Hepatitis A virus, and mycobacterium tuberculosis. This was analogous to the study conducted by Ravi Pathiyil Shankar et al. (2003), who set up that the most constantly insulated species were H.Influenzae, E. coli, K. pnemoniae, and S. aureus. Sputum, urine, blood, tracheal culture, and pus are the instance samples used in this study to assess antibiotic perceptivity patterns.The antibiotic perceptivity pattern was examined, and the results were set up to be analogous to the study conducted by Bijoy Thomas et al (2014) forreporting antibiotic perceptivity patterns exercising urine, trachea, pus, foam, and throat tar.Bijoy Thomas et al. (2014) set up that E.coli is sensitive to Amikacin, which are the Klebsiella, Amikacin, Pseudomonas and Meropenem respectively.(3)
5. Limitation:
There are also a few shortcomings in the current review paper. The cost of DUE treatments was not included in the analysis. This review paper's primary focus was on DUE procedures and techniques, which may limit and differ from other research. Additionally, there has been no mention of any ADR pertaining to DUE in this evaluation. We didn't cover additional metrics like bacterial infections, therapeutic results, or patient care indicators; we just talked about prescription indicators. This review also makes no mention of the pharmacist's role in DUE.
6. CONCLUSION:
The current investigation could evaluate antibiotic prescribing patterns, antibiotic sensitivity patterns, antibiotic side effects, and medication interactions. Cephalosporins were the most often administered antibiotics in the study population, with tetracyclines coming in second. Streptococcus pneumonia was shown to be highly detectable, followed by E. coli, Hepatitis A virus, and Mycobacterium TB, according to the culture sensitivity pattern. The ADRs and Drug interactions were not observed in these studies. By the statistical analysis it was found that the age factor will affect the recovery of the patients. The majority of the patients were cured in these studies. Clinicians and clinical pharmacists must play a key role in reducing antibiotic issues by implementing ongoing education campaigns about the most recent hospital prescription guidelines and reducing antibiotic resistance. For safety and medication monitoring, it is strongly advised that clinical pharmacists actively participate in clinical ward rounds and record their observations on prescriptions in patient folders. Additionally, doctors need to be well-versed in the prudent therapeutic use of antibiotics. They must exercise sound judgment when selecting antibiotic regimens and be aware of the prevalence of various diseases and resistance tendencies in their facility. Irrationality can be combated through guidelines, instructional programs, and observation at all levels of healthcare. As a result, care should be taken to avoid the incorrect use of antibiotics. To evaluate the wise use of antibiotics, a drug use review procedure must be established.
REFERENCES
- Govind Naik H, Khanwelkar CC, Kolur A, Desai R, Gidamudi S. National Journal Of Medical Research Drug Utilization Study On Antibiotics Use In Lower Respiratory Tract Infection.
- Soltani R, Hakamifard A, Mousavi S, Amani Z. Drug Utilization Evaluation of Antibiotics in Intensive Care Units of a Referral Teaching Hospital. Vol. 9, J Pharm Care. 2021.
- Chitra MB, Pharm M. CERTIFICATE.
- Rajini S, Venkateswarulu B. Drug Use Evaluation of Antibiotics In Non-Teaching Tertiary Care Hospital [Internet]. Vol. 1, World Journal of Current. Available from: https://www.wjcmpr.com
- Jayakar DB, Aleykutty DNA, Santhosh DR, Mathews M. Evaluation of Oral Antibiotic Utilization In Medical Inpatients.
- Rajini S, Venkateswarulu B. Drug Use Evaluation of Antibiotics In Non-Teaching Tertiary Care Hospital [Internet]. Vol. 1, World Journal of Current. Available from: https://www.wjcmpr.com
- Thomas AP, Kumar M, Johnson R, More SP, Panda BK. Evaluation of antibiotic consumption and compliance to hospital antibiotic policy in the surgery, orthopedics and gynecology wards of a tertiary care hospital. Clin Epidemiol Glob Health. 2022 Jan 1;13.
- Bithi SS, Minhazur M, Khan R, Khan AU. Drug utilization study in orthopaedic units: Antibiotics prescribed in hospital out-patients in Dhaka, Bangladesh [Internet]. Vol. 3, International Current Pharmaceutical Journal. 2014. Available from: http://www.icpjonline.com/documents/Vol3Issue9/01.pdf
- Kaur S, Rajagopalan S, Kaur N, Shafiq N, Bhalla A, Pandhi P, et al. Drug Utilization Study in Medical Emergency Unit of a Tertiary Care Hospital in North India. Emerg Med Int. 2014;2014:1–5.
- Kala K, Sodhi RK, Jain UK. Drug utilization evaluation of antibiotics in district hospital Rudraprayag. Journal of Drug Delivery and Therapeutics. 2018 Nov 15;8(6):87–90.


 Rashmitha R.*
Rashmitha R.*
 Sahana G.
Sahana G.
 Beulah Milton
Beulah Milton
 10.5281/zenodo.15576994
10.5281/zenodo.15576994