Abstract
Urticaria, commonly known as hives, is a dermatological condition marked by transient wheals, itching, and sometimes angioedema. It affects a significant portion of the population, with chronic urticaria presenting unique diagnostic and therapeutic challenges. This review explores the multifactorial etiology of urticaria, which includes physical factors, infections, autoimmune responses, and idiopathic causes. The pathophysiology primarily involves mast cell activation and histamine release, leading to the characteristic symptoms. Urticaria is classified into spontaneous and inducible forms, each with specific triggers and clinical presentations. Management strategies are diverse, encompassing first-line treatments with antihistamines, and advancing to immunomodulatory therapies such as omalizumab for chronic cases. Herbal and plant-based treatments, dietary modifications, and lifestyle changes, including yoga and stress management, are also integral to a comprehensive treatment approach. This review emphasizes the importance of individualized care and the potential benefits of integrating complementary therapies. Further research into the mechanisms and treatment options for urticaria is essential for improving patient outcomes and quality of life.
Keywords
Urticaria, Chronic Urticaria, Mast Cell Activation, Antihistamines, Herbal Medicine, Diet, Yoga, Complementary Therapies.
Introduction
Urticaria, commonly known as hives, is a prevalent dermatological condition characterized by transient, pruritic wheals and, in some cases, angioedema. These lesions typically appear as red or skin-colored swellings on the skin, varying in size and shape, and often accompanied by intense itching. The condition can be acute or chronic, with chronic urticaria (CU) defined as episodes persisting for six weeks or more. Chronic urticaria can be particularly distressing, significantly impacting patients' quality of life due to its persistent and often unpredictable nature. Epidemiology and Impact
Urticaria affects approximately 15-20% of the population at some point in their lives, with chronic urticaria impacting about 1-3% of individuals. Women are more commonly affected than men, and the condition can occur at any age, though it is most prevalent in adults. The unpredictable nature of urticaria, coupled with the potential for recurrent and chronic symptoms, poses a substantial burden on both patients and healthcare systems. The impact on quality of life is profound, often affecting sleep, daily activities, and emotional well-being.
Pathophysiology and Classification
The pathophysiology of urticaria involves complex interactions between immune cells, mast cells, and various triggers, leading to the release of histamine and other mediators that cause the characteristic wheals and itching. Urticaria is classified into two main types: spontaneous (idiopathic) and inducible. Spontaneous urticaria includes both acute and chronic forms, where the triggers are not easily identifiable. Inducible urticaria, on the other hand, is triggered by specific physical or environmental factors such as pressure, temperature changes, or sunlight.
Challenges in Management
Despite advances in understanding the underlying mechanisms of urticaria, managing chronic urticaria remains challenging. The first-line treatment typically involves H1-antihistamines, but many patients experience inadequate relief, necessitating the use of higher doses or additional therapies. Recent years have seen the exploration of alternative and complementary therapies, including dietary modifications, herbal medicine, and psychological interventions, to manage refractory cases.
Purpose and Scope of the Review
This review aims to provide a comprehensive overview of the current understanding of urticaria, with a particular focus on innovative and alternative management strategies. We will discuss the epidemiology, pathophysiology, and classification of urticaria, followed by an in-depth examination of traditional and emerging treatments. Special attention will be given to the role of diet, herbal remedies, and lifestyle modifications in managing chronic urticaria. By synthesizing recent research and clinical experiences, this review seeks to offer practical insights and recommendations for clinicians and researchers involved in the care of patients with urticaria. [1-8]
ETIOLOGY OF URTICARIA
Urticaria, commonly referred to as hives, is a complex condition with a diverse range of etiological factors. The etiology of urticaria involves both external and internal triggers that can activate mast cells, leading to the release of histamine and other inflammatory mediators. Understanding the underlying causes is crucial for effective management and treatment. The etiological factors can be broadly categorized into physical factors, infections, autoimmune disorders, medications, and idiopathic causes.
- Physical Factors
Physical urticaria is triggered by specific physical stimuli, and it accounts for approximately 15% of all urticaria cases. The following are common types of physical urticaria:
Dermatographism: Triggered by firm stroking or scratching of the skin, leading to linear wheals at the site of contact.
Delayed Pressure Urticaria: Occurs several hours after sustained pressure on the skin, such as from tight clothing or prolonged sitting.
Cold Urticaria: Induced by exposure to cold temperatures, leading to wheal formation in affected areas.
Cholinergic Urticaria: Triggered by an increase in body temperature due to exercise, hot showers, or stress, resulting in small, itchy wheals.
Solar Urticaria: Caused by exposure to sunlight, particularly ultraviolet rays.
Vibratory Urticaria: Triggered by vibration, such as from using power tools.
2. Infections
Infections, both bacterial and viral, are known triggers of urticaria. Although the association between infections and urticaria can sometimes be coincidental, several pathogens have been implicated:
Viral Infections: Viruses such as Hepatitis B, Herpes simplex, and Epstein-Barr have been associated with urticaria.
Bacterial Infections: Streptococcal and Mycoplasma species are commonly reported bacterial triggers.
Parasitic Infections: Parasitic infestations, such as those caused by Giardia lamblia and Strongyloides stercoralis, can lead to urticarial reactions.
3. Autoimmune Disorders
Autoimmune mechanisms play a significant role in the pathogenesis of chronic urticaria. Autoimmune urticaria is characterized by the presence of autoantibodies that target the high-affinity IgE receptor (Fc?RI) on mast cells or IgE itself. This immune response leads to mast cell activation and histamine release. Conditions associated with autoimmune urticaria include:
Autoimmune Thyroid Disease: Disorders such as Hashimoto's thyroiditis and Graves' disease are commonly associated with chronic urticaria.
Systemic Lupus Erythematosus: A systemic autoimmune condition that can present with urticarial lesions.
Rheumatoid Arthritis and Other Connective Tissue Diseases: These conditions can sometimes present with urticaria as a secondary manifestation.
4. Medications
Medications are a well-known cause of urticaria, with some drugs more commonly implicated than others. The following categories of medications are frequently associated with urticarial reactions:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These can exacerbate or trigger urticaria, particularly in individuals with aspirin sensitivity.
Antibiotics: Penicillins, sulfonamides, and cephalosporins are common culprits.
Opioids: Can induce urticaria by directly releasing histamine from mast cells.
ACE Inhibitors: Commonly used for hypertension and heart failure, these can occasionally cause urticarial reactions.
5. Idiopathic Causes
In many cases, the specific cause of urticaria remains unidentified, and these cases are classified as idiopathic. Idiopathic urticaria can be challenging to manage, as it often involves an unknown or unidentifiable trigger. Autoimmune mechanisms are suspected in a significant proportion of idiopathic cases, where autoantibodies target mast cells or IgE.
PATHOPHYSIOLOGY AND SYMPTOMS OF URTICARIA
Pathophysiology
Urticaria, or hives, is primarily characterized by the sudden onset of wheals, angioedema, or both. The underlying pathophysiological mechanisms involve complex interactions between the immune system, mast cells, and various triggers. The hallmark of urticaria is the activation and degranulation of mast cells, leading to the release of histamine and other pro-inflammatory mediators.
1. Mast Cell Activation
Mast cells play a central role in the pathogenesis of urticaria. These cells are widely distributed throughout the skin, mucosal tissues, and other organs. Upon activation, mast cells release a variety of mediators, including histamine, prostaglandins, leukotrienes, cytokines, and proteases. These mediators contribute to the clinical manifestations of urticaria, such as vasodilation, increased vascular permeability, and sensory nerve activation.
Histamine: The primary mediator in urticaria, histamine causes vasodilation and increased permeability of blood vessels, leading to the characteristic wheals. It also stimulates sensory nerves, causing pruritus (itching).
Leukotrienes and Prostaglandins: These lipid mediators enhance vascular permeability and contribute to inflammation and pain.
2. Immunological Mechanisms
Urticaria can be mediated by both immunological and non-immunological mechanisms. The immunological mechanisms are typically classified into:
IgE-Mediated Reactions: In some cases, urticaria results from type I hypersensitivity reactions, where specific IgE antibodies bind to allergens and cross-link the high-affinity IgE receptors (Fc?RI) on mast cells, leading to degranulation.
Autoimmune Mechanisms: Autoimmune urticaria involves the presence of autoantibodies that target Fc?RI or IgE itself, causing chronic activation of mast cells even in the absence of external allergens.
3. Non-Immunological Triggers
In addition to immune-mediated mechanisms, urticaria can also occur due to non-immunological triggers, which include:
Direct Mast Cell Activators: Certain substances, such as drugs (e.g., opioids, radiocontrast agents) and physical factors (e.g., pressure, temperature changes), can directly activate mast cells without involving IgE antibodies.
Pseudoallergens: These are substances that mimic the action of allergens but do not involve specific IgE antibodies. They can include certain food additives, preservatives, and medications.
Symptoms
The clinical presentation of urticaria is highly variable, with symptoms ranging from mild to severe. The primary symptoms include:
1. Wheals (Hives)
Wheals are the most characteristic feature of urticaria. They appear as raised, erythematous (red), and edematous (swollen) lesions on the skin. Wheals can vary in size from a few millimeters to several centimeters and may merge to form larger areas of affected skin.
Shape and Distribution: Wheals can be round, oval, or irregularly shaped. They typically have a central clearing and a well-defined border. Wheals can occur anywhere on the body, including the face, trunk, limbs, and scalp.
Duration: Individual wheals usually resolve within 24 hours without leaving any marks, but new wheals can appear as older ones fade, leading to a continuous cycle of symptoms in chronic cases.
Pruritus (Itching): Itching is a prominent symptom of urticaria and can be intense, causing significant discomfort.
2. Angioedema
Angioedema is the swelling of the deeper layers of the skin and mucous membranes, often occurring alongside wheals. It is most commonly seen on the face, particularly around the eyes and lips, and can also affect the tongue, throat, and genitals.
Characteristics: Unlike wheals, angioedema is typically non-erythematous (not red) and can be more painful than itchy. It tends to last longer than wheals, often persisting for up to 72 hours.
Severity: Severe cases of angioedema, especially when involving the airway or gastrointestinal tract, can be life-threatening and require immediate medical attention.
3. Systemic Symptoms
In some cases, urticaria can be accompanied by systemic symptoms such as:
Fever
Malaise
Joint Pain
Abdominal Pain
Headache
These symptoms are more common in cases of urticarial vasculitis, a related condition characterized by longer-lasting lesions and systemic involvement.
CLASSIFICATION OF URTICARIA
Urticaria, or hives, is a heterogeneous condition characterized by different clinical patterns and underlying causes. Proper classification of urticaria is essential for diagnosis, treatment, and management. The condition is broadly categorized into spontaneous and inducible urticaria, with further subdivisions based on duration, triggers, and underlying pathophysiological mechanisms.
1. Spontaneous Urticaria
Spontaneous urticaria, also known as idiopathic urticaria, occurs without identifiable external triggers. It is further classified based on the duration of symptoms:
Acute Urticaria
Definition: Acute urticaria is defined as the occurrence of urticaria symptoms (wheals, angioedema, or both) for less than six weeks.
Etiology: Common triggers include infections, medications, foods, and environmental allergens. In many cases, the cause remains unidentified.
Clinical Features: Symptoms typically resolve within a few hours to days. Acute urticaria is often self-limiting and may not require extensive investigation unless symptoms are severe or recurrent.
Chronic Urticaria
Definition: Chronic urticaria (CU) is characterized by the presence of urticaria symptoms for six weeks or longer. It can be further divided into chronic spontaneous urticaria (CSU) and chronic inducible urticaria (CIU).
Chronic Spontaneous Urticaria (CSU): In CSU, symptoms occur without specific external triggers. Autoimmune mechanisms, infections, and other systemic conditions are potential contributing factors.
Clinical Features: CSU is often challenging to manage due to the chronic and unpredictable nature of symptoms. Patients may experience daily or intermittent wheals and angioedema.
2. Inducible Urticaria
Inducible urticaria, also known as physical urticaria, occurs in response to specific physical or environmental stimuli. This category includes several distinct subtypes:
Dermatographism
Definition: Dermatographism, or "skin writing," is characterized by the development of linear wheals following firm stroking or scratching of the skin.
Clinical Features: The wheals typically appear within minutes and resolve within 30 minutes to an hour. Dermatographism is one of the most common forms of inducible urticaria.
Cold Urticaria
Definition: Cold urticaria is triggered by exposure to cold temperatures, including cold air, water, or objects.
Clinical Features: Symptoms include wheals, angioedema, and itching at the site of cold exposure. In severe cases, systemic reactions such as anaphylaxis can occur, particularly with generalized cold exposure (e.g., swimming in cold water).
Cholinergic Urticaria
Definition: Cholinergic urticaria is induced by an increase in body temperature, such as during exercise, hot showers, or emotional stress.
Clinical Features: This subtype is characterized by small, punctate wheals surrounded by erythema, often accompanied by intense itching. Symptoms typically resolve within an hour.
Solar Urticaria
Definition: Solar urticaria is caused by exposure to sunlight, particularly ultraviolet (UV) light.
Clinical Features: Symptoms include erythema, wheals, and itching in exposed areas. Onset is usually rapid, occurring within minutes of sun exposure.
Pressure Urticaria
Definition: Pressure urticaria, or delayed pressure urticaria, occurs after sustained pressure on the skin, such as from tight clothing or prolonged sitting.
Clinical Features: Symptoms include deep, painful swelling and wheals that develop hours after the pressure is applied. The symptoms can persist for several hours to days.
Aquagenic Urticaria
Definition: Aquagenic urticaria is a rare form triggered by contact with water, regardless of its temperature.
Clinical Features: Patients develop small wheals and itching after water exposure. This form of urticaria is particularly challenging as water is a ubiquitous substance.
3. Urticarial Vasculitis
Urticarial vasculitis is a distinct entity characterized by inflammation of the blood vessels in the skin. It presents with urticarial lesions that last longer than 24 hours and may leave hyperpigmentation or purpura as they resolve. Urticarial vasculitis is often associated with systemic symptoms such as fever, joint pain, and abdominal pain. It can be idiopathic or associated with autoimmune diseases like systemic lupus erythematosus or infections.
MANAGEMENT AND TREATMENTS OF URTICARIA
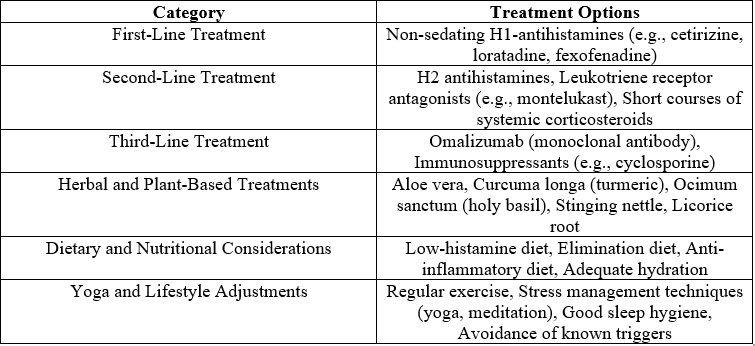
Table 1 strategies for managing and treating urticaria
The management of urticaria involves a multifaceted approach tailored to the individual's specific type and severity of symptoms. This includes pharmacological interventions, lifestyle modifications, and alternative therapies. The goal is to alleviate symptoms, improve quality of life, and, when possible, address the underlying causes. Here, we provide an overview of traditional treatments along with herbal and plant-based therapies, dietary and nutritional considerations, and the role of yoga and lifestyle changes in managing urticaria.
Pharmacological Treatments
First-Line Treatments
Antihistamines: Non-sedating H1-antihistamines are the first-line treatment for urticaria. These drugs block the effects of histamine, the main mediator of symptoms. Common options include cetirizine, loratadine, and fexofenadine. Higher doses may be used in cases where standard doses are ineffective.
Second-Line Treatments
H2 Antihistamines: These can be added to H1-antihistamines in resistant cases, targeting different histamine receptors involved in urticaria.
Leukotriene Receptor Antagonists: Medications like montelukast may be used, especially in cases linked to NSAID sensitivity.
Corticosteroids: Short courses of systemic corticosteroids can be effective for acute flare-ups but are not recommended for long-term use due to potential side effects.
Third-Line Treatments
Omalizumab: This monoclonal antibody targets IgE and is used for chronic spontaneous urticaria (CSU) that is unresponsive to antihistamines.
Immunosuppressants: In severe cases, drugs like cyclosporine may be considered.
Herbal and Plant-Based Treatments
Herbal medicine offers a complementary approach to managing urticaria, focusing on natural compounds that possess anti-inflammatory, antihistamine, and immunomodulatory properties. Here are some commonly used herbs:
Aloe Vera: Known for its soothing properties, aloe vera gel can be applied topically to alleviate itching and inflammation.
Curcuma Longa (Turmeric): Contains curcumin, a compound with potent anti-inflammatory effects. It can be consumed as a supplement or incorporated into the diet.
Ocimum Sanctum (Holy Basil): Has anti-inflammatory and antihistaminic properties. It can be taken as a tea or supplement.
Stinging Nettle (Urtica dioica): Traditionally used for its antihistamine effects, nettle can be consumed as a tea or in capsule form.
Licorice Root: Known for its anti-inflammatory and immune-boosting properties, licorice root can be taken as a supplement.
While herbal remedies can be beneficial, it is crucial to consult healthcare professionals before starting any new treatment, especially for individuals with allergies or those taking other medications.
Diet and Nutrition
Diet plays a significant role in managing urticaria, particularly for individuals with food sensitivities or intolerances. Here are some dietary guidelines and considerations:
Low-Histamine Diet: For individuals with histamine intolerance, a low-histamine diet can be beneficial. This involves avoiding foods high in histamine, such as aged cheeses, fermented foods, smoked meats, and certain fish.
Elimination Diet: This approach involves eliminating potential trigger foods from the diet and gradually reintroducing them to identify specific allergens.
Anti-Inflammatory Diet: Emphasizes the consumption of fruits, vegetables, whole grains, and healthy fats (e.g., omega-3 fatty acids) to reduce overall inflammation.
Hydration: Adequate hydration is essential for overall health and can help manage urticaria symptoms by supporting skin hydration and function.
Yoga and Lifestyle
Lifestyle modifications, including stress management and physical activity, can play a crucial role in managing urticaria. Stress, in particular, is known to exacerbate symptoms in many individuals.
Yoga and Relaxation Techniques
Yoga: Regular practice of yoga can help reduce stress, improve circulation, and enhance overall well-being. Specific poses that may be beneficial include:
Matsyasana (Fish Pose): Promotes relaxation and deep breathing.
Trikonasana (Triangle Pose): Improves flexibility and reduces muscle tension.
Bhujangasana (Cobra Pose): Helps open the chest and relieve stress.
Breathing Exercises (Pranayama): Techniques like deep breathing, Bhastrika (bellows breath), and Anulom Vilom (alternate nostril breathing) can help manage stress and anxiety, which are common triggers for urticaria.
Lifestyle Adjustments
Regular Exercise: Moderate exercise can improve immune function, reduce stress, and enhance overall health. It is important to avoid overheating, which can trigger cholinergic urticaria.
Sleep Hygiene: Adequate and quality sleep is crucial for immune function and overall health. Developing good sleep habits can help mitigate urticaria symptoms.
Avoidance of Triggers: Identifying and avoiding known triggers, such as certain foods, medications, and environmental factors, is essential for managing urticaria.
CONCLUSION
Urticaria, commonly known as hives, is a complex condition characterized by the rapid onset of wheals, itching, and sometimes angioedema. The etiology of urticaria is diverse, encompassing physical triggers, infections, autoimmune mechanisms, medications, and idiopathic causes. Understanding these underlying factors is crucial for effective management and treatment.
The pathophysiology of urticaria involves the activation of mast cells and the release of histamine and other mediators, leading to the characteristic symptoms. The condition is classified into spontaneous and inducible forms, with further subdivisions based on triggers and clinical features. This classification aids in diagnosis, guiding the selection of appropriate therapeutic strategies.
Management of urticaria is multifaceted, requiring a combination of pharmacological treatments, lifestyle modifications, and alternative therapies. First-line treatments typically involve antihistamines, with options for escalating to more advanced therapies such as omalizumab in chronic and refractory cases. Herbal and plant-based treatments, such as aloe vera, turmeric, and holy basil, offer additional options, particularly for those seeking natural or complementary approaches.
Dietary and nutritional considerations play a significant role, especially in managing chronic urticaria. Low-histamine diets and the avoidance of known dietary triggers can alleviate symptoms. Furthermore, yoga and lifestyle changes, including stress management and regular exercise, are essential components of a holistic approach to managing the condition.
In conclusion, the management of urticaria should be tailored to the individual, taking into account the specific type of urticaria, the severity of symptoms, and the presence of any identifiable triggers. A comprehensive approach that integrates conventional and complementary therapies can significantly improve patient outcomes and quality of life. Continued research into the pathophysiology and treatment of urticaria will enhance our understanding and lead to more effective and personalized therapeutic options.
ACKNOWLEDGMENT
We would like to express our deepest gratitude to Smt. S. M. Shah Pharmacy College for their unwavering support and invaluable resources that made this article possible. The guidance, facilities, and academic environment provided by the college have been instrumental in the successful completion of this review. We extend our heartfelt thanks to the faculty, staff, and colleagues at the institution for their encouragement, insightful discussions, and assistance throughout this study. Your contributions have been integral to our efforts and achievements. Thank you for fostering a collaborative and inspiring atmosphere that has greatly enriched our work.
CONFLICT OF INTEREST
The authors declare that there are no conflicts of interest regarding the publication of this article.
REFERENCE
- Wedi B, Kapp A. Chronic urticaria: assessment of current treatment. Expert Review of Clinical Immunology. 2005;1(3).
- Virani A, Puri V, Mohd H, Michniak-Kohn B. Effect of penetration enhancers on transdermal delivery of oxcarbazepine, an antiepileptic drug using microemulsions. Pharmaceutics. 2023;15(1):183.
- mac Carthy T, Hernández Montilla I, Aguilar A, García Castro R, González Pérez AM, Vilas Sueiro A, et al. Automatic Urticaria Activity Score: Deep Learning–Based Automatic Hive Counting for Urticaria Severity Assessment. JID Innovations. 2024;4(1).
- Pedersen NH, Sørensen JA, Ghazanfar MN, Zhang DG, Vestergaard C, Thomsen SF. Biomarkers for Monitoring Treatment Response of Omalizumab in Patients with Chronic Urticaria. Vol. 24, International Journal of Molecular Sciences. 2023.
- Fernando S, Broadfoot A. Chronic urticaria: Assessment and treatment. Australian Family Physician. 2010;39(3).
- Virani A, Dholaria N, Matharoo N, Michniak-Kohn B. A study of microemulsion systems for transdermal delivery of risperidone using penetration enhancers. Journal of Pharmaceutical Sciences. 2023;112(12):3109–19.
- Jadeja M, Detholia K, Umang V, Katariya H, Patel R. Quick Prep: Human Anatomy and Physiology: Human Anatomy and Physiology: Essential Guide for National and International Entrance Exams. https://www.amazon.in/dp/B0D783LW65?ref …; 2024.
- Puri V, Savla R, Chen K, Robinson K, Virani A, Michniak-Kohn B. Antifungal nail lacquer for enhanced transungual delivery of econazole nitrate. Pharmaceutics. 2022;14(10):2204.
- Dalal I, Levine A, Somekh E, Mizrahi A, Hanukoglu A. Chronic urticaria in children: Expanding the “autoimmune kaleidoscope.” Pediatrics. 2000;106(5 I).
- Virani A. Advanced Drug Delivery With PLGA Copolymers. International Research Journal of Modernization in Engineering Technology and Science. 2024;6(4):8116–24.
- Sharma YK, Gera V, Tiwari VD. Chronic urticaria: Expanding the autoimmune kaleidoscope. Medical Journal Armed Forces India. 2004;60(4).
- Virani A, Dholaria N, Mohd H, Albayati N, Michniak-Kohn B. Effect of chemical penetration enhancers on the transdermal delivery of olanzapine in human skin in vitro. AAPS Open. 2024;10(1):4.
- R K Patel and M B Jadeja. DEVELOPMENT AND EVALUATION OF PHOSPHATIDYLCHOLINE COMPLEXES OF ARBUTIN AS SKIN WHITENING AGENT. INTERNATIONAL JOURNAL OF PHARMACEUTICAL SCIENCES AND RESEARCH. 2021;12(2):917–27.
- Patel BA. NIOSOMES: A PROMISING APPROACH FOR ADVANCED DRUG DELIVERY IN CANCER TREATMENT. International Research Journal of Modernization in Engineering Technology and Science. 2024;6(04):2747–52.
- Mohd H, Dopiera?a K, Zidar A, Virani A, Michniak-Kohn B. Effect of Edge Activator Combinations in Transethosomal Formulations for Skin Delivery of Thymoquinone via Langmuir Technique. Scientia Pharmaceutica. 2024;92(2):29.
- Staubach P, Vonend A, Burow G, Metz M, Magerl M, Maurer M. Patients with chronic urticaria exhibit increased rates of sensitisation to Candida albicans, but not to common moulds. Mycoses. 2009;52(4).
- Reeves GEM, Boyle MJ, Bonfield J, Dobson P, Loewenthal M. Impact of hydroxychloroquine therapy on chronic urticaria: Chronic autoimmune urticaria study and evaluation. Internal Medicine Journal. 2004;34(4).
- Uguz F, Engin B, Yilmaz E. Quality of life in patients with chronic idiopathic urticaria: the impact of Axis I and Axis II psychiatric disorders. General Hospital Psychiatry. 2008;30(5).
- Jadeja MB, Saluja AK, Suthar RM, Patel HK, Lad BN, Patel HM, et al. PHARMACOGNOSTICAL, PHYTOCHEMICAL AND PHARMACOLOGICAL INVESTIGATIONS OF SAMANEA SAMAN STEM. Inventi Rapid: Planta Activa. 2012;
- Kowalski ML, Woessner K, Sanak M. Approaches to the diagnosis and management of patients with a history of nonsteroidal anti-inflammatory drug-related urticaria and angioedema. Journal of Allergy and Clinical Immunology. 2015;136(2).
- Kolkhir P, Giménez-Arnau AM, Kulthanan K, Peter J, Metz M, Maurer M. Urticaria. Nature Reviews Disease Primers. 2022;8(1).
- PATEL BA, Patel MR. Pharmaceutical Preparations Of Melatonin Suitable For Intranasal Administration. US Patent US20230143212A1; 2023.
- Micheletti R, Rosenbach M. An approach to the hospitalized patient with urticaria and fever. Dermatologic Therapy. 2011;24(2).
- Erdem T. An approach to the patient of urticaria. Turk Dermatoloji Dergisi. 2014;8(3).
- Baranov AA, Namazova-Baranova LS, Il’ina NI, Kubanov AA, Araviyskaya ER, Astafieva NG, et al. Modern Approaches to the Management of Patients with Urticaria. Pediatric pharmacology. 2023;20(5).
- Patel BA. PERMEATION ENHANCEMENT AND ADVANCED STRATEGIES: A COMPREHENSIVE REVIEW OF IMPROVED TOPICAL DRUG DELIVERY. International Research Journal of Modernization in Engineering Technology and Science. 2024;6(05):6691–702.
- Deacock SJ. An approach to the patient with urticaria. Vol. 153, Clinical and Experimental Immunology. 2008.
- PATEL BA, Patel MR. Novel solution formulation of cyclophosphamide. WO Patent WO2024112860A1; 2024.


 Krunal K. Detholia* 1
Krunal K. Detholia* 1
 Mukesh B. Jadeja 2
Mukesh B. Jadeja 2
 Umang R. Varia 3
Umang R. Varia 3
 Hitesh B. Katariya 4
Hitesh B. Katariya 4
 Vidhi D. Panchal 5
Vidhi D. Panchal 5
 Vishal B. Panchal 6
Vishal B. Panchal 6
 Jay K. Prajapati 7
Jay K. Prajapati 7
 Dhaval B. Chhipa 8
Dhaval B. Chhipa 8
 10.5281/zenodo.13168909
10.5281/zenodo.13168909